Please note all prices are just for operational fees and without used supplies & devices .
Average non-surgical (medical) treatment fees for International Patients department.
| No. | Service | Price |
|---|---|---|
| 1 | General Wards (per night) | 300$ |
| 2 | Intensive Care Unit (per night) | 500$ |
| 3 | Chemothrapy per night | 100$ |
From: 1,600.00$
Embark on a transformative journey with our exceptional range of medical treatments. As a leading medical tour operator, we offer a comprehensive selection of world-class treatments and procedures to address your unique healthcare needs. From advanced surgeries to cutting-edge therapies, our team of experienced professionals is dedicated to providing top-notch care and ensuring your comfort and satisfaction. Discover a new level of healthcare excellence with our tailored treatment options. Book now to start your journey towards a healthier and happier you.
A full tummy tuck, also known as abdominoplasty, is a surgical procedure aimed at removing excess skin and fat from the abdomen while tightening the abdominal muscles. Here is an overview of the procedure:
Anesthesia: The procedure begins with the administration of anesthesia, which can be intravenous sedation or general anesthesia. Your surgeon will determine the best option for you.
Incision: A horizontally-oriented incision is made in the area between the pubic hairline and the belly button. The length and shape of the incision depend on the amount of excess skin to be removed. In some cases, a second incision around the navel may be necessary to address excess skin in the upper abdomen.
Muscle Repair: After making the incision, the surgeon accesses the abdominal muscles. Weakened or separated muscles are repaired and tightened using sutures. This step helps create a firmer abdominal profile.
Excess Skin and Fat Removal: The surgeon removes excess skin and fat from the abdomen. The remaining skin is then repositioned to create a smoother and more toned appearance.
Navel Repositioning: In some cases, the navel may need to be repositioned to maintain a natural appearance. The surgeon carefully creates a new opening for the navel and sutures it into place.
Closure: The incisions are closed using sutures, skin adhesives, tapes, or clips. Drainage tubes may be inserted to remove excess fluid or blood.
Recovery: After the procedure, you will be monitored in a recovery area. You may need to wear a compression garment to support the healing process and minimize swelling. Your surgeon will provide specific instructions for post-operative care, including medication, activity restrictions, and follow-up appointments.
A full tummy tuck (abdominoplasty) is suitable for individuals who have excess abdominal skin and fat, as well as weakened or separated abdominal muscles. It is commonly sought by individuals who have experienced significant weight loss, pregnancy, or aging, resulting in loose, sagging skin and stretched abdominal muscles.
Suitable candidates for a full tummy tuck typically meet the following criteria:
Good General Health: Candidates should be in good overall health to undergo surgery and tolerate the recovery process.
Stable Weight: It is important for candidates to have achieved a stable weight before considering a full tummy tuck. Significant fluctuations in weight after the procedure may affect the results.
Excess Abdominal Skin and Fat: Candidates should have excess skin and fat in the abdominal area that cannot be adequately addressed through diet and exercise alone.
Weakened or Separated Abdominal Muscles: Candidates with weakened or separated abdominal muscles, typically due to pregnancy or significant weight loss, can benefit from the muscle repair aspect of a full tummy tuck.
Realistic Expectations: It is crucial for candidates to have realistic expectations about the outcomes of the procedure and understand that a full tummy tuck is not a substitute for weight loss or a solution for all body contouring concerns.
A full tummy tuck (abdominoplasty) may not be suitable for everyone. While a qualified plastic surgeon is the best person to assess an individual’s candidacy, there are certain situations where a full tummy tuck may not be recommended. Here are some examples:
Poor General Health: Individuals with significant underlying health conditions that could increase the risks of surgery and anesthesia may not be suitable candidates for a full tummy tuck. This includes individuals with uncontrolled diabetes, heart disease, or certain autoimmune disorders.
Unstable Weight: Candidates who have not achieved a stable weight prior to the procedure may be advised to postpone the surgery. Significant weight fluctuations after a tummy tuck can impact the results and potentially require revision surgery.
Planning Future Pregnancies: Women who plan to have more pregnancies in the future should consider postponing a full tummy tuck. Pregnancy after the surgery can stretch the abdominal muscles and skin, potentially compromising the results.
Smoking or Nicotine Use: Smoking and nicotine use can impair healing and increase the risk of complications. Candidates who smoke or use nicotine products may be asked to quit or abstain for a specific period before and after the surgery.
Unrealistic Expectations: Individuals who have unrealistic expectations or seek a “perfect” or idealized outcome may not be suitable candidates. It is important to have a clear understanding of the limitations and potential outcomes of the procedure.
