Cystocele: Comprehensive Guide to Symptoms, Diagnosis, and Advanced Treatment Options 🩺
Understanding the ‘Fallen Bladder’ and Finding Effective Care
✨ Executive Summary: Key Takeaways on Cystocele
WMedTour recognizes that understanding a condition is the first step toward effective treatment.
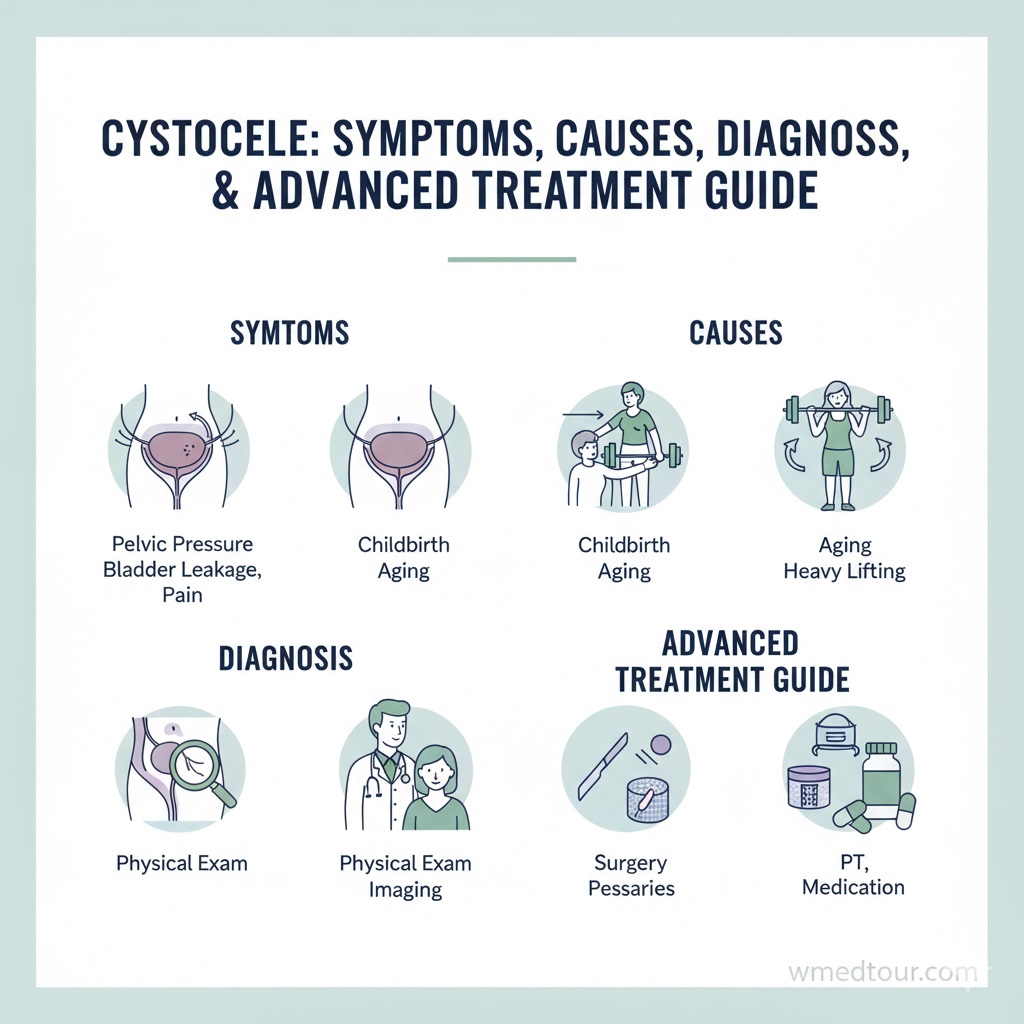
A **Cystocele**, often referred to as a “fallen bladder,” occurs when the wall between a woman’s bladder and vagina weakens, causing the bladder to bulge into the vagina. This condition is a common form of Pelvic Organ Prolapse (POP). Primarily, childbirth and chronic straining contribute to its development. Symptoms range from mild discomfort and pelvic pressure to severe issues like urinary incontinence and difficulty emptying the bladder. Treatment for a **Cystocele** is highly individualized, spanning from conservative management like physical therapy (Kegel exercises) and pessaries, to advanced surgical options such as anterior colporrhaphy (A&P repair) or, less commonly, reconstructive mesh procedures. Early diagnosis through a pelvic exam is crucial. Therefore, women experiencing symptoms should seek consultation promptly. Furthermore, effective management significantly improves quality of life, emphasizing the need for comprehensive patient education and careful specialist selection.
