✨
ECCE’s Specific Niche: Why Extracapsular Cataract Extraction Excels in Complex Cases and Resource-Limited Settings
Executive Summary 🔍
While many view Extracapsular Cataract Extraction (ECCE) as the “traditional” cataract surgery, it retains an absolutely vital role in contemporary ophthalmology, especially where newer techniques, like Phacoemulsification (Phaco), fall short. This authoritative guide dissects ECCE’s Specific Niche, detailing precisely when it is not merely an alternative, but the mandatory choice for optimal patient outcomes. Specifically, ECCE proves superior for managing extremely dense cataracts and navigating existing surgical complications. Furthermore, we explore its indispensable nature and high-value contribution to eye health in vast resource-limited settings worldwide. This method ensures that sight restoration remains accessible, affordable, and sustainable globally.
💡 Understanding Extracapsular Cataract Extraction (ECCE)
The evolution of cataract surgery has seen the rise of micro-incision techniques. However, before we delve into ECCE’s Specific Niche, it is crucial to appreciate its fundamental process. ECCE involves the removal of the hard, central nucleus of the cataract through a relatively large incision, leaving the posterior capsule and outer portion of the lens (the anterior capsule rim) intact to support the new intraocular lens (IOL). This method provides a stable platform for lens implantation. Consequently, it offers greater control when facing anatomical or pathological challenges. Therefore, recognizing the full capability of ECCE is essential for both medical professionals and patients researching their options.
🎯 ECCE’s Specific Niche: The Mandatory Choice in Complex Cases
In an ideal world, all cataracts would suit the rapid recovery offered by Phacoemulsification. Nevertheless, there are distinct clinical scenarios where the risks of modern, small-incision surgery outweigh the benefits. This is precisely where ECCE’s Specific Niche becomes invaluable, acting as the indispensable fallback and, often, the primary procedure of choice for the most challenging eyes. Indeed, the decision between ECCE and Phaco is less about which procedure is newer and more about which one ensures the safest, most predictable outcome for that individual patient’s eye.
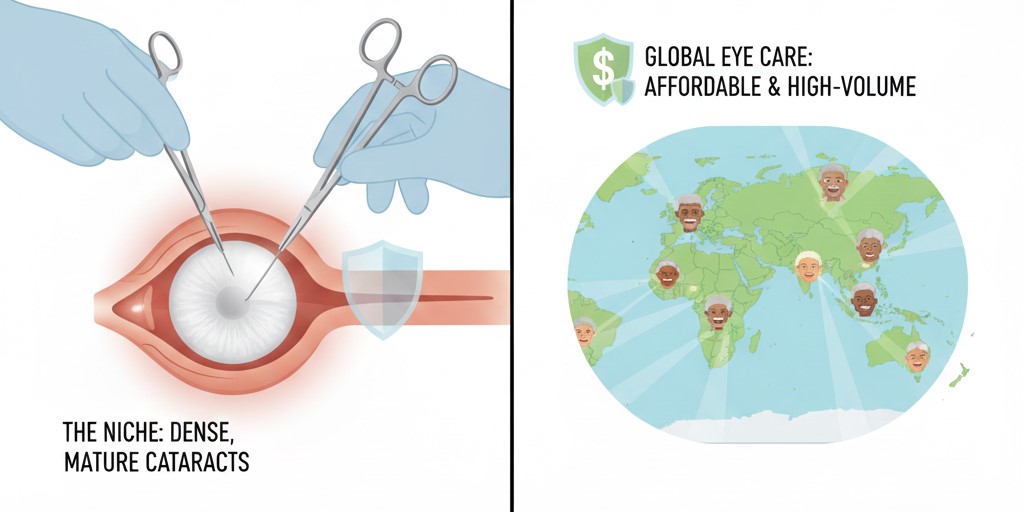
🧱 Handling Dense, Hard, and Mature Cataracts
Cataracts that have progressed to extreme hardness, often referred to as “rock-hard” or “black” cataracts, represent the most definitive indication for ECCE.
Furthermore, in these cases, the lens nucleus is so stiff that it requires a massive amount of ultrasonic energy (Phaco power) to break it down. **Consequently**, this prolonged exposure to high energy within the delicate anterior chamber of the eye significantly increases the risk of thermal burns to the incision site and, critically, irreversible damage to the corneal endothelium—the non-regenerating cell layer that keeps the cornea clear.
