Fetal Gender Selection: Risks, Success Rates & Your Options in 2026 👶🧬
Executive Summary: Navigating Modern Family Balancing 📝
In 2026, fetal gender selection has transitioned from a futuristic concept to a highly precise medical reality. This guide provides a detailed look at the clinical pathways available for parents. While technical accuracy is nearly 100% with modern methods like PGT-A, the journey involves significant emotional and financial investments. We analyze the primary methods including IVF with genetic screening. We also highlight the importance of choosing accredited international centers. This article emphasizes that while the science is robust, understanding the ethical landscape and medical risks is vital for any prospective parent.
What is Fetal Gender Selection?
Fetal gender selection is the process of influencing or determining the sex of a baby before conception or implantation. The two most common approaches are:
Sperm Sorting: This technique separates X- and Y-chromosome-bearing sperm to increase the likelihood of conceiving a child of the desired gender. It can be combined with intrauterine insemination (IUI) or in vitro fertilization (IVF).
Preimplantation Genetic Testing (PGT) with IVF: Embryos are created via IVF, tested for gender in the laboratory, and only embryos of the desired gender are implanted. This method is the most accurate but more complex and costly.
Each method has advantages and limitations regarding accuracy, invasiveness, and cost.
Who is This For? 👥
This guide addresses a diverse audience seeking clarity on reproductive technologies. It is specifically designed for:
- Couples desiring family balancing to ensure a mix of genders in their household.
- Individuals with a history of sex-linked genetic disorders seeking healthy offspring.
- Medical professionals staying updated on the latest gynecological surgery department trends.
- Patients researching all locations for advanced fertility treatments.
Understanding Fetal Gender Selection in 2026 🧬
Fetal gender selection refers to the medical process of choosing the sex of a baby before a pregnancy is established. In 2026, the gold standard remains Preimplantation Genetic Testing for Aneuploidy (PGT-A). This process occurs during an In Vitro Fertilization (IVF) cycle. However, the decision to pursue this path is complex. Science has advanced significantly, making the process safer and more accessible. Despite this, patients must navigate varying international laws and clinical protocols.
The Science of Genetic Screening 🔬
Modern laboratories now use Next-Generation Sequencing (NGS) to examine embryos. This technology allows doctors at the oncology department and fertility centers to see chromosomal health. They can identify the presence of XX or XY chromosomes with near-perfect accuracy. Consequently, the term “gender selection” is often a byproduct of a broader health screening. This ensures that only the healthiest embryos are transferred to the uterus.
The Emotional and Ethical Landscape 🕊️
Entering the world of assisted reproduction requires a steady mindset. Many parents feel a mix of excitement and anxiety. Transitioning into this phase often requires support from specialists found in our about us section. Ethics play a massive role as many countries restrict selection for non-medical reasons. Therefore, many families seek care in regions where family balancing is legally protected and clinically supported.
Primary Methods for Sex Selection 🛠️
IVF with PGT-A (Preimplantation Genetic Testing)
This is the most effective method available today. The process begins with standard IVF protocols. After egg retrieval and fertilization, the resulting embryos grow for five days. At the blastocyst stage, a few cells are biopsied. These cells reveal the genetic makeup without harming the embryo. This method is highly recommended for those visiting a checkup department for fertility assessments.
MicroSort (Sperm Sorting)
While less common than PGT-A, sperm sorting technologies like MicroSort attempt to separate X and Y-bearing sperm. This happens before insemination. However, the success rates are lower than genetic testing. It is often used in conjunction with Intrauterine Insemination (IUI). Many patients explore this at Iran medical centers due to the advanced technology available there.
Pros and Cons of Fetal Gender Selection ⚖️
The Advantages 🌟
- Prevention of sex-linked genetic diseases like Hemophilia or Duchenne Muscular Dystrophy.
- Psychological satisfaction for parents pursuing family balancing.
- Increased chance of a healthy pregnancy through comprehensive chromosomal screening.
