💆 Cystocele: A Complete Guide to Understanding, Treating, and Preventing Fallen Bladder – WMedTour
Executive Summary
This comprehensive guide details everything you need to know about a **Cystocele**, commonly called a “fallen bladder.” This condition, where the bladder bulges into the vagina due to weakened pelvic floor support, affects millions of women but is highly treatable. Essentially, understanding the different grades—from mild (Grade 1) to severe (Grade 3)—is the first crucial step toward effective management. We delve into both conservative methods, like pelvic floor physical therapy and pessaries, and definitive surgical solutions, such as anterior colporrhaphy.
For those considering specialized care, especially complex surgical repair, medical tourism presents an attractive avenue for accessing world-class experts and advanced facilities at a better value. Therefore, we emphasize that regaining comfort and urinary control is absolutely achievable through informed treatment choices. Furthermore, maintaining a healthy lifestyle is key to long-term prevention.
💙 Understanding Cystocele: What is a Fallen Bladder?
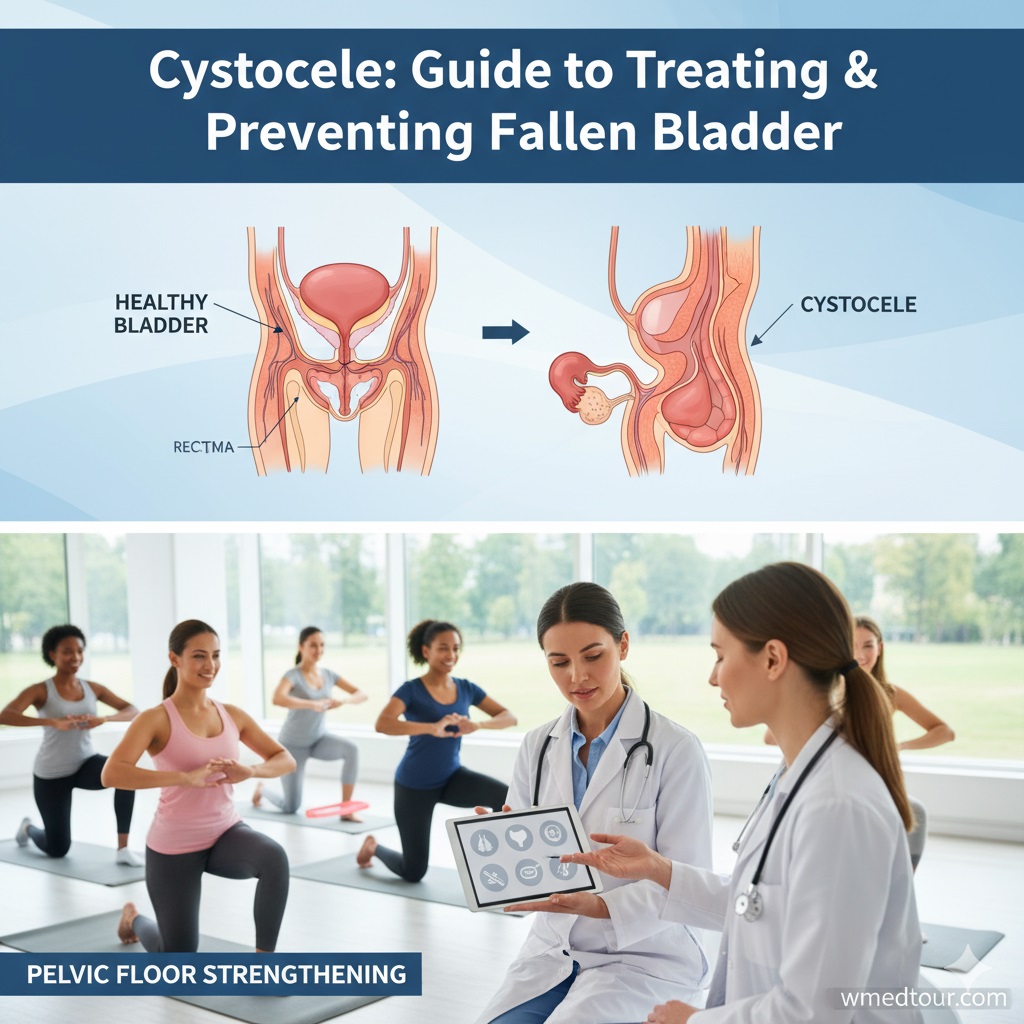
The term **Cystocele** might sound clinical, but it simply describes a common condition where the tough, supportive tissue separating the bladder and the vagina tears or weakens. Consequently, the bladder descends and bulges into the vaginal space. This is a type of **Pelvic Organ Prolapse (POP)**. The pelvic floor muscles, which act like a hammock, can weaken over time, allowing the bladder to literally “fall” or prolapse.