💙 What Exactly is a Cystocele? A Definition
A **Cystocele** represents the prolapse of the urinary bladder into the vagina due to a breakdown of the supportive tissues that separate the two organs. This breakdown, essentially a defect in the anterior vaginal wall, allows the bladder—which rests directly atop this wall—to sag or herniate downward.
Consequently, this creates a visible or palpable bulge within the vaginal canal. It’s important to clarify that while the condition is commonly called a “fallen bladder,” the bladder itself is not falling out; rather, the weakened support structure allows its position to shift. This type of pelvic organ prolapse is one of the most frequently diagnosed conditions in the Gynecological Surgery Department. Given its prevalence, understanding the underlying mechanism is essential for both patients and healthcare providers. Moreover, recognizing the different degrees of prolapse is vital for determining the most suitable course of action.
📌 The Grading System of Cystocele
Clinicians use a standardized system, often the Pelvic Organ Prolapse Quantification (POP-Q) system, to classify the severity of the **Cystocele**. This classification dictates the appropriate treatment path:
- Grade 1 (Mild): The bladder drops only a short way into the upper vagina. Symptoms are often minor or absent.
- Grade 2 (Moderate): The bladder descends to the opening of the vagina. Patients usually feel a distinct bulge or pressure.
- Grade 3 (Severe): The bladder protrudes outside the vaginal opening. This causes significant discomfort and severe symptoms, necessitating immediate attention, typically requiring specialized pelvic floor reconstruction.
- Grade 4 (Complete): The entire bladder and vaginal wall are prolapsed outside the body.
🧠 Causes and Significant Risk Factors
The primary cause of a **Cystocele** is damage or weakness to the pelvic floor muscles and the connective tissue (fascia) that holds the organs in place.
Since the pelvic floor must absorb incredible pressure over a lifetime, several factors can accelerate this weakening.
👀 Key Contributors to Pelvic Floor Weakness
- Childbirth: This is arguably the most significant factor. The physical strain of labor, especially a vaginal delivery involving a large baby or prolonged pushing, stretches and tears the supportive ligaments and muscles. Women who have had multiple children face an increased risk, which is a key consideration in reproductive planning.
- Hysterectomy: Removal of the uterus removes key structural support in the pelvis, subsequently increasing the likelihood of prolapse later in life, sometimes requiring a complex Hysterectomy.
- Age and Menopause: Declining estrogen levels after menopause cause the pelvic tissues to thin, dry, and lose elasticity. Therefore, the supporting fascia becomes less resilient over time.
- Chronic Straining: Repeatedly increasing intra-abdominal pressure significantly weakens the floor. This includes chronic constipation, heavy lifting, or a persistent, severe cough (like from COPD or chronic asthma). In fact, addressing issues like constipation is just as crucial as addressing structural defects.
- Genetics: Some individuals inherently have weaker connective tissue. Consequently, they may be predisposed to develop a **Cystocele** or related conditions like hernias (Hernia Repair).
Understanding these risk factors allows patients to pursue preventative measures. For more detailed information on pelvic floor support, you can review research on the biomechanics of the pelvic floor here.
📜 Identifying the Symptoms and Impact
The symptoms associated with a **Cystocele** vary greatly depending on the grade of prolapse. While mild cases might be asymptomatic, moderate to severe cases often dramatically impact a woman’s quality of life. Patients report a distinct set of issues, primarily related to the bladder’s dysfunction and the physical presence of the prolapse.
💧 Urological Symptoms
- Urinary Incontinence: This is the most common complaint. Stress incontinence (leaking urine during coughing, laughing, or exercising) frequently occurs when the structural support is compromised. This often requires simultaneous or subsequent urinary incontinence surgery.
