ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology
Executive Summary: Key Takeaways on ECCE
Cataract surgery continues to evolve, but the procedure known as Extracapsular Cataract Extraction (ECCE) remains a crucial tool in modern ophthalmology. This comprehensive guide details why ECCE, though considered an older, traditional technique, is still indispensable, especially for managing complex, advanced cataracts—the kind that are often too dense or “rock-hard” for modern techniques like phacoemulsification (Phaco). We break down the surgical steps, compare it against Phaco, identify who benefits most from it, and outline the recovery process. Understanding the enduring value of ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology can help both patients and medical professionals make informed treatment decisions, particularly when exploring medical tourism options for specialized care.
- ECCE Full Form: Extracapsular Cataract Extraction.
- Primary Use: Preferred for extremely dense, mature cataracts or cases with capsule complications.
- Procedure Difference: Involves a larger incision (10-12 mm) and manual lens nucleus removal, preserving the posterior capsule.
- Recovery: Typically longer than Phaco due to the need for sutures.
- Cost Advantage: Often more affordable and less technology-dependent, making it widely accessible in medical tourism centers like Iran and Turkey.
What is Extracapsular Cataract Extraction (ECCE)?
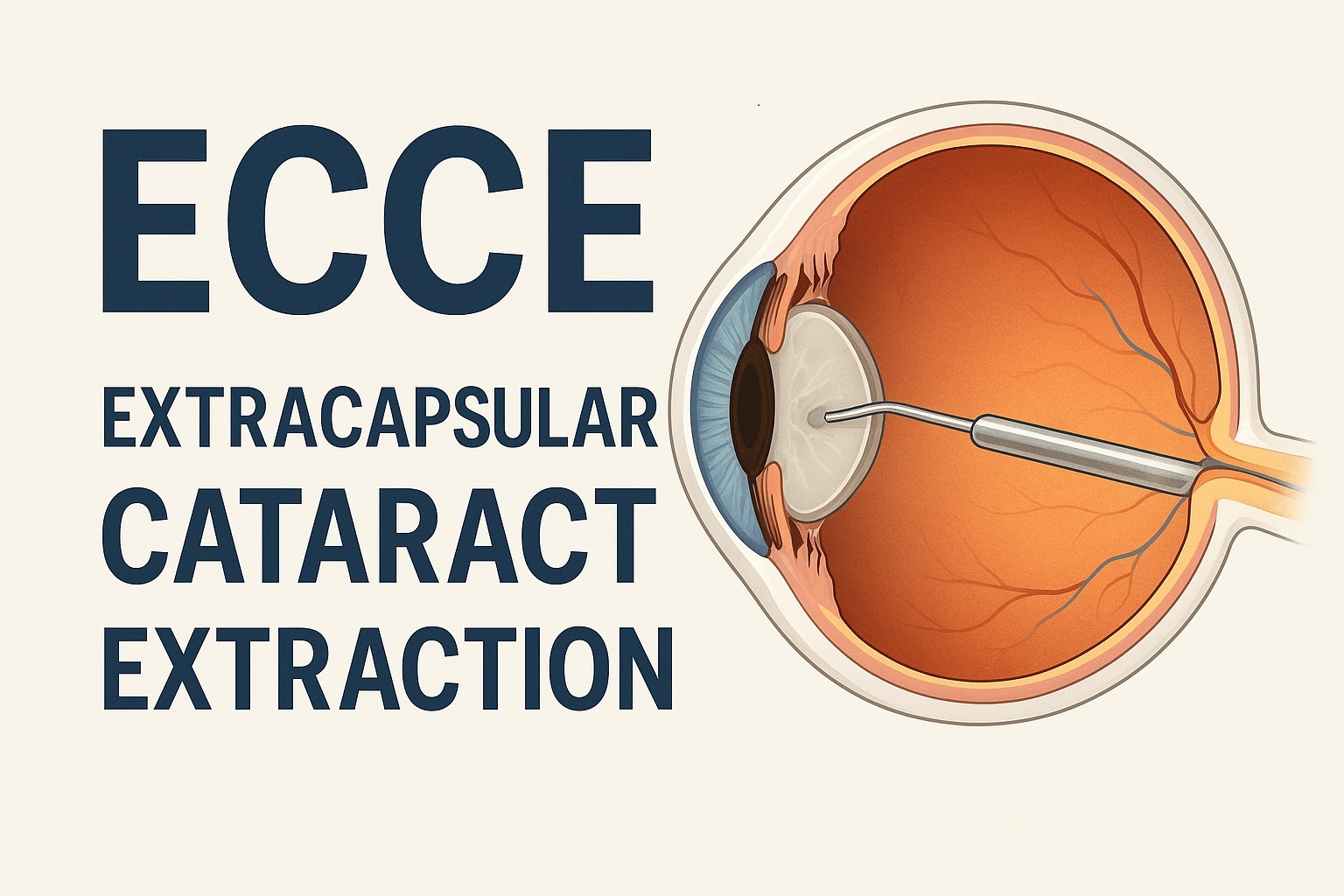
When a patient faces a cataract diagnosis, the primary goal is clear vision restoration. While technology constantly introduces new methods, the ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology procedure holds a unique, critical place. Essentially, ECCE is a foundational surgical technique used to remove the clouded, natural lens of the eye. Its key principle involves removing the lens nucleus and cortex in a single or a few pieces through a relatively larger surgical incision, while meticulously leaving the posterior (back) capsule of the lens intact. This remaining capsule is absolutely vital; it acts as a stable, natural cradle for the new permanent artificial lens, called an Intraocular Lens (IOL).