- Access to world-class doctors specializing in reproductive endocrinology.
The Challenges ⚠️
- The process requires invasive procedures like egg retrieval and embryo biopsy.
- Significant financial investment is often required, as seen in our faq cost sections.
- Emotional stress associated with IVF failure or lack of embryos of the desired sex.
- Legal restrictions in many European and Asian countries.
Comparison Table: Gender Selection Techniques 📊
| Method | Accuracy | Complexity | Primary Use |
|---|---|---|---|
| PGT-A (IVF) | >99% | High (Invasive) | Medical & Balancing |
| Sperm Sorting | 70-85% | Moderate | Pre-conception |
| Natural Methods | 50% (Random) | Low | Non-medical |
The Patient Roadmap: Your Journey to Success 🗺️
Step 1: Initial Virtual Consultation
Your journey begins with a telemedicine consultation. During this call, fertility specialists review your medical history. They discuss your goals for fetal gender selection. This stage is crucial for managing expectations and understanding the legalities involved.
Step 2: Diagnostic Testing and Prep
Before traveling to Mashhad or other hubs, you undergo blood work. This includes hormone testing and ultrasound. If you have concerns about other health areas, you might visit the cardiac surgery or ophthalmology department for a full pre-op clearance.
Step 3: The IVF Cycle
The mother undergoes ovarian stimulation for about 10-12 days. This is followed by a minor surgical procedure for egg retrieval. These eggs are then fertilized in the lab. If there are any unrelated issues, such as a need for plastic surgery after pregnancy, those are noted for future planning.
Step 4: Biopsy and Selection
Once embryos reach day five, the biopsy occurs. Samples are sent to a genetics lab. Within a week, a report identifies the gender and health of each embryo. You then choose which embryo to transfer back to the uterus.
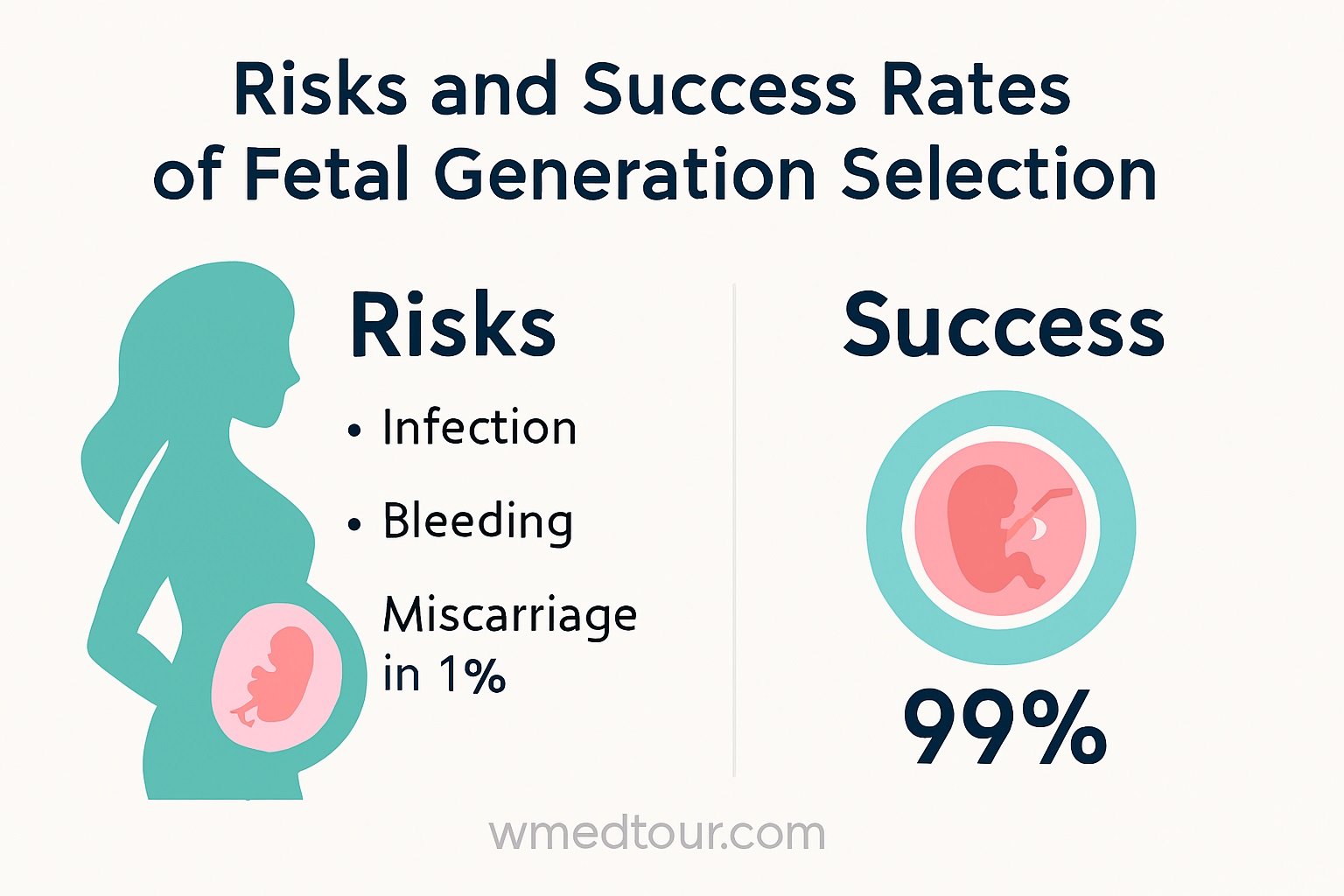
Risk Assessment and Safety in 2026 🛡️