Causes and Key Risk Factors
The underlying cause is usually excessive pressure or damage to the pelvic floor. It’s important to realize that several factors significantly increase the risk. Firstly, vaginal childbirth, especially multiple or difficult deliveries, stretches and damages the supporting fascia. Secondly, chronic straining, such as from long-term constipation, chronic coughing (like from smoking or asthma), or heavy lifting, exerts downward pressure. Moreover, aging and menopause lead to a reduction in estrogen, which weakens the connective tissues across the entire body, including the pelvis. Finally, genetic factors can predispose some women to weaker connective tissue.
The Grading System: How Severity is Measured
Doctors classify the severity of a **Cystocele** using a grading system, which directly influences the recommended treatment plan. Knowing your grade is vital for making an informed decision about your care:
- ① **Grade 1 (Mild):** The bladder barely drops into the vagina. Symptoms may be minimal or non-existent.
- ② **Grade 2 (Moderate):** The bladder descends far enough to reach the opening of the vagina. Patients usually feel a distinct bulge or pressure. This is where most symptomatic women present for gynecological surgery assessment.
- ③ **Grade 3 (Severe):** The bladder actually bulges outside the vaginal opening. This severe **Cystocele** grade often requires surgical intervention for functional restoration.
☦ Symptoms and Recognizing the Need for Care
Symptoms of a **Cystocele** are primarily related to the bulging mass and disruption of normal urinary function. Therefore, recognizing these signs early can prevent progression and lead to faster relief. Often, the symptoms worsen during the day and are alleviated when lying down.
Key Symptom Categories
- **Vaginal/Pelvic Discomfort:** A feeling of fullness, heaviness, or pressure in the pelvis, often described as “sitting on a ball.” Patients may feel or see a soft lump or bulge in the vagina.
- **Urinary Issues:** This is the most common and disruptive group of symptoms. It includes urinary frequency, urgency, incomplete emptying of the bladder (leading to a feeling of needing to strain), and, conversely, **stress urinary incontinence (SUI)**, which is leakage when coughing, laughing, or exercising. For the more challenging cases involving SUI, detailed evaluations like Urodynamics are necessary.
- **Sexual Problems (Dyspareunia):** Discomfort or pain during intercourse can occur due to the tissue displacement.
The transition from mild discomfort to functional impairment is the clear signal to seek professional help. Indeed, waiting only prolongs the issue, particularly when considering surgical options for long-term correction. You can also explore our comprehensive checkup department to ensure early detection of any gynecological issues.
🔍 Diagnosing Cystocele: The Medical Process
Diagnosis begins with a thorough medical history, focusing on childbirth, urinary function, and any straining activities. Following this, the physician performs a pelvic examination.
Key Diagnostic Tools
- **Pelvic Examination:** The doctor examines the vagina and pelvis while the patient is asked to bear down (Valsalva maneuver) to assess the degree of prolapse. This determines the grading.
- **Urine Culture:** This test rules out a urinary tract infection (UTI), as UTI symptoms can sometimes mimic prolapse symptoms.
- **Urodynamic Testing:** This suite of tests measures how well the bladder and urethra are storing and releasing urine. It is vital for planning treatment, as it determines if the prolapse is masking underlying incontinence. Furthermore, it helps the surgeon understand the full picture before considering urinary incontinence surgery alongside **Cystocele** repair.
- **Intravenous Pyelogram (IVP) or Renal Ultrasound:** These imaging tests are reserved for severe cases to ensure the prolapse is not obstructing the ureters and affecting kidney function.
- ✓ Zero invasiveness and cost-effective.
- ✓ Can improve sexual sensation and control.
- ✓ Effective for prevention and mild symptoms.
- ❌ Requires significant dedication and consistency.
- ❌ Limited effectiveness for Grade 3 or severe prolapse.
- ❌ Easy to perform incorrectly without biofeedback.
- ✓ Immediate symptom relief upon insertion.
- ✓ Non-surgical and reversible.
- ✓ Can be used by patients with high surgical risk.
- ❌ Requires regular cleaning and maintenance.
- ❌ Potential for vaginal discharge or irritation.
- ❌ May interfere with sexual activity for some users.
- ✓ Definitive, long-lasting correction for severe prolapse.