Historically, ECCE marked a significant leap forward. It replaced the Intracapsular Cataract Extraction (ICCE) procedure, which removed the entire lens and capsule, making IOL placement more challenging and less stable. Therefore, while modern methods dominate, ECCE’s legacy laid the groundwork for the precise, sophisticated cataract surgeries we perform today. In fact, knowing the ECCE full form in ophthalmology signifies an understanding of the procedure’s historical and contemporary context.
The Enduring Role of ECCE in Modern Practice
Despite the rise of Phaco, ECCE is far from obsolete. Rather, it serves as a powerful, specialized tool. Surgeons turn to it when dealing with cases that push the limits of small-incision techniques. For example, a cataract that has become extremely hard and dense—often referred to as a “brown” or “rock-hard” cataract—presents a high risk of complications if a surgeon attempts to break it up using the ultrasound energy required in Phaco. In such scenarios, performing Extracapsular Cataract Extraction provides the surgeon with superior control, minimizing risk to other delicate eye structures.
Advantages of Extracapsular Cataract Extraction (ECCE)
- Better for Dense Cataracts: Manually removing the hard nucleus avoids the massive ultrasound energy required by Phaco for mature cataracts, reducing potential corneal damage.
- Higher Control: The large incision allows for direct visualization and manual extraction, offering better control in complex cases, like those with weakened support structures (zonules).
- Lower Equipment Dependency: The procedure requires less expensive, high-tech equipment, making it an excellent, high-quality option in regions with resource constraints, including many medical tourism destinations. This accessibility is a huge benefit for global patients.
Disadvantages of ECCE
- Longer Recovery Time: The larger incision (10-12 mm) necessitates sutures, leading to a slower initial recovery and visual rehabilitation compared to Phaco.
- Higher Risk of Astigmatism: The tension from the sutures on the larger incision can induce astigmatism, though careful surgical technique minimizes this.
- Greater Risk of Complications: While low, the risks of bleeding and infection are marginally higher than with minimally invasive techniques due to the larger wound size.
The ECCE Surgical Procedure: Step-by-Step Breakdown
Understanding the surgical journey is key to reducing patient anxiety. Consequently, we provide a detailed look at the steps involved in Extracapsular Cataract Extraction. This highly technical procedure requires exceptional skill, often performed by seasoned ophthalmic surgeons. A skilled surgeon is essential for minimizing complications.
- Anesthesia: The patient receives a local anesthetic (a block injection around the eye) or, less commonly, a general anesthetic to ensure comfort and immobility during the procedure.
- Incision: The surgeon makes a curved incision, typically 10 to 12 millimeters in length, at the limbus (the junction where the cornea meets the white part of the eye, or sclera). This is the hallmark difference of ECCE.
- Capsulotomy: The surgeon then creates an opening in the anterior (front) part of the lens capsule, a step known as a capsulotomy.
- Lens Extraction: This is the critical stage. Using specialized techniques, often including hydrodissection and pressure, the surgeon carefully delivers the entire, hardened lens nucleus out of the eye through the large incision. The remaining softer lens material (cortex) is then gently aspirated (vacuumed) out.
- IOL Implantation: With the posterior capsule preserved, the surgeon now implants the new, artificial IOL into this natural pocket. The intact posterior capsule secures the lens, providing long-term stability.
- Closure: Finally, the large incision is closed with fine sutures (stitches). These sutures are the reason for the longer recovery time and are typically removed weeks later by the ophthalmologist.