Safety is the cornerstone of modern reproductive medicine. However, no medical procedure is without risk. Ovarian Hyperstimulation Syndrome (OHSS) is a potential complication of IVF. Furthermore, the biopsy process carries a less than 1% risk of damaging the embryo. Transitioning to a high-volume clinic significantly reduces these risks. According to research from Cambridge University, the expertise of the embryologist is the most critical factor in success.
Ensuring Long-term Health
Studies continue to show that children born via IVF and PGT-A are as healthy as naturally conceived children. Nevertheless, follow-up care is essential. Patients are encouraged to utilize our contact us page to coordinate post-transfer monitoring. This ensures the pregnancy progresses safely under expert guidance.
Case Study: Sarah and Mark’s Path to Family Balancing 📖
Sarah and Mark had three wonderful boys but always dreamt of a daughter. They decided to pursue fetal gender selection through an international program. Initially, they were hesitant about the IVF process. However, after a thorough consultation with a fertility expert from our departments list, they felt confident. They traveled for treatment, combined with one of our tours in Iran. They successfully produced two healthy female embryos. Today, they are the proud parents of a baby girl. Their story highlights how modern technology can fulfill personal family goals when combined with expert medical care.
Cost Analysis Table: International Comparisons 💸
| Service Component | Estimated Cost (USD) | Note |
|---|---|---|
| Full IVF Cycle | $4,500 – $8,000 | Includes medications |
| PGT-A (up to 8 embryos) | $2,000 – $3,500 | Essential for gender |
| Embryo Transfer | $1,000 – $2,000 | Per attempt |
Recovery and Medical Tourism Excellence 🌟
Recovery after egg retrieval is generally quick. Most patients return to light activities within 24 hours. While waiting for genetic results, many families take the opportunity to explore. Enjoying tours in India or Oman can turn a clinical trip into a memorable vacation. Transitioning from the stress of treatment to a relaxing environment promotes better outcomes. Our coordinators assist with all logistics, from dental checkups to specialized surgical appointments, ensuring a seamless experience.