- ✓ Significant or complete elimination of bulge and pressure symptoms.
- ✓ Often performed through a minimally invasive vaginal approach (no abdominal incision).
- ❌ Recovery time of several weeks (avoiding lifting).
- ❌ Potential for surgical complications (infection, bleeding).
- ❌ Risk of recurrence or developing incontinence afterward.
- **The Newly Diagnosed Patient:** If you’ve just received a **Cystocele** diagnosis (especially Grade 1 or 2) and are exploring non-surgical and surgical options.
- **The Frustrated Patient:** If you’ve tried pelvic floor exercises or lifestyle changes without satisfactory results and are now seriously considering surgery.
- **The Medical Tourist Candidate:** If you are seeking specialized, timely, or cost-effective **Cystocele** repair surgery from an internationally recognized expert. You can see how our doctors are vetted by checking our Checklist for Choosing a Surgeon/Clinic Abroad.
- **Healthcare Professionals and Caregivers:** Those who need to quickly grasp the core concepts, modern treatments, and patient experience pathways for this common pelvic floor disorder.
- **Maintain a Healthy Weight:** Excess abdominal fat puts constant, undue pressure on the pelvic floor. Maintaining a healthy BMI is one of the most effective preventive measures.
- **Avoid Chronic Straining:** This means managing chronic constipation (ensure adequate fiber and fluid intake, as detailed in this medical tourism guide), and seeking treatment for any chronic cough.
- **Lift Safely:** When lifting heavy objects—a child, a box, or weights—always engage the core and pelvic floor muscles. Never hold your breath and strain.
- **Consistent Pelvic Floor Maintenance:** Even after surgery, regularly performing Kegel exercises helps maintain muscle tone and support.
Consequently, accurate diagnosis is the foundation of a successful treatment plan.
🚫 Non-Surgical Management Strategies
Non-surgical treatments are the first line of defense, especially for Grade 1 and many Grade 2 **Cystocele** cases, or for patients who wish to defer surgery. Generally speaking, these options focus on strengthening the support structure and alleviating symptoms.
Pelvic Floor Muscle Training (Kegels)
Targeted exercises, known as Kegels, aim to strengthen the muscles that form the pelvic floor. Consistent practice can improve symptoms of mild prolapse and incontinence. However, proper technique is critical; physical therapy with a specialist often yields the best results.
Pros of Kegels
Cons of Kegels
Pessary Insertion
A pessary is a medical device, usually made of silicone, inserted into the vagina to physically support the prolapsed bladder. This is a highly effective, low-risk option. Furthermore, it can be a temporary solution while awaiting surgery or a permanent option for women who are not candidates for an operation.
Pros of Pessary
Cons of Pessary
Lifestyle Modifications
Simple changes dramatically impact the pelvic floor. Losing excess weight significantly reduces pressure. Managing chronic cough and avoiding heavy lifting (or using proper form) are also essential. Because constipation is a major contributor, increasing dietary fiber and hydration is critical. You can learn more about general surgery options that may also be related to weight management on our bariatric surgery page.
⚗ Surgical Repair Options
Surgery becomes the definitive solution for Grade 3 **Cystocele**, or for patients with Grade 2 prolapse where non-surgical methods have failed or symptoms are significantly impacting quality of life. The goal of surgery is to push the bladder back into its correct position and repair the weakened fascia that supports it. This procedure is called anterior colporrhaphy, or “anterior repair.”
Anterior Colporrhaphy (Cystocele Repair)
This is the most common surgical procedure. The surgeon typically accesses the repair site through the vagina (vaginal approach). They make an incision in the anterior (front) wall of the vagina, push the bladder back, tighten the fascia between the bladder and vagina, and then stitch the vaginal wall closed. In short, this restores the normal anatomy.
Using Surgical Mesh vs. Native Tissue Repair
Historically, surgeons used synthetic mesh to reinforce the repair, especially in recurrent or severe cases. However, mesh usage has become highly controversial due to potential complications. Therefore, the current standard approach prioritizes **native tissue repair**, using the patient’s own strong fascia, unless the risk of recurrence is exceptionally high. You must discuss the benefits and risks of mesh carefully with your surgeon.
Pros of Surgery
Cons of Surgery
For patients facing complex pelvic issues, surgeons often utilize advanced techniques, which you can read about in our Robotic-Assisted Urological Surgery guide. Additionally, post-operative care is crucial; recovery involves strictly avoiding heavy lifting for at least six weeks.
