Receiving a cancer diagnosis is a life-altering moment, filled with uncertainty and questions. However, the landscape of oncology is evolving faster than ever before. The treatments available in 2025 offer more hope, precision, and personalized options than at any point in history. Understanding these different approaches is the first step toward empowerment and making informed decisions about your health journey.
From the foundational pillars of surgery and chemotherapy to the revolutionary impact of immunotherapy and AI-driven diagnostics, the options are expanding. This guide will walk you through the various kinds of cancer treatments, explaining how they work, who they are for, and what the future holds. Consequently, you will be better equipped to discuss your path forward with your medical team.
For decades, a few core methods have formed the backbone of cancer treatment. While newer therapies are emerging, these established techniques remain highly effective and are often used in combination to achieve the best outcomes.
Surgery is often the primary treatment for solid tumors that are contained in one area. The primary goal of surgical oncology is to physically remove the cancerous mass, along with a small margin of healthy tissue to ensure all cancer cells are taken out. For early-stage cancers, surgery alone can sometimes be curative. Moreover, it plays a crucial role in diagnosing and staging cancer through biopsies.
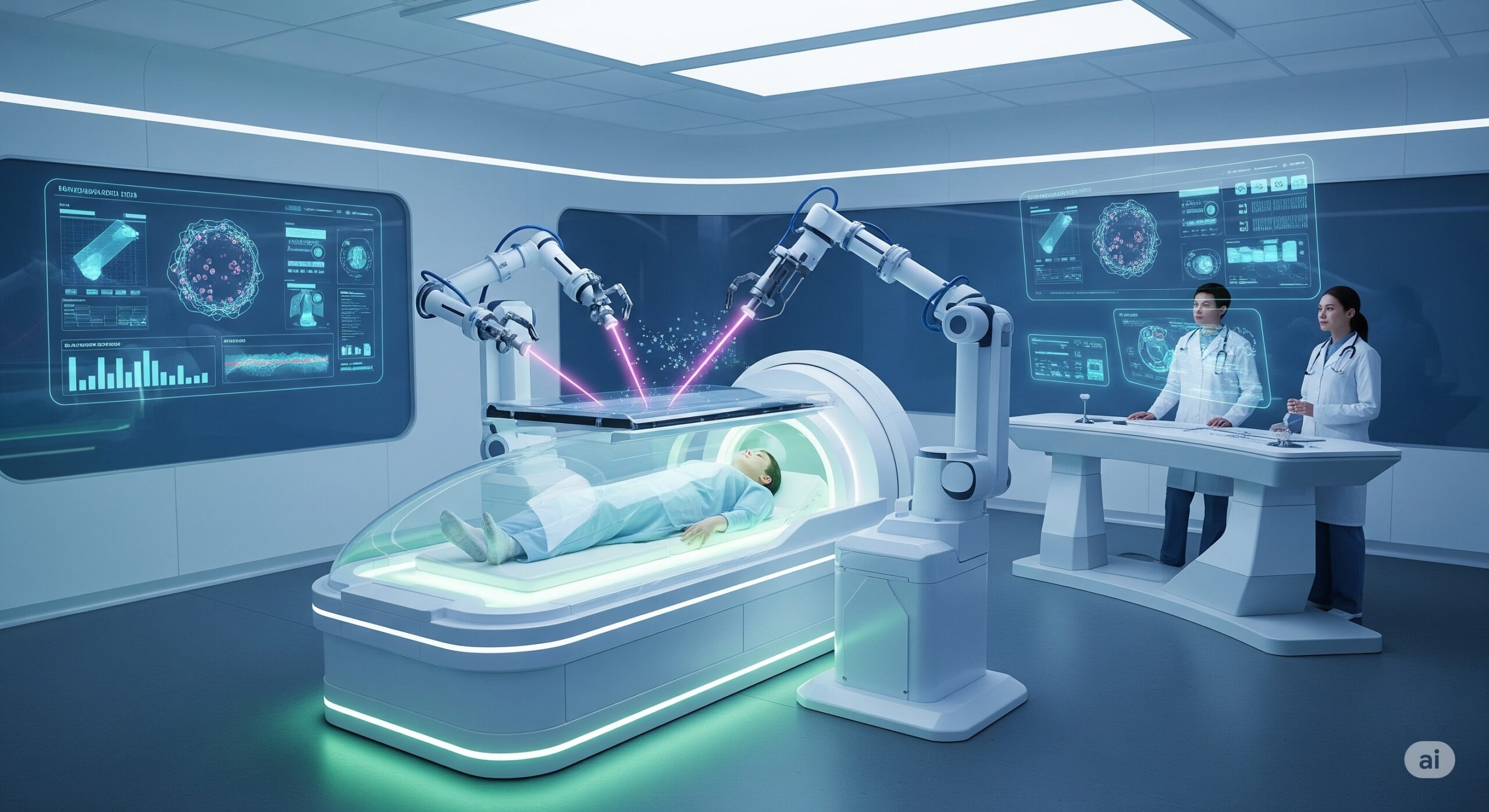
Advances in surgical techniques, such as minimally invasive laparoscopic and robotic-assisted surgeries, have significantly reduced recovery times, minimized scarring, and lowered the risk of complications. Surgeons can now operate with greater precision than ever, preserving healthy organs and functions. For more information on surgical options, exploring a dedicated oncology department can provide valuable insights.
Radiation therapy uses high-energy particles or waves, such as X-rays or protons, to damage the DNA of cancer cells, destroying their ability to multiply. According to the National Cancer Institute, more than half of all cancer patients receive some form of radiation therapy. It can be used to shrink a tumor before surgery, eliminate any remaining cancer cells after surgery, or as the main treatment.