Medical Disclaimer ⚠️
The information provided in this article is for educational purposes only. It does not constitute medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider. Furthermore, fetal gender selection is subject to local laws. Ensure your chosen path complies with the regulations of both your home country and the treatment destination. For more information, visit our faq section or consult with a legal professional.
Frequently Asked Questions (FAQ) ❓
1. Is fetal gender selection 100% accurate in 2026?
With PGT-A, the accuracy of identifying the embryo’s sex is over 99.9%. Errors are extremely rare and usually related to laboratory anomalies rather than technology failure.
2. Can I choose the gender without doing IVF?
No, medical gender selection requires embryos to be created outside the body to be tested. Natural methods or “diets” have no scientific basis for choosing sex.
3. How long does the whole process take?
From the first consultation to embryo transfer, the process usually takes 2 to 3 months, depending on your biological cycle and lab timelines.
4. Are there any health risks for the baby?
Yes, there are some considerations regarding the baby’s health with IVF, but overall, most babies born through IVF are healthy. Here’s a clear breakdown:
1. Slightly higher risks at birth
- Multiple pregnancies: IVF often involves transferring more than one embryo, which increases the risk of twins or triplets. Multiples are more likely to be born prematurely or with low birth weight.
- Premature birth & low birth weight: Even singleton IVF babies have a slightly higher chance compared to naturally conceived babies, but the difference is small.
2. Birth defects
- Studies show a very small increase in certain congenital anomalies in IVF babies, but the absolute risk is still low.
- Much of the risk is thought to come from underlying infertility factors, not the IVF procedure itself.
3. Epigenetic and long-term health
- Research is ongoing, but current evidence suggests that long-term health (childhood development, school performance, and adult health) is generally comparable to naturally conceived children.
4. Minimizing risks
- Using single embryo transfer whenever possible reduces multiples and associated risks.
- Choosing a clinic with high standards and experienced embryologists helps ensure proper embryo handling.
- Monitoring during pregnancy is important, especially if IVF involved more advanced procedures (like ICSI or donor eggs).
✅ Bottom line: Most IVF babies are healthy. Risks are slightly higher than natural conception, mainly due to multiples, but careful planning and monitoring can minimize these risks.
5. Which country is best for family balancing?
Countries like the USA, UAE, and Iran are popular because they offer advanced PGT-A technology and favorable legal frameworks for non-medical gender selection.
6. What happens if no embryos of the desired gender are found?
This is a possibility. In such cases, patients can choose to transfer a healthy embryo of the other gender or start a new IVF cycle.
7. Does insurance cover gender selection?
Most insurance plans do not cover gender selection unless it is medically necessary to prevent a sex-linked genetic disorder.
8. Is there an age limit for this procedure?
There is no universal age limit for fetal gender selection, but age does matter medically and legally, depending on how the gender selection is done and the country where it is performed.
Here’s a clear, structured explanation 👇
First: How Fetal Gender Selection Is Done
Gender selection is usually achieved through:
🔹 IVF with PGT (Preimplantation Genetic Testing)
- Eggs are retrieved, fertilized in the lab
- Embryos are genetically tested
- Embryos of the desired gender are transferred
👉 This is the only reliable and legal medical method in most countries.
Is There an Age Limit? (Medical Perspective)
✅ For Women
There is no fixed legal age cutoff, but biological limits apply:
- Under 35: Highest success rates
- 35–40: Reduced egg quality, still possible
- 40–43: Possible but lower success; often needs multiple IVF cycles
- Over 43–45: Many clinics recommend donor eggs
⚠️ Clinics may refuse treatment if pregnancy risks are considered too high.
✅ For Men
- No strict age limit
- Sperm quality may decline after 45–50
- Genetic risks increase slightly but usually manageable
Legal & Clinic-Imposed Limits
Even if medically possible, clinics may set limits such as:
- Maximum maternal age (often 45–50)
- Requirement for medical clearance
- Psychological counseling (in some countries)
Country-Specific Rules (Important)
Age limits and legality vary widely:
- Permissive countries may allow gender selection for family balancing
- Restrictive countries allow it only for medical reasons
- Some countries ban non-medical gender selection entirely
👉 Age limits are often clinic policy, not national law.