Therefore, using ECCE allows the surgeon to extract the cataract nucleus whole or in large, safe segments through the larger incision, thereby completely bypassing the need for excessive intraocular ultrasound. **In essence**, ECCE protects the cornea and the overall integrity of the eye in these extreme circumstances. This protective measure is fundamental to the continued relevance of Extracapsular Cataract Extraction’s niche.
 Pros and Cons: ECCE for Dense Cataracts
Pros and Cons: ECCE for Dense Cataracts
✅ Advantages
- Corneal Protection: Significantly reduces intraocular ultrasound exposure, minimizing endothelial cell loss.
- Efficiency: Often faster removal of a rock-hard nucleus than struggling with Phaco power.
- Safety Margin: Provides a larger margin of safety for the surrounding eye structures.
❌ Disadvantages
- Slower Recovery: The larger incision requires sutures, leading to a longer initial healing period.
- Induced Astigmatism: The wound may cause temporary or permanent changes in the cornea’s shape.
🛡️ The Solution for Intraoperative Complications
Even the most skilled surgeons encounter unforeseen challenges. Significantly, when a complication arises during a small-incision procedure, the surgeon may be forced to convert to ECCE. This capability is a cornerstone of professional ophthalmological training and highlights the procedure’s enduring importance. Notably, two critical scenarios make ECCE indispensable:
Managing Posterior Capsular Rupture (PCR)
A PCR is a surgical emergency where the thin membrane supporting the lens breaks. If this occurs, especially during the nucleus removal phase of Phaco, nuclear fragments may fall into the vitreous gel. In this situation, a Phaco-sized incision is often inadequate for safe retrieval and proper cleanup. The larger ECCE incision facilitates the safe removal of dropped fragments and allows for a stable, controlled placement of the intraocular lens, typically in the sulcus or anterior chamber. Therefore, the ability to convert to ECCE is often the difference between a minor complication and a potentially blinding one. General surgical training principles emphasize having a plan for complications, and in cataract surgery, ECCE is that plan.
Eyes with Pre-existing Conditions
Patients often present with other ocular morbidities that complicate Phaco. For example, small, non-dilating pupils, zonular weakness (fragile support fibers of the lens), or existing corneal opacities all make the precision required for Phaco extremely difficult and dangerous. Conversely, the ECCE technique, with its wide-open view and direct manual manipulation of the lens, offers a less technically demanding and safer route to cataract removal under these conditions. Consequently, a comprehensive pre-operative eye checkup is crucial to determine if these factors necessitate the primary use of ECCE.
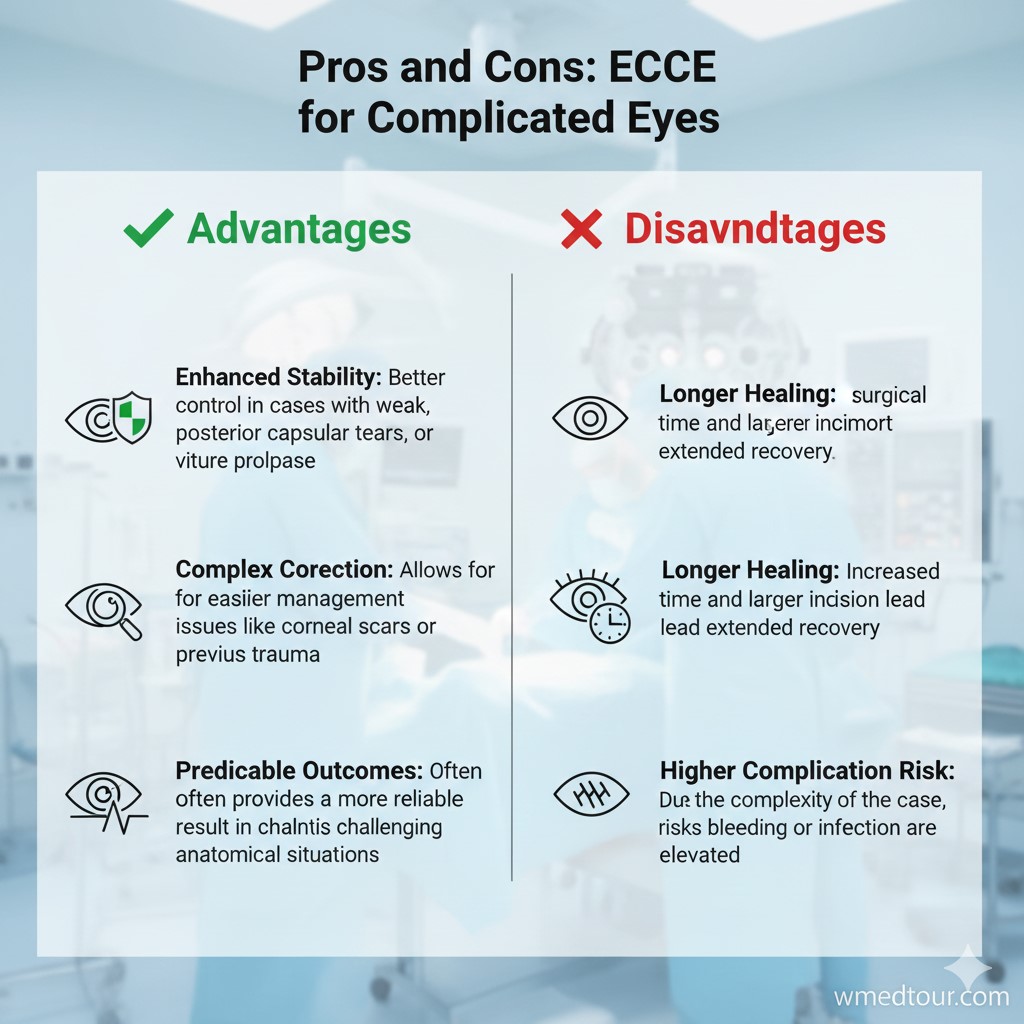
Pros and Cons: ECCE for Complicated Eyes
✅ Advantages