- Urinary Frequency and Urgency: The bladder’s shifted position can irritate the lining, leading to a constant urge to urinate.
- Difficulty Emptying the Bladder (Urinary Retention): The kinking of the urethra caused by the prolapse prevents the bladder from fully draining. Consequently, patients often have to change position (e.g., lift the prolapse with fingers) to void, a phenomenon known as splinting. Incomplete emptying increases the risk of urinary tract infections.
🍆 Physical and Pain Symptoms
- Vaginal/Pelvic Pressure: Patients describe a feeling of fullness, heaviness, or like “something is falling out” of the vagina. This sensation often worsens by the end of the day or after prolonged standing.
- A Visible Bulge: In Grade 2 or higher cases, a soft tissue mass may be visible at the vaginal opening.
- Sexual Discomfort (Dyspareunia): The physical presence of the prolapse can interfere with intercourse, causing pain or discomfort.
🔎 Diagnosis and Assessment
Diagnosing a **Cystocele** is typically a straightforward process performed in a gynecologist’s or urologist’s office.
🔍 Diagnostic Tools
- Pelvic Examination: The physician performs a thorough pelvic exam, often while the patient is standing or bearing down (Valsalva maneuver), to determine the grade of the prolapse. They use instruments like a speculum to isolate the anterior wall, confirming the presence of the **Cystocele**.
- Bladder Function Tests (Urodynamics): Since incontinence is a major symptom, tests are often required to measure bladder pressure, urine flow rate, and volume. This helps isolate whether the bladder dysfunction is solely due to the physical prolapse or if another condition is involved. Furthermore, specialized procedures like Pelvic Laparoscopy may be used to rule out co-existing issues.
- Cystoscopy: Although less common, the doctor might insert a thin tube with a camera into the bladder to check for stones, tumors, or other abnormalities in the bladder and urethra (Bladder Surgery).
💊 Non-Surgical Treatment Options
For Grade 1 and many Grade 2 cases, conservative management offers excellent relief and can prevent progression. This approach emphasizes strengthening the existing support structures and physically supporting the bladder.
🏋 Lifestyle and Physical Therapy
- Kegel Exercises: These exercises, targeting the pubococcygeus muscles, are the foundation of non-surgical treatment. Consistent performance helps strengthen the entire pelvic floor complex. Patients must perform them correctly, which often necessitates guidance from a specialized pelvic floor physical therapist.
- Weight Management: Reducing excess weight decreases the chronic downward pressure on the pelvic floor. Diet and exercise are powerful tools in prevention and early management.
- Managing Constipation: Preventing straining is paramount. Increasing fiber and fluid intake minimizes the need for forceful bowel movements, protecting the integrity of the pelvic floor. Patients should consult resources like this study on the connection between abdominal pressure and POP from a major health system here.
🧼 Pessaries
A vaginal pessary is a medical device, typically made of silicone, that a physician inserts into the vagina to hold the bladder in place. This is a highly effective, non-invasive method for immediate symptom relief. It requires regular cleaning and replacement, but it is an excellent option for patients who wish to avoid surgery or for whom surgery is medically contraindicated.
📖 Pros and Cons of Non-Surgical Treatment
| Feature | Pros (+) | Cons (-) |
|---|---|---|
| Pessaries | Instant symptom relief; Non-invasive; Avoids anesthesia and hospital stay. | Does not cure the prolapse; Requires regular maintenance and fitting; Potential for vaginal irritation or odor. |
| Pelvic Floor PT | Addresses the root cause (muscle weakness); No side effects; Effective prevention tool. | Requires long-term commitment and dedication; Results are not immediate; Less effective for Grade 3 or higher **Cystocele**. |
🏪 Surgical Treatment for Advanced Cystocele
When conservative measures fail or the **Cystocele** reaches Grade 3 or 4, surgery becomes the most definitive treatment. The goal of surgical repair is to push the bladder back into its correct anatomical position and reconstruct the weakened anterior vaginal wall.