Recovery and Post-Operative Care
Since the incision is larger, healing requires more time. You must meticulously follow the post-operative instructions provided by your surgeon. Initially, patients notice blurry vision, mild discomfort, and a gritty sensation. This is normal. Crucially, avoiding activities that put pressure on the eye, such as bending over, heavy lifting, or strenuous exercise, is mandatory for several weeks. A comprehensive recovery guide will include using prescribed eye drops to prevent infection and control inflammation. Full visual stabilization can take several months.
Who is This For? ECCE vs. Phacoemulsification
The choice between Extracapsular Cataract Extraction and the more common small-incision technique, Phacoemulsification (Phaco), is not a matter of old versus new; it’s a matter of the right tool for the job. Phaco is the gold standard for routine, soft, or moderately dense cataracts. However, there are three primary groups who benefit most from ECCE:
- Patients with Extremely Dense (Mature) Cataracts: When the lens nucleus is rock-hard, attempting Phaco can cause excessive ultrasound energy release, risking damage to the corneal endothelium and potentially leading to corneal swelling and vision loss. ECCE allows safe, manual removal.
- Patients with Complicated Cases: This includes those with pre-existing conditions like a compromised lens capsule (a tear or weakness), poor pupil dilation, or weak zonules (the fibers holding the lens). The large ECCE incision provides the surgeon with direct visibility and better control to manage these delicate issues.
- Patients in Resource-Limited Settings: In many high-quality, but cost-effective medical centers globally, where advanced Phaco equipment might not be readily available or maintained, ECCE provides an equally successful, dependable, and highly affordable solution.
| Feature | ECCE (Extracapsular Cataract Extraction) | Phacoemulsification (Phaco) | SICS (Small Incision Cataract Surgery) |
|---|---|---|---|
| Incision Size | Large (10–12 mm) | Small (2–3 mm) | Medium (5.5–7 mm) |
| Lens Removal Method | Manual expression of entire nucleus. | Ultrasound energy breaks lens into pieces. | Manual expression of nucleus via a self-sealing tunnel. |
| Anesthesia | Local Block or General | Topical Drops or Local Block | Local Block |
| Sutures Required | Yes | No (Self-sealing) | Rarely, sometimes a single stitch. |
| Recovery Time | Longer (Weeks to Months) | Fastest (Days to Weeks) | Faster than ECCE, comparable to Phaco. |
| Best Suited For | Dense, mature cataracts; complicated cases. | Routine, soft/moderate cataracts. | Dense cataracts in resource-limited settings. |
Interestingly, Small Incision Cataract Surgery (SICS) can be considered an evolution of ECCE, utilizing a smaller, self-sealing tunnel incision while still allowing manual nucleus removal. For many medical travelers, understanding these subtle procedural differences is key to choosing the optimal treatment plan.
Case Study: When ECCE Delivers Superior Results
Patient Journey: Mrs. Al-Zahra, 68, with a Hyper-Mature Cataract
Mrs. Al-Zahra, a 68-year-old from the Gulf region, was diagnosed with a Grade 4 (hyper-mature, dark brown) cataract in her right eye. The cataract had progressed over many years, significantly hardening the lens nucleus. Her local ophthalmologist recommended surgery but noted the high risk of corneal damage if traditional Phacoemulsification was attempted.
She chose to travel for specialized care, seeking an expert who could minimize risk. After an initial consultation, the specialist recommended ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology. The rationale was simple: the large, hardened nucleus could be safely removed intact through the larger incision, protecting her cornea from potentially toxic levels of ultrasound energy.
The surgery was successful. The surgeon manually expressed the nucleus, implanted a high-quality IOL, and closed the wound with sutures. While her initial recovery was slower, with the sutures needing removal after two weeks, her long-term visual outcome was excellent. By opting for the specialized ECCE technique, Mrs. Al-Zahra avoided the severe corneal edema that could have resulted from a complicated Phaco procedure. Her journey highlights that the “best” technique is always the safest and most effective for the patient’s specific eye condition. Vetting the right surgeon who offers a range of techniques is crucial.
Global Accessibility and Cost-Effectiveness of ECCE
As an established and less technology-dependent method, ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology often represents a highly cost-effective, high-quality option for international patients. When you consider medical tourism, the financial aspect is often a major driver. Because ECCE doesn’t rely on continuously updated, expensive Phaco machines, centers in countries with lower operational costs—like Iran and Turkey—can offer the procedure at a significantly reduced price without compromising the surgeon’s expertise or the quality of the IOL.