- Control: Provides superior instrument access and visibility for managing vitreous loss or lens fragment retrieval.
- Lens Implantation: Easier placement of a large IOL in the absence of capsular support, which is often crucial for visual rehabilitation.
❌ Disadvantages
- Vitreous Management: While providing better access, managing vitreous humor may be more extensive due to the larger wound.
- Post-operative Care: Requires more vigilant post-operative monitoring due to the complexity of the initial surgery.
🌍 ECCE’s Indispensable Role in Resource-Limited Settings
Beyond its role in complex clinical scenarios, a second, equally important pillar of ECCE’s Specific Niche lies in global public health and medical outreach. Cataract blindness is a massive burden, particularly in developing nations, and ECCE offers an extremely effective, sustainable, and high-volume solution. The World Health Organization (WHO) and global health initiatives recognize that sustainable surgery must prioritize simplicity and affordability. Therefore, the adoption of ECCE, or its modern variant, Manual Small Incision Cataract Surgery (MSICS)—which shares the key principles of ECCE but reduces incision size—is a humanitarian and practical imperative.
💲 Cost-Effectiveness and Sustainability
Phacoemulsification relies on sophisticated machines that cost tens of thousands of dollars, require regular, expensive maintenance, and depend on a constant supply of disposable Phaco tips and cassettes. Conversely, ECCE and MSICS primarily utilize basic, autoclavable (reusable) surgical instruments and a simple operating microscope. This drastically reduces the capital investment and the prohibitive running costs. In fact, the cost difference can be staggering, making ECCE the only financially viable option for mass cataract campaigns in low-income regions. The low overhead ensures that high-quality, sight-restoring surgery can be delivered affordably, making ECCE a true high-value procedure. Furthermore, this sustainability allows local healthcare providers to establish and maintain their own services without dependence on international aid for high-tech supplies. Consequently, this boosts the overall capacity of the local ophthalmology department.
🎓 Training and Equipment Logistics
The training curve for a competent ECCE or MSICS surgeon is significantly less steep and machine-dependent than for Phaco. Hence, training a new cohort of surgeons in ECCE’s Specific Niche is a faster, more reproducible process that does not rely on access to advanced simulation equipment. Moreover, the equipment is easier to transport, set up, and repair in remote field hospitals or clinics with unreliable infrastructure. This logistical simplicity is an overriding factor in effective cataract management in vast areas of Africa, South Asia, and parts of Latin America. Therefore, organizations focused on global eye health continue to rely on and train surgeons in this robust technique.