💻 Primary Surgical Technique: Anterior Colporrhaphy (A&P Repair)
The standard procedure is the anterior colporrhaphy. The surgeon makes an incision in the front wall of the vagina, pushes the prolapsed bladder back up, trims away excess tissue, and sutures the strong fascia together beneath the bladder neck to provide robust new support. Surgeons often perform this repair alongside procedures to correct other coexisting prolapse issues. When considering surgery abroad, it’s vital to use checklists like the one for Choosing a Surgeon or Clinic Abroad.
🔧 Modern Advancements and Mesh Use
In certain complex or recurrent cases, surgeons might use surgical mesh to provide reinforcement, although its use in prolapse repair has seen significant regulatory review and decline in recent years due to complications. Today, specialized surgeons prefer native tissue repair whenever possible, often utilizing advanced minimally invasive techniques. Many centers now offer complex reconstructive surgeries using robotic-assisted urological surgery, which offers shorter recovery times and higher precision. For patients seeking such specialized care, destinations like Turkey have become global hubs for medical travel, which you can read more about in our Ultimate Guide to Medical Travel in Turkey.
📖 Pros and Cons of Surgical Treatment (Anterior Colporrhaphy)
| Feature | Pros (+) | Cons (-) |
|---|---|---|
| Native Tissue Repair | Definitive, anatomical repair; High long-term success rates; Resolves the prolapse and related symptoms like urgency. | Requires anesthesia and hospital stay; Involves a recovery period (4–6 weeks); Potential risk of post-operative dyspareunia (painful sex). |
| Mesh-Augmented Repair | May offer stronger support in high-risk patients; Lower recurrence risk initially. | Risk of mesh erosion, pain, or exposure (requires removal); High complexity procedure. |
📄 Comparison Table: Treatment Options for Cystocele
| Treatment Method | Ideal Grade | Efficacy | Recovery Time | Risk Profile |
|---|---|---|---|---|
| Pelvic Floor Therapy (PT) | Grade 1 & Prevention | Good for symptoms, not a cure. | Immediate (Ongoing) | Very Low |
| Vaginal Pessary | Grade 1 & 2 (Temporary) | Excellent symptom management. | None (Fitting required) | Low (Local irritation) |
| Anterior Colporrhaphy | Grade 2, 3, & 4 | Definitive anatomical repair. | 4-6 Weeks | Moderate (Infection, recurrence) |
A thorough discussion with a specialized physician is necessary to tailor the choice of treatment to the patient’s specific health profile and desired outcomes. You can learn more about general gynecological surgery considerations on our Gynecological Surgery Pre-Travel Checklist.
👧 Case Study: Maria’s Journey with Cystocele
🔮 A Patient Journey Example
Maria, a 55-year-old mother of three, began experiencing increasing pelvic discomfort and an inability to fully empty her bladder. She also noticed stress urinary incontinence when she coughed, prompting her to seek help. Her family history included similar issues, suggesting a possible genetic predisposition. Initially, she assumed these were normal signs of aging.
Upon consultation, a specialist performed a detailed pelvic examination and diagnosed her with a Grade 2 **Cystocele**. The physician initially recommended a non-surgical approach. Maria was fitted with a supportive ring pessary and began intensive pelvic floor physical therapy. While the pessary immediately relieved her pressure symptoms, the incontinence persisted, and she found the maintenance cumbersome. Consequently, she decided to pursue definitive surgical correction.
Maria opted for a traditional anterior colporrhaphy, performed by an expert in Turkey, after consulting with WMedTour to find a highly-rated surgeon. The recovery was managed with pain medication and strict adherence to light activity for six weeks. Six months post-surgery, Maria reported a complete resolution of her pelvic pressure and a significant improvement in her incontinence. Her experience underscores that while conservative treatment is a good starting point, surgery often offers the best long-term outcome for a debilitating **Cystocele**. Her successful outcome was a result of early diagnosis and careful selection of her surgical team (Find Doctors).
👩 Who is This For? Understanding the Target Patient
This information is primarily for three groups of people:
- Women experiencing unexplained pelvic symptoms: If you feel a bulge, pelvic pressure, or notice sudden onset of stress incontinence, this guide helps identify potential causes and encourages seeking professional medical advice.
- Healthcare professionals and students: This serves as a comprehensive overview of the current diagnostic and treatment standards for **Cystocele**, including the latest surgical techniques. Furthermore, understanding the scope of pelvic floor disorders is vital for all practitioners in women’s health.