📋 Choosing the Right Path: Comparison of Treatment Options
The decision between non-surgical and surgical intervention depends on several factors: the grade of the **Cystocele**, the severity of symptoms, the patient’s age and overall health, and whether they plan to have more children. Consequently, a detailed consultation with a urogynecologist is indispensable.
| Treatment Option | Best For | Time to Relief | Invasiveness | Recurrence Risk |
|---|---|---|---|---|
| Pelvic Floor Training (Kegels) | Grade 1, Prevention | Months (Gradual) | None | High (if not maintained) |
| Pessary | Grade 1 or 2, Surgical Ineligibility | Immediate | Minimal (Insertion/Maintenance) | N/A (Symptom Management) |
| Anterior Colporrhaphy (Surgery) | Grade 3, Symptomatic Grade 2, Recurrence | Weeks (After Healing) | High (Invasive) | Low to Moderate (Expert dependent) |
👩⚕️ Case Study: Elena’s Journey to Relief
Elena’s Battle with a Moderate Cystocele
Elena, a 55-year-old high school teacher from Toronto, had three natural childbirths and loved gardening. Over the last five years, she experienced a worsening feeling of pelvic pressure and often had to double-void her bladder. Her symptoms, especially the feeling of a bulge, were disruptive, causing her to limit her physical activity, including her beloved gardening. Following a routine checkup, her physician diagnosed her with a Grade 2 **Cystocele**.
Initially, Elena tried six months of pelvic floor physical therapy. While her urinary urgency slightly improved, the feeling of pressure and the physical bulge remained bothersome. Because she wanted a permanent solution and struggled with the long wait times for specialized surgery at home, she began researching medical tourism. She decided to pursue anterior colporrhaphy abroad.
WMedTour connected her with a highly experienced urogynecologist in a top international center. After a successful native tissue repair, Elena followed her recovery instructions rigorously, and three months later, she reported complete resolution of the pressure and bulge. She is now back to lifting light garden pots and is planning a post-recovery celebratory trip, confident that her **Cystocele** is finally behind her. This case illustrates the vital role of specialized surgical expertise when conservative treatments fall short.
🌐 Cystocele and Medical Tourism: A Viable Solution
For many patients, especially those requiring complex reconstructive surgery for a severe **Cystocele**, medical tourism offers compelling advantages. The confluence of long wait times in many Western countries and the high cost of private domestic care makes seeking treatment abroad a logical and often superior choice. By carefully vetting top-tier surgeons and accredited facilities—a service we specialize in at WMedTour—patients can access high-quality care.
The procedures, such as advanced laparoscopic or robotic-assisted anterior repairs, are often performed by surgeons specializing exclusively in pelvic reconstructive surgery, ensuring optimal outcomes. Furthermore, the overall cost, including travel and accommodation, is often significantly less than the cost of the surgery alone in countries like the US or UK. We provide comprehensive guides for patients considering options in various regions, such as the Ultimate Guide to Medical Travel in Iran or the Ultimate Guide to Medical Travel in Turkey, where such specialized procedures are readily available.
It is important, however, to follow specific guidelines for safe and effective medical travel. Reviewing our pre-travel checklist for gynecological surgery is a vital step. You must also understand the global medical treatment regulations guide for the destination you choose. While the quality of surgical care can be world-class, thorough planning is paramount to a smooth journey and recovery.
👤 Who is This For?
This guide on **Cystocele** is explicitly designed for a few key audiences:
💪 Preventing Recurrence and Long-Term Wellness
Surgical repair for **Cystocele** is highly effective, yet the key to long-term success lies in preventing the issue from returning. Furthermore, the same factors that caused the initial prolapse can cause a recurrence.
Strategies for Long-Term Pelvic Health
Always remember that post-operative recovery involves a structured return to activity. This ensures the repair site has enough time to heal fully. You must follow all prescribed post-op protocols from your surgeon and avoid intense activities until cleared. For those who travel for surgery, a well-planned recovery period in the host country is beneficial before returning home, often facilitated by your medical tourism provider.
📝 Authoritative Insights & Credibility
To ensure this guide provides the most current and authoritative information, we synthesize knowledge from global urogynecology consensus. Research from institutions like the National Institute of Child Health and Human Development highlights the multi-factorial nature of pelvic floor disorders and the importance of personalized, multi-modal treatment approaches. Additionally, studies published in the American Journal of Obstetrics and Gynecology (AJOG) consistently reaffirm native tissue repair as the gold standard for most anterior prolapse repairs.