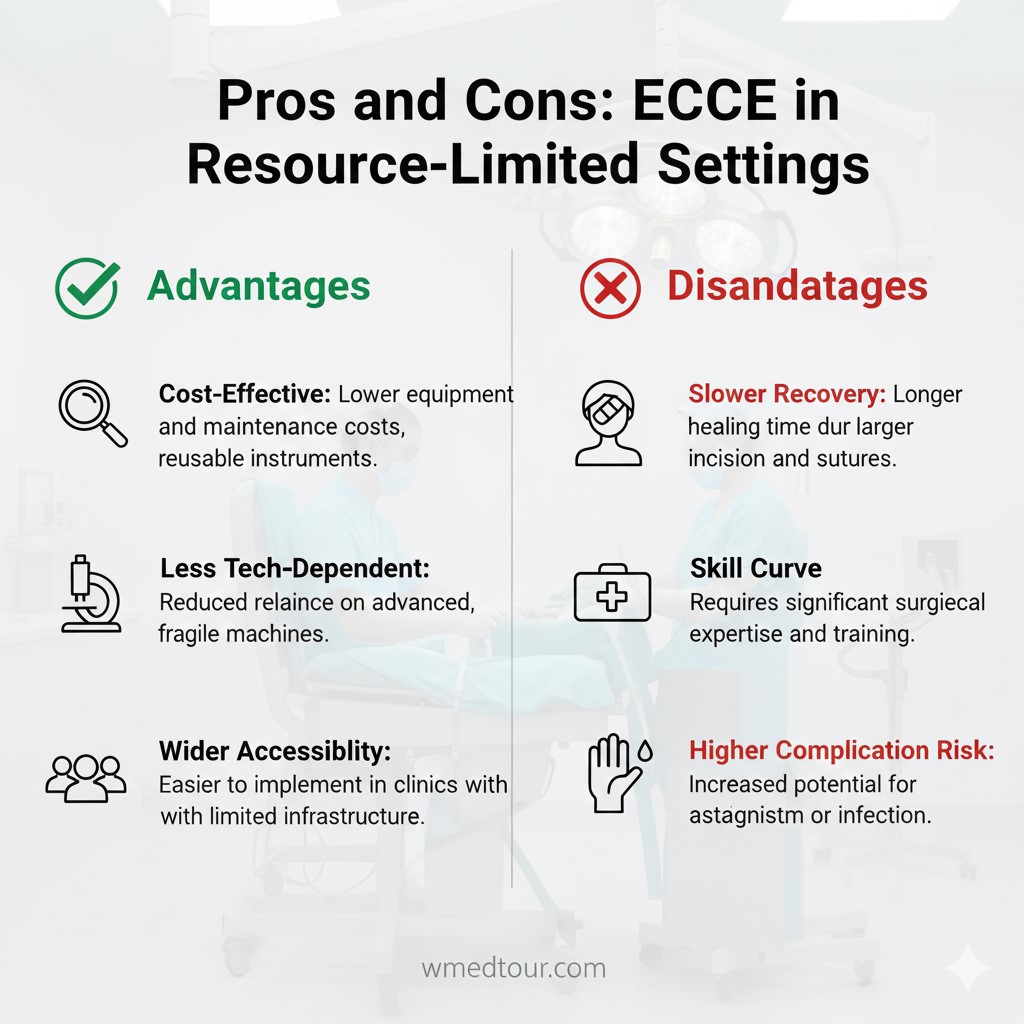
Pros and Cons: ECCE in Resource-Limited Settings
✅ Advantages
- Extreme Affordability: Minimal capital expenditure and use of non-disposable instruments.
- Portability and Durability: Equipment is simple, rugged, and easy to maintain in remote areas.
- High Volume Capacity: Enables rapid, mass treatment of cataract blindness, a critical public health objective.
❌ Disadvantages
- Patient Compliance: Post-operative recovery is longer, requiring greater patient discipline with eye drops and activity.
- Vision Fluctuation: Slower stabilization of vision compared to the immediate ‘wow’ effect of micro-incision surgery.