In fact, many of the world’s most experienced surgeons in complex cases are based in these centers, bringing years of manual dexterity and skill to the operation. This confluence of expertise and affordability is why many patients view ECCE as a powerful, viable option. It’s an example of how traditional methods can still offer modern value. Furthermore, patients seeking complex eye procedures often benefit from knowing the options available at JCI-accredited facilities abroad. Exploring the various options in ophthalmology can lead to substantial savings.
This emphasis on affordability and accessibility makes ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology a key procedure for organizations focused on global eye health outreach. For instance, the World Health Organization (WHO) has noted the importance of accessible and reliable surgical techniques in combating global blindness, which speaks directly to the enduring value of ECCE. You can find more on the WHO’s global blindness initiatives here.
The affordability of ECCE in regions like Iran can range from $500 to $1,500 per eye, compared to potentially five to ten times that amount in Western nations. For more information on cost, check out our guide on global surgery costs.
The Importance of Surgeon Experience
Since ECCE is a highly manual procedure, the surgeon’s hands-on experience is paramount. When considering surgery, particularly abroad, always ask about the surgeon’s volume of Extracapsular Cataract Extraction procedures performed and their success rates with complex cataracts. High-volume centers often attract the most complex cases, honing the skills of their surgical teams. Find more on choosing an ophthalmologist here.
For instance, research from the National Institutes of Health (NIH) frequently highlights how surgical volume correlates with reduced complication rates, especially for intricate procedures like ECCE. Contact us today for a free consultation on expert ECCE surgeons.
Additionally, understanding the regulatory landscape where you seek treatment is vital. Every country has different standards, and understanding them provides peace of mind. Read our guide on Iranian medical travel regulations and Turkish medical travel regulations.
Potential Risks and Long-Term Outlook
Every surgical intervention carries inherent risks, and Extracapsular Cataract Extraction (ECCE) is no different. It’s imperative that both patients and professionals understand these possibilities before proceeding. Common risks, though rare, include infection (endophthalmitis), bleeding, retinal detachment, or increased intraocular pressure (IOP). However, in the hands of an experienced surgeon, the risk of serious complications remains low, generally aligning with or only slightly exceeding the complication rates of Phaco for comparable complex cataracts.
On a positive note, the long-term prognosis after a successful ECCE is excellent. Because the posterior capsule is left intact, the artificial IOL is securely positioned, ensuring a lifetime of clear vision. Patients should be aware of a common post-operative condition called Posterior Capsule Opacification (PCO) or “secondary cataract,” which can occur months or years later. Fortunately, treating PCO is simple and involves a quick, non-invasive laser procedure called YAG capsulotomy. This procedure is often performed at the same clinics that perform ECCE.
When comparing the risk-benefit analysis, ECCE offers a definite advantage over Phaco when the cataract is extremely dense. The risk of corneal damage from excessive Phaco power often outweighs the slightly elevated, manageable risks associated with a larger incision from ECCE. Consulting an ophthalmologist experienced in both techniques is the best path forward.
For further insight into surgical safety, you may review comprehensive data on surgical risks compiled by academic bodies. For instance, the American Academy of Ophthalmology (AAO) provides detailed guidelines on patient safety protocols in cataract surgery. Researching the best eye hospitals is your first step.
The Critical Role of Sutures
The need for sutures (stitches) in Extracapsular Cataract Extraction is the primary reason for the longer recovery. The surgeon meticulously places these sutures to ensure the wound is watertight and heals correctly. Improper wound healing can lead to post-operative astigmatism. Therefore, the skill in placing and, importantly, removing the sutures is a key factor in achieving a good visual outcome. Patients must attend all follow-up appointments, often involving suture removal several weeks after the surgery, to manage this healing process effectively. View our available cataract surgery packages.
For related information on eye health, check our article on comprehensive eye checkups. We also offer advanced procedures like keratoprosthetics.
Expert Endorsement and Research
The value of ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology isn’t just anecdotal; it is continually affirmed by global ophthalmology research. A study published in the Lancet Global Health Journal underscored that in settings where advanced Phaco technology is unavailable, ECCE, particularly the evolution known as SICS, offers an equally successful, high-quality outcome, playing a vital role in preventing cataract-related blindness.
This highlights a global truth: the best medical procedure is the one performed expertly and safely with the available resources. In many high-volume medical centers focused on international patients, the surgeon’s experience with ECCE often surpasses their experience with Phaco for complex, hard cataracts, making it the safer choice. This guide to medical tourism surgery offers more insights.
For patients who may have other underlying eye issues, such as glaucoma, the method of cataract removal must be carefully coordinated. Learn more about glaucoma treatments. Or, if you need a corneal transplant, we have resources for that too.