Modern radiotherapy techniques like Intensity-Modulated Radiation Therapy (IMRT) and Stereotactic Body Radiation Therapy (SBRT) allow doctors to shape the radiation beams precisely to the tumor, sparing the surrounding healthy tissue. This targeted approach enhances effectiveness while reducing side effects. For a deeper look, see this article on the mechanisms of radiation therapy.
Chemotherapy involves using powerful drugs to kill fast-growing cells throughout the body, making it a systemic treatment for cancer that has spread (metastatic). It can be administered intravenously (IV) or orally. While it is highly effective, its non-specific nature means it can also damage healthy, fast-growing cells like those in the hair follicles, bone marrow, and digestive tract, leading to well-known side effects.
Fortunately, supportive care has improved dramatically. Today, treatments to manage side effects like nausea and fatigue are much more effective, improving patients’ quality of life during chemotherapy. In addition, oncologists are becoming more adept at tailoring chemotherapy regimens to individual patient needs.
The one-size-fits-all approach to cancer is fading. The modern era of oncology focuses on the specific genetic and molecular characteristics of a patient’s tumor. This personalized strategy leads to more effective treatments with fewer side effects.
Unlike chemotherapy, targeted therapy drugs are designed to interfere with specific molecules (molecular targets) that are involved in the growth, progression, and spread of cancer. Because these drugs focus on what makes cancer cells different from normal cells, they are often less harmful to healthy cells.
For this treatment to be effective, a patient’s tumor must have the specific molecular target that the drug is designed for. Therefore, genetic testing of the tumor is a critical first step. An excellent resource for understanding this is the American Cancer Society’s page on targeted therapy.
Immunotherapy represents one of the most significant breakthroughs in cancer treatment in the last decade. Instead of attacking the cancer directly, it harnesses the power of the patient’s own immune system to find and destroy cancer cells. Cancer cells often develop ways to hide from the immune system, and immunotherapy drugs essentially remove this “disguise.”
Checkpoint inhibitors are the most common type of immunotherapy. They block proteins that stop the immune system from attacking cancer cells. This therapy has produced long-lasting remissions in patients with advanced cancers, such as melanoma and lung cancer, that were previously very difficult to treat. You can learn more about immunotherapy options by visiting our dedicated page.
Some cancers, particularly breast and prostate cancers, rely on hormones to grow. Hormone therapy works by blocking the body’s ability to produce these hormones or by interfering with how hormones affect cancer cells. This approach is highly effective for hormone-receptor-positive cancers.
For example, drugs like Tamoxifen are used for estrogen receptor-positive breast cancer, while androgen deprivation therapy is a cornerstone of treating advanced prostate cancer. This treatment is often less toxic than chemotherapy and can be used for many years to control cancer growth.
The field of oncology is on the cusp of another major leap forward. Driven by technology and a deeper understanding of cancer biology, these emerging treatments are set to redefine cancer care.
CAR T-cell therapy is a revolutionary form of immunotherapy where a patient’s own T-cells (a type of immune cell) are collected, genetically re-engineered in a lab to produce chimeric antigen receptors (CARs), and then infused back into the patient. These newly armed CAR T-cells are “living drugs” that can seek out and kill cancer cells with incredible precision. It has shown remarkable success in treating blood cancers like leukemia and lymphoma, and research is underway to adapt it for solid tumors. For more details on this innovative treatment, refer to the Mayo Clinic’s guide to CAR T-cell therapy.
Artificial intelligence (AI) is rapidly changing how cancer is diagnosed and treated. AI algorithms can analyze medical images like CT scans and mammograms with a level of detail that can surpass the human eye, detecting cancer earlier and more accurately. Furthermore, AI can analyze vast amounts of genetic data to predict which treatments will be most effective for a specific patient, truly personalizing medicine. This integration of technology promises a future of proactive and highly tailored global cancer care.
Building on the success of mRNA COVID-19 vaccines, researchers are developing therapeutic cancer vaccines. These don’t prevent cancer but rather treat it by stimulating the immune system to attack tumors. Each vaccine can be personalized to a patient’s specific tumor mutations, creating a highly targeted immune response. Major clinical trials are showing promising results, and this could become a standard treatment within the next few years.
| Treatment Type | How It Works | Best For | Key Advantage |
|---|---|---|---|
| Surgery | Physically removes the tumor. | Solid, localized tumors (e.g., early-stage breast, colon). | Can be curative on its own. |
| Radiation Therapy | Uses high-energy rays to kill cancer cells. | Local control of tumors, often used with other treatments. | Highly targeted, spares healthy tissue. |
| Chemotherapy | Systemic drugs that kill fast-growing cells. | Metastatic (widespread) cancer. | Treats the entire body. |
| Targeted Therapy | Drugs that block specific molecules involved in cancer growth. | Cancers with specific genetic mutations (e.g., lung, melanoma). | Fewer side effects than chemo. |
| Immunotherapy | Boosts the body’s own immune system to fight cancer. | Various cancers, including melanoma, lung, and bladder cancer. | Can result in long-term remission. |
| CAR T-Cell Therapy | Genetically engineered patient T-cells attack cancer. | Blood cancers (leukemia, lymphoma). | A “living drug” with lasting effects. |
Navigating these complex options can be overwhelming. The best treatment plan is unique to you and depends on your cancer type, its stage, your overall health, and your personal preferences. This is where a multidisciplinary team of oncologists is essential.
At WMedTour, we connect you with world-class hospitals and specialists, including those in leading medical tourism destinations like Turkey and Iran. We help you access these advanced treatments, often at a more affordable cost, without compromising on quality. Our role is to simplify the process, from initial consultations and medical record transfers to travel logistics and post-treatment care.
Your journey to recovery begins with having the right information and the right partners. We are here to ensure you have access to the best care the world has to offer.