- Patients considering medical travel: If you require surgery for a Grade 3 or 4 **Cystocele** and are exploring high-quality, specialized care options abroad, this article highlights the types of procedures available and the need for thorough preparation, including obtaining a medical visa.
Considering the global landscape of specialized gynecological care, patients must evaluate all their options.
🛡 Prevention and Long-Term Management
Preventing the recurrence or progression of a **Cystocele** is an ongoing process that centers on minimizing pressure on the pelvic floor. Women who have had successful surgical repair or those at high risk (multiple vaginal births, chronic cough, obesity) should rigorously adhere to preventative strategies.
💪 Key Preventative Measures
- Sustained Pelvic Floor Exercises: Commit to daily Kegel exercises indefinitely. Consistency is key to maintaining muscle tone.
- Avoidance of Heavy Lifting: Learn proper lifting techniques if heavy loads are unavoidable, and try to lift from the legs, not the back or abdomen.
- Management of Chronic Conditions: Aggressively treat any underlying conditions that cause chronic abdominal pressure, such as managing asthma or seeking solutions for chronic constipation. Regular women’s health checkups are essential for early detection.
- Hormone Replacement Therapy (HRT): For postmenopausal women, discussing the benefits of localized estrogen therapy with a physician can help maintain the strength and vitality of vaginal and pelvic tissues. You can find more authoritative information regarding POP risk and prevention from top institutions specializing in women’s health here.
Finally, it is paramount to recognize that a **Cystocele** is a physical, treatable condition, not merely an inevitable consequence of aging. Patients have numerous options for treatment, ranging from conservative physical therapy to advanced surgical techniques like Transurethral Resection (if related urological issues are present) or full pelvic floor repair. Understanding these options, as detailed in this comprehensive guide, empowers women to take control of their pelvic health. Our commitment is to ensure access to the best global care, connecting you with experts in conditions ranging from fertility treatments IVF, ICSI, and Egg Donation to complex pelvic surgeries. You can explore further information on pelvic floor rehabilitation from leading research centers here. We also recommend reading this essential guide on global regulations before seeking treatment here.
❔ Frequently Asked Questions (FAQ) About Cystocele
1. Does a Cystocele always require surgery?
No. Mild (Grade 1) cases often require no treatment other than observation and lifestyle modifications. Moderate cases (Grade 2) are often managed successfully with pessaries or pelvic floor physical therapy. Surgery is generally reserved for severe (Grade 3/4) cases or when conservative methods fail.
2. Can men get a Cystocele?
No, a Cystocele is exclusive to women as it involves the vaginal wall and uterus, organs that men do not possess. However, men can experience a similar condition called a bladder prolapse, which is typically a form of hernia. This is more akin to a Hernia Repair than a POP.
3. How does a Cystocele affect sexual function?
The impact varies. Some women experience no change, while others find the physical bulge interferes with intercourse, causing pain (dyspareunia) or discomfort. Successful surgical repair often significantly improves or resolves sexual function issues.
4. How long does it take to recover from Cystocele surgery?
The initial recovery phase, where patients must avoid heavy lifting and strenuous activity, typically lasts 4 to 6 weeks. Full return to normal, unrestricted activities may take up to three months.
5. Are Kegel exercises enough to fix a Grade 3 Cystocele?
Unfortunately, no. While Kegel exercises are crucial for symptom management and preventing further progression, they cannot physically lift and reposition a severely prolapsed bladder (Grade 3 or 4). These advanced stages require definitive anatomical repair, usually surgical.
6. What happens if I ignore a Cystocele?
Ignoring a significant prolapse can lead to complications such as chronic urinary retention (inability to empty the bladder completely), recurrent urinary tract infections (UTIs), kidney damage (in rare, severe cases), and increased physical discomfort. Seeking treatment, even conservative management, is always recommended.
7. What is the success rate of surgical repair?
Native tissue repair (Anterior Colporrhaphy) generally has a high anatomical success rate, often exceeding 85% in terms of initial correction. However, recurrence rates vary, and up to 15-20% of women may experience some degree of recurrent prolapse over many years. This highlights the need for specialized surgeons and advanced techniques like the Pelvic Organ Prolapse Surgery available abroad.