Important Health Considerations
Older maternal age increases risks of:
- Miscarriage
- Chromosomal abnormalities
- Pregnancy complications (e.g., preeclampsia, gestational diabetes)
That’s why clinics focus more on health status than age alone.
Bottom Line
✔ There is no absolute age limit
✔ Female age (egg quality) is the key factor
✔ Clinics may impose their own age caps
✔ Donor eggs are an option for older women
9. Can I do ivf if I already have children?
Yes! Having children already does not prevent you from doing IVF. IVF is used for a variety of reasons, not just infertility in people who have never conceived. Here’s a breakdown:
Why someone with children might do IVF
- Age-related fertility decline – Even if you had children before, fertility can decrease with age. IVF can help if natural conception is now difficult.
- Male or female factor infertility – Issues like low sperm count, ovulation problems, or blocked fallopian tubes can occur later.
- Genetic concerns – Some parents opt for IVF with preimplantation genetic testing (PGT) to reduce the risk of passing on genetic conditions.
- Same-sex couples or single parents – IVF is commonly used with donor sperm or eggs, regardless of previous children.
- Repeated pregnancy loss – IVF can sometimes help identify and prevent causes of miscarriage.
Key points
- Your previous pregnancies usually do not reduce your chances of IVF, though age and ovarian reserve do.
- Clinics may evaluate your fertility history and overall reproductive health to design the best protocol.
- IVF success rates vary, but prior successful pregnancies can be a positive sign for future IVF attempts.
10. How many embryos are usually tested?
On average, clinics test between 4 and 10 embryos per cycle, depending on how many eggs are successfully retrieved and fertilized.
11. Is sperm sorting as good as embryo testing?
Not exactly — sperm sorting and embryo testing are both methods for gender selection, but they differ significantly in accuracy, reliability, and application. Here’s a detailed comparison:
1. Sperm Sorting
How it works:
- Sperm is separated into X-bearing (girl) and Y-bearing (boy) before fertilization.
- Only the desired sperm is used to fertilize the egg (usually via IVF or IUI).
Pros:
- Less invasive than testing embryos.
- Can be used with IUI (in some cases) or IVF.
- Avoids embryo destruction, which some patients prefer.
Cons:
- Accuracy: ~70–80% (less reliable than embryo testing).
- Success depends on sperm quality and lab technique.
- Cannot detect genetic diseases — only gender.
2. Embryo Testing (PGT/PGD)
How it works:
- Eggs are fertilized in vitro.
- Embryos are biopsied at day 5.
- DNA testing identifies gender and can also detect genetic disorders.
- Only embryos of the desired gender are transferred.
Pros:
- Accuracy: >99% — almost guaranteed gender selection.
- Detects genetic diseases, not just gender.
- Standard for non-medical gender selection in many countries.
Cons:
- More invasive (biopsy of embryos).
- Higher cost.
- Requires IVF, even if no fertility issues exist.
- Ethical/legal restrictions in some countries.
💡 Bottom Line
| Feature | Sperm Sorting | Embryo Testing (PGT) |
| Accuracy | 70–80% | >99% |
| Detects Genetic Disorders | No | Yes |
| Invasiveness | Low | Moderate |
| Cost | Lower | Higher |
| Standard for Gender Choice | Some clinics | Most clinics |
✅ Summary:
- Embryo testing is more reliable and precise, especially if you also want to screen for genetic diseases.
- Sperm sorting is less invasive and cheaper but less accurate.
12. Where can I find reputable clinics for this?
You can browse our list of doctors and accredited hospitals on the WMedTour portal for verified options worldwide.
By understanding the Fetal Gender Selection: Risks, Success Rates & Your Options in 2026, you empower your family to make the best reproductive choices. Contact us today to start your journey toward a balanced family future.