Limited Skin Laxity: Candidates with minimal excess skin or localized fat deposits may be better suited for less invasive procedures, such as liposuction or mini tummy tucks, instead of a full tummy tuck.
There are several advantages to undergoing a full tummy tuck (abdominoplasty) procedure. Here are some of the potential benefits:
Removal of Excess Skin and Fat: A full tummy tuck can effectively remove excess skin and fat from the abdominal area that may be resistant to diet and exercise. This can help achieve a flatter, more toned appearance.
Tightening of Abdominal Muscles: The procedure involves repairing and tightening the abdominal muscles that may have become weakened or separated due to factors such as pregnancy or significant weight loss. This can result in a firmer and more defined abdominal contour.
Improved Body Proportions: By removing excess skin and fat and tightening the abdominal muscles, a full tummy tuck can enhance body proportions and create a more balanced and aesthetically pleasing silhouette.
Enhanced Self-Confidence: Many individuals who undergo a full tummy tuck report an increase in self-confidence and improved body image. The procedure can help individuals feel more comfortable and satisfied with their appearance, leading to improved overall well-being.
Reduced Skin Irritation and Discomfort: Excess skin folds and hanging skin can cause skin irritation, rashes, and discomfort. A full tummy tuck can alleviate these issues by removing the excess skin and providing a smoother, more comfortable abdominal area.
Improved Posture and Core Strength: Repairing and tightening the abdominal muscles during a full tummy tuck can contribute to improved posture and core strength. This can have a positive impact on overall physical well-being and may help alleviate certain back and posture-related issues.
Complications can occur with any surgical procedure, including a full tummy tuck (abdominoplasty). It’s important to be aware of the potential risks and complications associated with the surgery. Here are some of the complications that may arise:
Poor Wound Healing: In some cases, the incision site may have difficulty healing properly, leading to delayed wound healing or wound separation. This can increase the risk of infection and may require additional treatment or revision surgery.
Infection: There is a risk of developing an infection at the surgical site. This can be managed with antibiotics, but in severe cases, it may require drainage or further intervention.
Blood Clots: Blood clots, also known as deep vein thrombosis (DVT), can form in the legs after surgery. These clots can be potentially dangerous if they travel to the lungs (pulmonary embolism). Measures such as early ambulation, compression stockings, and blood thinners may be used to minimize this risk.
Numbness or Changes in Sensation: Temporary or permanent changes in sensation, including numbness or altered sensation, may occur in the abdominal area or around the incision site. This is usually temporary but can persist in some cases.
Asymmetry: There is a possibility of unevenness or lopsidedness in the appearance of the abdomen after a tummy tuck. This can occur due to factors such as differences in healing or individual anatomical variations.
Scarring: While efforts are made to minimize scarring, a tummy tuck does result in a permanent scar. The appearance of the scar can vary depending on individual healing and surgical techniques used.
Preoperative care refers to the physical and psychosocial care provided to prepare a patient for surgery safely. It involves a series of steps and assessments to ensure the patient is in the best possible condition for the surgical procedure. While the specific preoperative care protocols may vary depending on the healthcare facility and the type of surgery, here are some general aspects of preoperative care:
Medical History and Physical Examination: A thorough medical history and physical examination are conducted to assess the patient’s overall health and identify any pre-existing conditions or risk factors that may affect the surgery or anesthesia.
Preoperative Testing: Various tests and evaluations may be performed to assess the patient’s baseline health status. These tests can include blood work, imaging studies, electrocardiogram (ECG), and other diagnostic procedures as deemed necessary.
Patient Education: Patients are provided with information about the surgical procedure, including its purpose, potential risks and benefits, expected outcomes, and post-operative care instructions. This helps patients understand what to expect and actively participate in their own care.
Medication Management: Medications that the patient is currently taking are reviewed, and any necessary adjustments or modifications are made. It is important to inform the healthcare team about all medications, including prescription drugs, over-the-counter medications, and supplements.
Preparation for Anesthesia: If the surgery requires anesthesia, the patient’s anesthesia provider will evaluate their fitness for anesthesia and discuss the anesthesia plan. This may involve fasting instructions, discontinuation of certain medications, and other specific guidelines.
Preoperative Fasting: Patients are typically instructed to refrain from eating or drinking for a specific period before the surgery. This is done to reduce the risk of aspiration during anesthesia.