8. Can pregnancy cause a Cystocele to worsen?
Yes. The weight and pressure of a developing fetus, combined with hormonal changes that soften ligaments, can worsen an existing prolapse. Furthermore, vaginal delivery poses the highest risk for progression. Expectant mothers with known prolapse should discuss their birthing options with their obstetrician. For more resources, check our Articles page.
9. What is a pessary made of?
Most modern pessaries are made from medical-grade silicone, which is flexible, durable, and hypoallergenic, making them safe for long-term use.
10. Does having a hysterectomy increase the risk of a Cystocele?
A hysterectomy (removal of the uterus) can remove significant support from the top of the vagina, potentially increasing the risk of subsequent prolapse, though this is debated. This is why surgeons often perform preventative pelvic support procedures during a hysterectomy. Find out more about this complex relationship in research from a university specializing in surgical outcomes here.
11. What is the difference between a Cystocele and a Rectocele?
A **Cystocele** is an anterior wall defect where the bladder prolapses into the vagina. A Rectocele is a posterior wall defect where the rectum bulges into the vagina. Both are forms of Pelvic Organ Prolapse, but they affect different organs and cause different symptoms (bladder issues vs. bowel issues).
12. Are there any medications to treat Cystocele?
There are no medications that will physically repair the tissue defect of a **Cystocele**. However, topical estrogen therapy for postmenopausal women can strengthen the vaginal tissues, and medications can be used to treat co-existing urinary urgency or frequency symptoms. You can explore more on female urology from experts at the Cleveland Clinic here.
13. Is it possible to have a Cystocele without knowing it?
Yes, especially in Grade 1 (mild) cases. The prolapse may be entirely asymptomatic, discovered only during a routine comprehensive checkup or gynecological exam.
14. Where can I find specialized doctors for this condition abroad?
You can search our specialized directory of physicians, focusing on the Gynecological Surgery Department, which often overlaps with Urological Surgery. For example, explore listings like those in Iran or other medical tourism destinations for highly-experienced pelvic reconstructive surgeons.
15. What is the role of the Urology department in treating Cystocele?
Urologists, particularly female pelvic medicine and reconstructive specialists, often treat **Cystocele** because it directly impacts the urinary tract. They are experts in managing the resulting urinary incontinence and voiding dysfunction. Read about Urological procedures in our Laparoscopic Urological Surgery guide.
💗 Conclusion and Next Steps
Managing a **Cystocele** involves personalized care that evolves with the condition’s severity. From the foundational practice of pelvic floor exercises to the precision of modern anterior colporrhaphy, effective solutions exist to restore comfort and function. We urge you to consult with a specialist if you suspect any degree of pelvic organ prolapse. The availability of high-quality surgical care globally, documented by organizations like the NIH here, means that world-class treatment is accessible. Understanding the grading of your **Cystocele** and discussing both conservative and surgical pathways with a trusted physician is the most responsible way forward. For those planning treatment abroad, remember to utilize all our resources, including our Iran Medical Travel Guide and About Us page, to ensure a smooth and informed patient journey.
🔗 Further Reading and Resources
Explore more insights into pelvic health and surgical tourism on these authoritative sites:
- ➤ Review of Pelvic Floor Support Mechanisms: UCLA Gyn Surgery Outcomes
- ➤ Women’s Health Data and Epidemiology: CDC Women’s Health Data
- ➤ Advances in Urogynecology: Johns Hopkins Pelvic Floor Research
- ➤ The Role of Physical Therapy in POP: Duke Physiotherapy Studies
- ➤ Clinical Guidelines on POP Diagnosis: Stanford Urology Research
- ➤ Biomechanics of the Pelvic Floor: Princeton Biomechanics Research
- ➤ Comprehensive Pelvic Health Information: NIH Pelvic Health Portal
- ➤ Research on Women’s Health: Harvard Women’s Health Studies
- ➤ Female Urology and Pelvic Organ Prolapse: Cleveland Clinic Female Urology
- ➤ Mayo Clinic General Women’s Health: Mayo Clinic Women’s Health