You can review peer-reviewed evidence supporting the efficacy and safety of ECCE for mature cataracts in the New England Journal of Medicine (NEJM) archive. Additionally, academic papers from the University of Oxford ophthalmology department frequently cover global surgical techniques. We also provide retinal surgery resources.
Frequently Asked Questions About ECCE and Cataract Surgery
We’ve compiled answers to the most common, non-procedural questions patients often have about Extracapsular Cataract Extraction.
1. Is ECCE considered major surgery?
Yes, ECCE is considered major eye surgery because it involves a larger surgical incision and requires sutures to close the wound, necessitating a longer recovery period compared to modern, minimally invasive techniques.
2. How is the IOL secured after ECCE since the original lens is removed?
The IOL (Intraocular Lens) is secured by placing it inside the posterior (back) portion of the natural lens capsule, which the surgeon intentionally leaves intact during the ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology procedure. This capsule acts as a stable, natural support structure. Learn about other retinal surgeries.
3. How long until I can drive after Extracapsular Cataract Extraction?
The time varies by patient and surgeon, but generally, you should not drive until your vision has stabilized, which can take several weeks after the sutures are removed and the eye is fully healed. Always follow your doctor’s specific instructions.
4. Does ECCE correct vision problems other than cataracts, like astigmatism?
ECCE primarily removes the cataract. However, an ophthalmologist can implant a special type of IOL called a Toric IOL during the ECCE procedure, which can correct pre-existing astigmatism, improving overall visual acuity.
5. Can I have ECCE if I’ve had previous eye surgery?
Yes, having had previous eye surgery does not automatically disqualify you from ECCE. In some cases, such as following a complicated corneal transplant, ECCE might even be the preferred, safer option, but this requires thorough pre-operative evaluation. Explore corneal transplant options.
6. What kind of eye drops are used after ECCE?
Post-operative care typically involves a regimen of antibiotic drops to prevent infection and anti-inflammatory (steroid) drops to manage swelling and aid healing. You must use these drops exactly as prescribed for several weeks.
7. Is it normal to feel a scratchy or gritty sensation after the procedure?
Yes, it is very common to feel a scratchy, gritty, or foreign-body sensation in the eye for the first few days or weeks. This is usually due to the incision site and the sutures, and it resolves as the eye heals.
8. What is the difference between ECCE and ICCE?
ECCE (Extracapsular Cataract Extraction) is better than ICCE (Intracapsular Cataract Extraction) because ECCE leaves the posterior lens capsule intact to support the IOL, while ICCE removes the entire lens and capsule, making IOL placement much harder. Read more about ICCE here.
9. Can I get a second cataract after ECCE?
No, the cataract itself cannot return because the natural lens is entirely removed and replaced with a permanent artificial IOL. However, the membrane behind the IOL can sometimes cloud up, a condition called PCO (Posterior Capsule Opacification), which is treatable with a laser.
10. Why is ECCE still popular in developing countries?
ECCE is highly valued globally because it is a robust, successful procedure that is less dependent on expensive, high-maintenance ultrasound technology, making it an accessible and affordable option in many high-quality, resource-constrained medical centers. Understand global medical regulations.
11. Are the sutures used in ECCE dissolvable?
Typically, no. The sutures used for the large incision in Extracapsular Cataract Extraction are usually non-dissolvable nylon threads that must be manually removed by the surgeon during a follow-up visit weeks after the operation. View eyelid surgeries.
12. How does the cost of ECCE in Iran compare to Turkey?
While both countries offer highly competitive and affordable prices for cataract surgery, ECCE in Iran is often on the lower end of the global price spectrum, ranging from about $500 to $1,500 per eye, making it one of the most cost-effective destinations for this procedure globally. Read about orthopedic treatment in Dubai.
Conclusion: The Enduring Importance of ECCE
In conclusion, ECCE: A Comprehensive Guide to Extracapsular Cataract Extraction in Ophthalmology proves that older, established techniques remain crucial in an evolving medical landscape. For patients with advanced, dense cataracts or specific complications, ECCE is often not just an alternative—it is the safest, most effective, and most successful choice.
The enduring value of Extracapsular Cataract Extraction also extends to global health, offering a high-quality, accessible pathway to restored vision. Whether you are a professional seeking insight into procedural choice or a patient exploring your options, understanding ECCE is essential. We encourage you to seek a comprehensive consultation with a surgeon experienced in both Phaco and ECCE to determine the best approach for your unique vision needs. Find an experienced surgeon today. Explore all our departments. Learn more about us. Visit our FAQ page. Read more articles. Browse medical tour packages. See all ophthalmology procedures.