Preoperative Skin Preparation: The surgical site may need to be prepared by cleansing the skin with an antiseptic solution to reduce the risk of infection.
Consent and Documentation: Informed consent is obtained from the patient or their legal representative after discussing the risks, benefits, and alternatives of the procedure. All necessary consent forms and documentation are completed.
Postoperative care refers to the care and management provided to patients immediately following a surgical procedure. The goal of postoperative care is to ensure the patient’s safety, promote healing, manage pain, and facilitate a smooth recovery. While the specific postoperative care protocols may vary depending on the type of surgery and individual patient needs, here are some general aspects of postoperative care:
Monitoring Vital Signs: The patient’s vital signs, including heart rate, blood pressure, respiratory rate, and oxygen saturation, are closely monitored in the immediate postoperative period. This helps identify any signs of complications or changes in the patient’s condition.
Pain Management: Adequate pain relief is essential for patient comfort and to facilitate recovery. Pain medications, both oral and intravenous, may be prescribed and administered as needed. Non-pharmacological pain management techniques, such as ice packs or positioning, may also be utilized.
Wound Care: The surgical incision site is carefully monitored for signs of infection or complications. Dressings may be changed as needed, and proper hygiene practices are followed to minimize the risk of infection. Specific wound care instructions are provided to the patient and their caregivers.
Mobility and Ambulation: Early mobilization and ambulation are encouraged to promote blood circulation, prevent complications such as blood clots, and aid in the recovery process. Physical therapy or occupational therapy may be involved in guiding the patient’s movement and rehabilitation.
Fluid and Nutrition Management: Adequate hydration and nutrition are important for the healing process. Intravenous fluids may be administered initially, followed by a transition to oral intake as tolerated. Dietary instructions, including any restrictions or modifications, are provided to the patient.
Medication Management: Patients may be prescribed various medications postoperatively, including pain medications, antibiotics, and prophylactic medications to prevent complications such as blood clots. Medication instructions, dosage, and timing are provided to the patient.
Respiratory Care: Depending on the type of surgery and anesthesia, patients may require specific respiratory care, such as deep breathing exercises, incentive spirometry, or the use of respiratory devices to prevent respiratory complications and aid in lung expansion.
Emotional and Psychosocial Support: Postoperative care also involves providing emotional support to patients and addressing any psychosocial needs they may have. This can include providing information about the recovery process, addressing concerns or anxieties, and involving the patient’s support system in their care.
Only logged in customers who have purchased this product may leave a review.


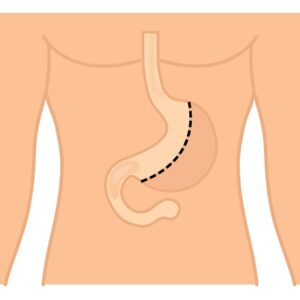
A full tummy tuck, also known as abdominoplasty, is a surgical procedure aimed at removing excess skin and fat from the abdomen while tightening the abdominal muscles. Here is an overview of the procedure:
Anesthesia: The procedure begins with the administration of anesthesia, which can be intravenous sedation or general anesthesia. Your surgeon will determine the best option for you.
Incision: A horizontally-oriented incision is made in the area between the pubic hairline and the belly button. The length and shape of the incision depend on the amount of excess skin to be removed. In some cases, a second incision around the navel may be necessary to address excess skin in the upper abdomen.
Muscle Repair: After making the incision, the surgeon accesses the abdominal muscles. Weakened or separated muscles are repaired and tightened using sutures. This step helps create a firmer abdominal profile.
Excess Skin and Fat Removal: The surgeon removes excess skin and fat from the abdomen. The remaining skin is then repositioned to create a smoother and more toned appearance.
Navel Repositioning: In some cases, the navel may need to be repositioned to maintain a natural appearance. The surgeon carefully creates a new opening for the navel and sutures it into place.
Closure: The incisions are closed using sutures, skin adhesives, tapes, or clips. Drainage tubes may be inserted to remove excess fluid or blood.
Recovery: After the procedure, you will be monitored in a recovery area. You may need to wear a compression garment to support the healing process and minimize swelling. Your surgeon will provide specific instructions for post-operative care, including medication, activity restrictions, and follow-up appointments.
A full tummy tuck (abdominoplasty) is suitable for individuals who have excess abdominal skin and fat, as well as weakened or separated abdominal muscles. It is commonly sought by individuals who have experienced significant weight loss, pregnancy, or aging, resulting in loose, sagging skin and stretched abdominal muscles.