⚖️ Comparison Table: Extracapsular Cataract Extraction (ECCE) vs. Phacoemulsification
To further clarify ECCE’s Specific Niche, let us compare the two dominant methods based on key parameters.
| Feature | ECCE (Extracapsular Cataract Extraction) | Phacoemulsification (Phaco) |
|---|---|---|
| Primary Indication | Dense/Mature Cataracts, Complicated Eyes, Resource-Limited Settings | Routine, Soft-to-Medium Density Cataracts |
| Incision Size | Large (8–12 mm), requires sutures | Small (2–3 mm), often self-sealing |
| Corneal Trauma/Energy | Minimal (No ultrasound power used inside the eye) | Requires high-frequency ultrasound energy |
| Equipment Cost | Low capital cost, sustainable, basic instruments | Very High capital cost, requires expensive maintenance and disposables |
| Initial Recovery Time | Slower (weeks to months for final vision) | Faster (days to weeks for functional vision) |
| Astigmatism Risk | Higher, due to the large, sutured incision | Very Low, due to micro-incision design |
The table clearly illustrates why both procedures coexist. Ultimately, the choice is determined by the patient’s individual eye pathology and the available infrastructural resources.
👤 Who is This For?
Understanding ECCE’s Specific Niche is crucial for a broad audience. This information is highly relevant to:
The Prospective Patient
If your doctor has told you you have an extremely advanced or dense cataract, or if your surgeon has mentioned pre-existing ocular issues, ECCE might be recommended as the safest primary option. Also, if you are considering medical tourism for ophthalmology and your case is complex, seeking a high-volume center that excels in ECCE may be your best path to vision restoration. Always utilize our surgeon and clinic vetting checklist before committing.
The Global Health Professional
For ophthalmologists, residents, and healthcare administrators operating in or planning missions to low-resource areas, ECCE and MSICS represent the sustainable standard of care. Training and promoting this technique is vital to meeting the WHO’s goals for reducing global cataract blindness. The principles of safe ECCE should be taught alongside modern techniques to create robust, adaptable surgeons. Furthermore, understanding the regulatory landscape for global medical treatment is part of responsible practice.
🗺️ Case Study: A Global Patient Journey – The Need for ECCE
Patient Profile: Mr. Davut, Age 75 (Hypothetical)
Mr. Davut, a 75-year-old gentleman from a remote village, presented with a mature, rock-hard “brunescent” cataract in his right eye. His vision deteriorated for over a decade. His local clinic had access to a high-quality Phaco machine but advised against its use. Instead, they referred him to a regional hospital renowned for its high-volume ECCE program, often supported by international training initiatives (similar to this Turkey location).
The Clinical Challenge and ECCE Solution
The primary risk was corneal damage. The density of the cataract meant a Phaco procedure would take over 10 minutes of intense ultrasound, practically guaranteeing significant, potentially blinding, corneal endothelial cell loss. Therefore, the senior surgeon, who had trained in the robust methods of ECCE’s Specific Niche, elected for a primary ECCE. The procedure involved a controlled, approximately 10mm limbal incision, manual expression of the hard nucleus, and insertion of a low-cost, rigid intraocular lens. The entire nucleus was removed in seconds once the incision was created, dramatically minimizing internal eye trauma.
Outcome and Takeaway
Despite the initial slower visual recovery, Mr. Davut’s cornea remained perfectly clear. His vision, while not immediate, steadily improved to 20/40 after two months, a life-changing result given his prior near-blindness. Crucially, the hospital performed this procedure safely and affordably, leveraging the low-cost model of ECCE. This case exemplifies why ECCE is the most ethical and clinically responsible choice when patient safety outweighs the pursuit of a faster recovery time. Patients must check their medical visa requirements before undertaking such travel.
❓ Frequently Asked Questions (FAQ)
ECCE’s Role in Safety and Superiority
Yes, for an extremely dense or mature cataract, surgeons often consider ECCE safer. The stiff nucleus of a dense cataract requires significantly more ultrasonic energy during Phacoemulsification, which can increase the risk of corneal endothelial damage. ECCE, however, removes the nucleus whole or in large pieces outside the eye, minimizing internal trauma.