This authoritative grounding ensures that the advice provided is evidence-based and aligned with current medical standards, especially when considering complex procedures. For those considering surgical options, researching top-tier specialists who align with these global standards is the most important step. Consider reviewing our doctors directory to find accredited surgeons.
❓ FAQ: Your Most Pressing Questions Answered
1. Can a Cystocele heal on its own without intervention?
A mild Grade 1 **Cystocele** will not typically “heal” completely on its own, but its symptoms can be significantly managed or reduced with dedicated non-surgical methods like pelvic floor muscle training and lifestyle modifications. Moderate or severe prolapse (Grade 2 or 3) requires intervention—a pessary or surgery—for true anatomical correction and relief.
2. Is a Cystocele linked to cancer risk?
No, a **Cystocele** is a structural issue—a prolapse of tissue—and is not a precursor to, or a risk factor for, bladder cancer or any other type of pelvic oncology. However, it can lead to complications like chronic urinary retention and recurrent urinary tract infections (UTIs).
3. What is the difference between a Cystocele and a Rectocele?
A **Cystocele** (anterior prolapse) involves the bladder bulging into the front wall of the vagina. A Rectocele (posterior prolapse) involves the rectum bulging into the back wall of the vagina. They often occur simultaneously, but treatment strategies for each part of the urological and gynecological system are distinct.
4. Can men get a condition similar to a Cystocele?
While men do not have a vagina for the bladder to prolapse into, they can suffer from analogous pelvic floor disorders, such as a **rectal prolapse** or **urethral prolapse**, usually associated with chronic straining and weakened pelvic structures, particularly after certain prostate surgeries.
5. How long after childbirth should I wait before seeking treatment for a Cystocele?
It is advisable to wait at least six months postpartum to allow for natural tissue recovery and to fully dedicate time to pelvic floor physical therapy. If symptoms persist or worsen after this period, you should consult a specialist.
6. Can a pessary fall out or cause significant pain?
A properly fitted pessary should not fall out during normal daily activities. If it falls out, it means the fit is incorrect, and you must see your healthcare provider immediately. It might cause mild initial discomfort or discharge, but it should not cause significant, ongoing pain.
7. What is the success rate for surgical repair of a Cystocele?
Success rates for surgical **Cystocele** repair (patient satisfaction and anatomical correction) are generally high, often ranging from **85% to 95%** at five years. The primary risk is recurrence, which is why surgical expertise and post-op compliance are so critical. Patients must also consider addressing potential incontinence during the same procedure.
8. Will surgery affect my ability to have children in the future?
If you plan on future pregnancies, surgeons typically recommend delaying definitive surgical **Cystocele** repair until after you finish childbearing, as the delivery process can undo the repair. In the meantime, pessaries are often used for symptom management.
9. Do I need an abdominal incision for Cystocele surgery?
Most standard anterior colporrhaphy procedures are performed entirely through the vagina, meaning there is no visible abdominal incision. However, if the surgeon chooses an abdominal approach (for complex cases or combined procedures), the incision may be small (laparoscopic or robotic) or larger (open surgery).
10. What is “occult stress incontinence,” and how does it relate to Cystocele?
Occult stress incontinence (SUI) is leakage that is only revealed after the **Cystocele** is anatomically corrected. The prolapsed bladder neck can sometimes kink the urethra, artificially preventing leakage. When the prolapse is fixed, this kink is straightened, and the underlying SUI is revealed. Surgeons often test for this pre-operatively with a pessary reduction and may offer a simultaneous SUI procedure.
11. Can diet or supplements help treat a Cystocele?
Diet and supplements cannot fix the structural prolapse. However, a high-fiber diet and adequate hydration are essential for treating and preventing constipation, which is a major risk factor and cause of recurrence. Supplements that support collagen production, such as Vitamin C, may theoretically help connective tissue strength but are not a primary treatment.
12. How soon can I travel after Cystocele repair surgery?
Most surgeons recommend avoiding long periods of sitting and heavy lifting for at least **2 to 4 weeks** post-surgery. Short flights or car rides can be managed after 1-2 weeks, but long-haul international travel should be planned for the 4-6 week mark. Always consult your specific surgeon, especially when coordinating medical travel and recovery, as detailed in our definitive patient handbook on medical visas.
Disclaimer: This article provides general information and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
WMedTour is a leading platform connecting patients with accredited global specialists. Learn more about us on our About Us page or Contact Us for a personalized consultation.
Fallen bladder, anterior prolapse, bladder prolapse, anterior colporrhaphy, pelvic organ prolapse