Suitable candidates for a full tummy tuck typically meet the following criteria:
Good General Health: Candidates should be in good overall health to undergo surgery and tolerate the recovery process.
Stable Weight: It is important for candidates to have achieved a stable weight before considering a full tummy tuck. Significant fluctuations in weight after the procedure may affect the results.
Excess Abdominal Skin and Fat: Candidates should have excess skin and fat in the abdominal area that cannot be adequately addressed through diet and exercise alone.
Weakened or Separated Abdominal Muscles: Candidates with weakened or separated abdominal muscles, typically due to pregnancy or significant weight loss, can benefit from the muscle repair aspect of a full tummy tuck.
Realistic Expectations: It is crucial for candidates to have realistic expectations about the outcomes of the procedure and understand that a full tummy tuck is not a substitute for weight loss or a solution for all body contouring concerns.
A full tummy tuck (abdominoplasty) may not be suitable for everyone. While a qualified plastic surgeon is the best person to assess an individual’s candidacy, there are certain situations where a full tummy tuck may not be recommended. Here are some examples:
Poor General Health: Individuals with significant underlying health conditions that could increase the risks of surgery and anesthesia may not be suitable candidates for a full tummy tuck. This includes individuals with uncontrolled diabetes, heart disease, or certain autoimmune disorders.
Unstable Weight: Candidates who have not achieved a stable weight prior to the procedure may be advised to postpone the surgery. Significant weight fluctuations after a tummy tuck can impact the results and potentially require revision surgery.
Planning Future Pregnancies: Women who plan to have more pregnancies in the future should consider postponing a full tummy tuck. Pregnancy after the surgery can stretch the abdominal muscles and skin, potentially compromising the results.
Smoking or Nicotine Use: Smoking and nicotine use can impair healing and increase the risk of complications. Candidates who smoke or use nicotine products may be asked to quit or abstain for a specific period before and after the surgery.
Unrealistic Expectations: Individuals who have unrealistic expectations or seek a “perfect” or idealized outcome may not be suitable candidates. It is important to have a clear understanding of the limitations and potential outcomes of the procedure.
Limited Skin Laxity: Candidates with minimal excess skin or localized fat deposits may be better suited for less invasive procedures, such as liposuction or mini tummy tucks, instead of a full tummy tuck.
There are several advantages to undergoing a full tummy tuck (abdominoplasty) procedure. Here are some of the potential benefits:
Removal of Excess Skin and Fat: A full tummy tuck can effectively remove excess skin and fat from the abdominal area that may be resistant to diet and exercise. This can help achieve a flatter, more toned appearance.
Tightening of Abdominal Muscles: The procedure involves repairing and tightening the abdominal muscles that may have become weakened or separated due to factors such as pregnancy or significant weight loss. This can result in a firmer and more defined abdominal contour.
Improved Body Proportions: By removing excess skin and fat and tightening the abdominal muscles, a full tummy tuck can enhance body proportions and create a more balanced and aesthetically pleasing silhouette.
Enhanced Self-Confidence: Many individuals who undergo a full tummy tuck report an increase in self-confidence and improved body image. The procedure can help individuals feel more comfortable and satisfied with their appearance, leading to improved overall well-being.
Reduced Skin Irritation and Discomfort: Excess skin folds and hanging skin can cause skin irritation, rashes, and discomfort. A full tummy tuck can alleviate these issues by removing the excess skin and providing a smoother, more comfortable abdominal area.
Improved Posture and Core Strength: Repairing and tightening the abdominal muscles during a full tummy tuck can contribute to improved posture and core strength. This can have a positive impact on overall physical well-being and may help alleviate certain back and posture-related issues.
Complications can occur with any surgical procedure, including a full tummy tuck (abdominoplasty). It’s important to be aware of the potential risks and complications associated with the surgery. Here are some of the complications that may arise:
Poor Wound Healing: In some cases, the incision site may have difficulty healing properly, leading to delayed wound healing or wound separation. This can increase the risk of infection and may require additional treatment or revision surgery.
Infection: There is a risk of developing an infection at the surgical site. This can be managed with antibiotics, but in severe cases, it may require drainage or further intervention.
Blood Clots: Blood clots, also known as deep vein thrombosis (DVT), can form in the legs after surgery. These clots can be potentially dangerous if they travel to the lungs (pulmonary embolism). Measures such as early ambulation, compression stockings, and blood thinners may be used to minimize this risk.
Numbness or Changes in Sensation: Temporary or permanent changes in sensation, including numbness or altered sensation, may occur in the abdominal area or around the incision site. This is usually temporary but can persist in some cases.