ECCE is the preferred choice when pre-existing corneal damage, poorly dilating pupils, or a compromised posterior capsule (the lens’s supporting membrane) complicate the procedure. Its larger incision allows surgeons better control and easier implantation of a large, rigid intraocular lens (IOL) when the standard IOL used in Phaco is not feasible. This directly relates to ECCE’s Specific Niche in managing difficult eyes.
ECCE typically results in slower initial visual recovery compared to Phaco. Because ECCE involves a larger incision that requires sutures, a longer healing period is needed. Patients generally must wait several weeks for the sutures to dissolve or be removed, and final visual acuity may take a few months to stabilize, whereas Phaco offers faster initial results.
Yes, theoretically, surgeons can use ECCE to remove any type of cataract. However, for routine, soft, or moderately dense cataracts, Phacoemulsification is often the preferred method due to its smaller incision and faster recovery. ECCE’
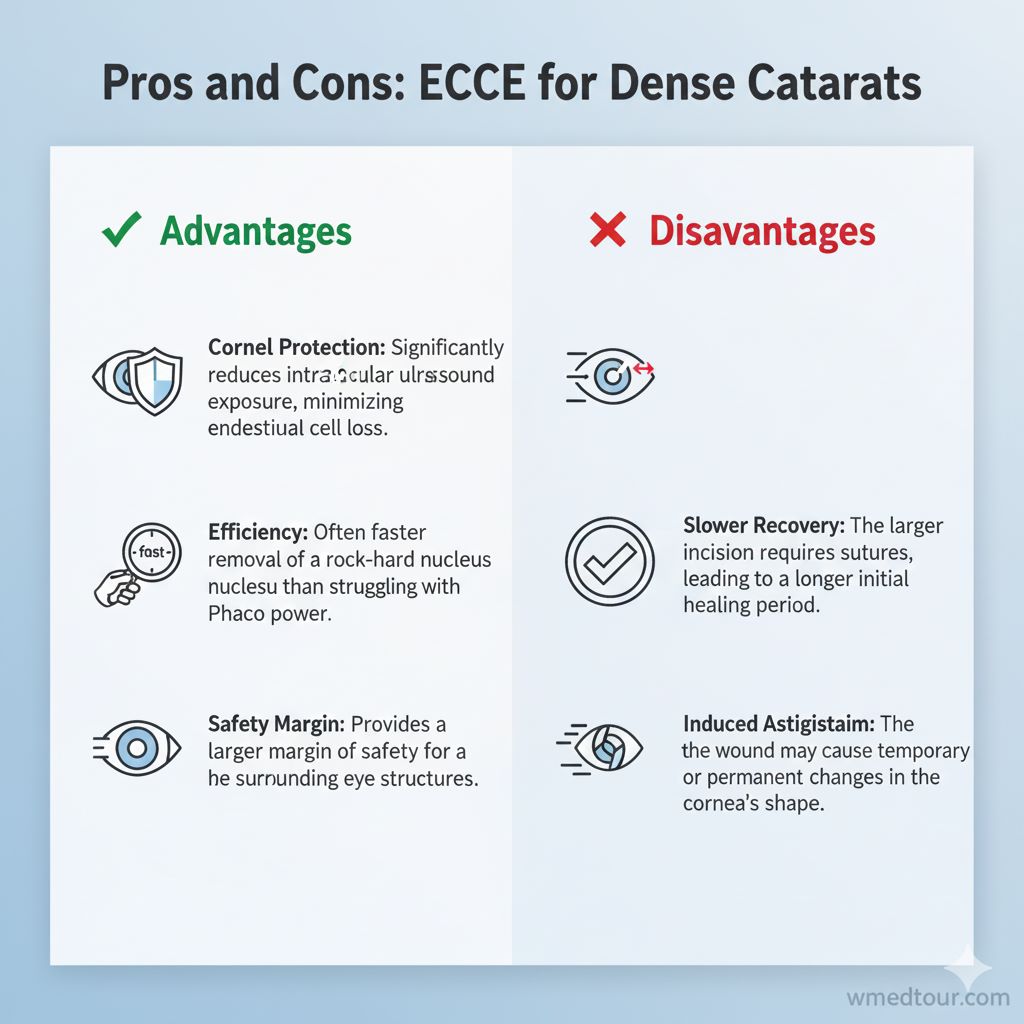 Pros and Cons: ECCE for Dense Cataracts
Pros and Cons: ECCE for Dense Cataracts