Asymmetry: There is a possibility of unevenness or lopsidedness in the appearance of the abdomen after a tummy tuck. This can occur due to factors such as differences in healing or individual anatomical variations.
Scarring: While efforts are made to minimize scarring, a tummy tuck does result in a permanent scar. The appearance of the scar can vary depending on individual healing and surgical techniques used.
Preoperative care refers to the physical and psychosocial care provided to prepare a patient for surgery safely. It involves a series of steps and assessments to ensure the patient is in the best possible condition for the surgical procedure. While the specific preoperative care protocols may vary depending on the healthcare facility and the type of surgery, here are some general aspects of preoperative care:
Medical History and Physical Examination: A thorough medical history and physical examination are conducted to assess the patient’s overall health and identify any pre-existing conditions or risk factors that may affect the surgery or anesthesia.
Preoperative Testing: Various tests and evaluations may be performed to assess the patient’s baseline health status. These tests can include blood work, imaging studies, electrocardiogram (ECG), and other diagnostic procedures as deemed necessary.
Patient Education: Patients are provided with information about the surgical procedure, including its purpose, potential risks and benefits, expected outcomes, and post-operative care instructions. This helps patients understand what to expect and actively participate in their own care.
Medication Management: Medications that the patient is currently taking are reviewed, and any necessary adjustments or modifications are made. It is important to inform the healthcare team about all medications, including prescription drugs, over-the-counter medications, and supplements.
Preparation for Anesthesia: If the surgery requires anesthesia, the patient’s anesthesia provider will evaluate their fitness for anesthesia and discuss the anesthesia plan. This may involve fasting instructions, discontinuation of certain medications, and other specific guidelines.
Preoperative Fasting: Patients are typically instructed to refrain from eating or drinking for a specific period before the surgery. This is done to reduce the risk of aspiration during anesthesia.
Preoperative Skin Preparation: The surgical site may need to be prepared by cleansing the skin with an antiseptic solution to reduce the risk of infection.
Consent and Documentation: Informed consent is obtained from the patient or their legal representative after discussing the risks, benefits, and alternatives of the procedure. All necessary consent forms and documentation are completed.
Postoperative care refers to the care and management provided to patients immediately following a surgical procedure. The goal of postoperative care is to ensure the patient’s safety, promote healing, manage pain, and facilitate a smooth recovery. While the specific postoperative care protocols may vary depending on the type of surgery and individual patient needs, here are some general aspects of postoperative care:
Monitoring Vital Signs: The patient’s vital signs, including heart rate, blood pressure, respiratory rate, and oxygen saturation, are closely monitored in the immediate postoperative period. This helps identify any signs of complications or changes in the patient’s condition.
Pain Management: Adequate pain relief is essential for patient comfort and to facilitate recovery. Pain medications, both oral and intravenous, may be prescribed and administered as needed. Non-pharmacological pain management techniques, such as ice packs or positioning, may also be utilized.
Wound Care: The surgical incision site is carefully monitored for signs of infection or complications. Dressings may be changed as needed, and proper hygiene practices are followed to minimize the risk of infection. Specific wound care instructions are provided to the patient and their caregivers.
Mobility and Ambulation: Early mobilization and ambulation are encouraged to promote blood circulation, prevent complications such as blood clots, and aid in the recovery process. Physical therapy or occupational therapy may be involved in guiding the patient’s movement and rehabilitation.
Fluid and Nutrition Management: Adequate hydration and nutrition are important for the healing process. Intravenous fluids may be administered initially, followed by a transition to oral intake as tolerated. Dietary instructions, including any restrictions or modifications, are provided to the patient.
Medication Management: Patients may be prescribed various medications postoperatively, including pain medications, antibiotics, and prophylactic medications to prevent complications such as blood clots. Medication instructions, dosage, and timing are provided to the patient.
Respiratory Care: Depending on the type of surgery and anesthesia, patients may require specific respiratory care, such as deep breathing exercises, incentive spirometry, or the use of respiratory devices to prevent respiratory complications and aid in lung expansion.
Emotional and Psychosocial Support: Postoperative care also involves providing emotional support to patients and addressing any psychosocial needs they may have. This can include providing information about the recovery process, addressing concerns or anxieties, and involving the patient’s support system in their care.
There are no reviews yet.
Only logged in customers who have purchased this product may leave a review.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment. The preferred choice for many patients is choosing private care.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment.
Reviews
There are no reviews yet.