Fetal Gender Selection Success Rates 2026 📊: PGT-A vs. MicroSort Guide 🔬
Choosing your child’s gender is a significant decision. Discover the definitive comparison of PGT-A and MicroSort, focusing on the latest Fetal Gender Selection Success Rates 2026, procedures, ethical considerations, and global availability.
✨ Executive Summary: The Choice Between Precision and Accessibility
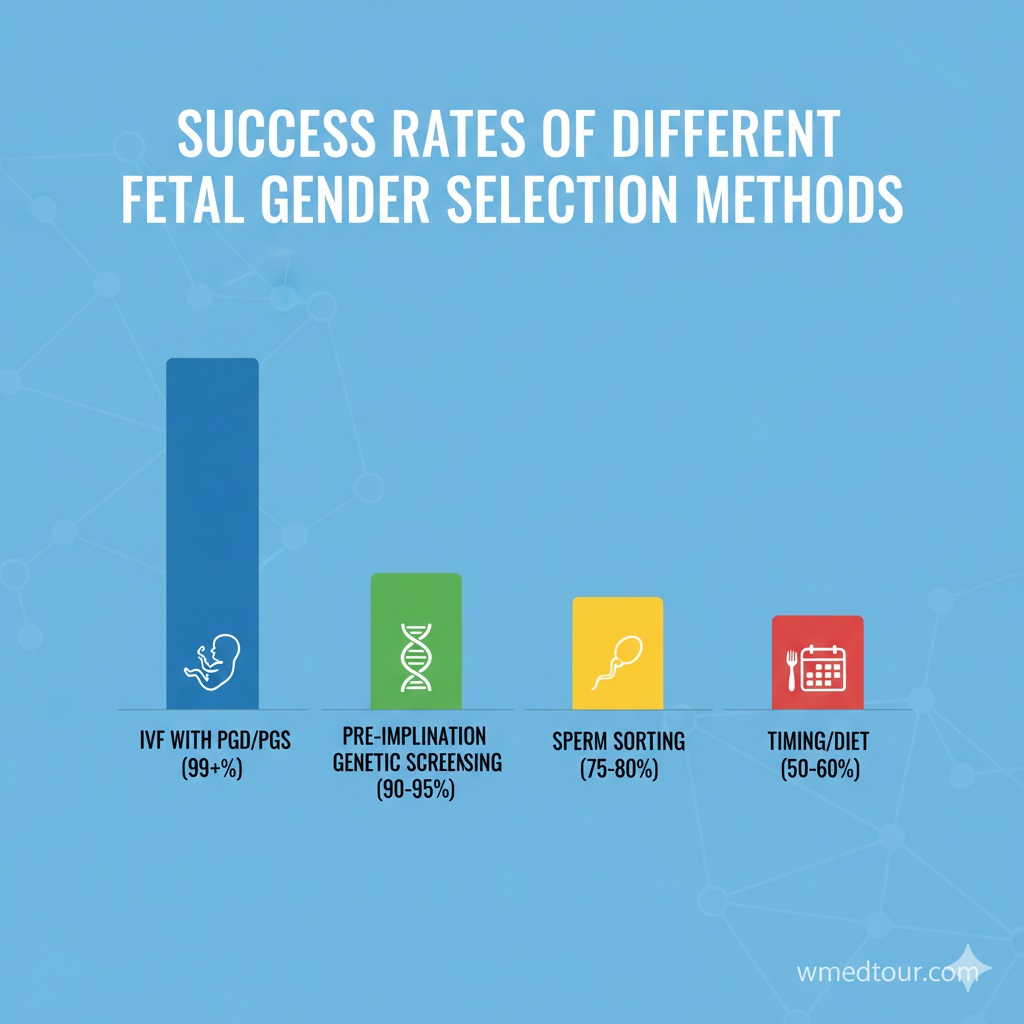
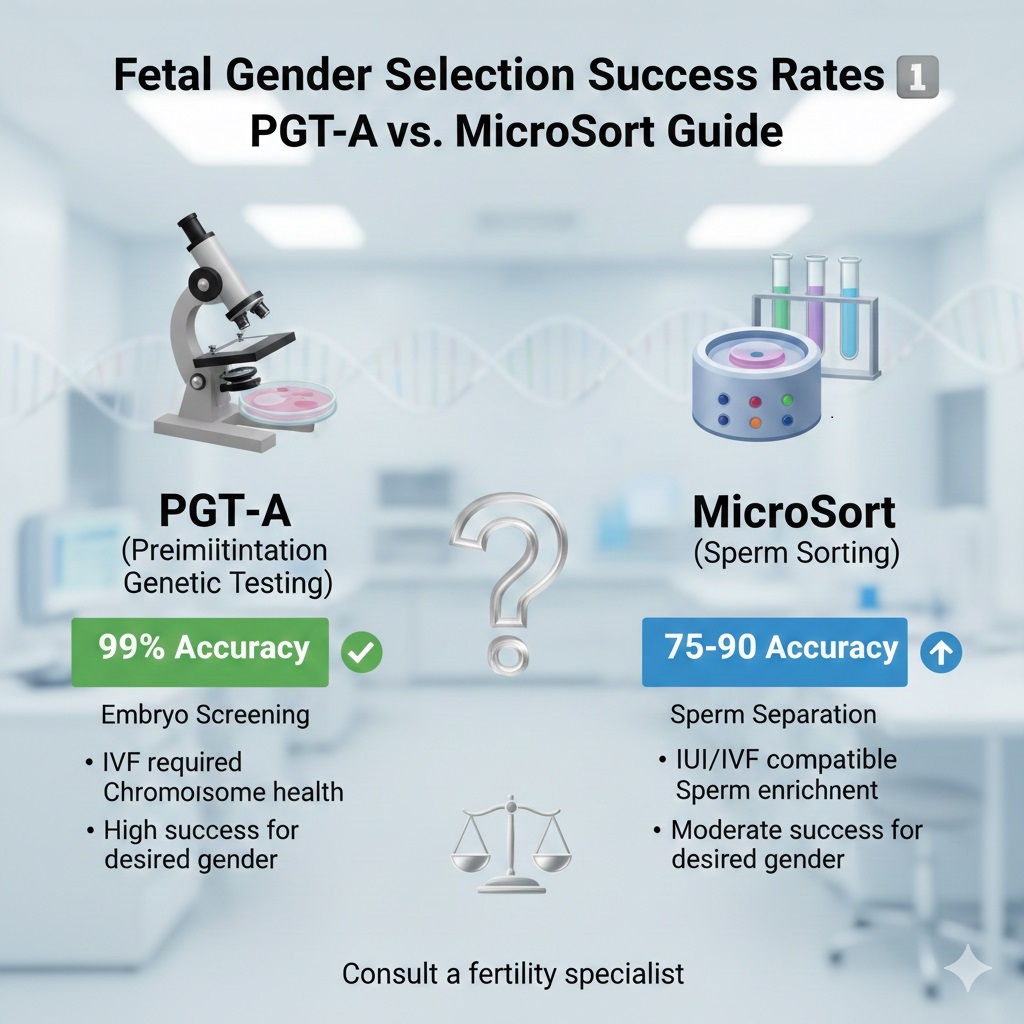
Selecting the sex of an offspring, often referred to as family balancing, is primarily achieved using two distinct methods. Consequently, this guide presents a critical analysis of the two leading pre-conception methods: Preimplantation Genetic Testing for Aneuploidy (PGT-A) and the sperm-sorting technology, MicroSort. Ultimately, PGT-A, performed during IVF, offers near-perfect, >99.9% accuracy, establishing it as the gold standard for high certainty. However, MicroSort, which sorts sperm before fertilization, provides a less invasive but significantly less accurate solution (73-93%). Therefore, understanding the legality, cost, and true Fetal Gender Selection Success Rates 2026 for each method is essential for making an informed, ethical, and successful choice, particularly when considering medical travel.
🔬 PGT-A: The Gold Standard for Near-Perfect Accuracy
Preimplantation Genetic Testing for Aneuploidy (PGT-A) is the most accurate method available for fetal gender selection. Because this technique involves genetically screening the embryo directly, it eliminates almost all ambiguity regarding the embryo’s sex. Crucially, PGT-A requires a full cycle of In Vitro Fertilization (IVF), making it a highly technical and integrated procedure. Consequently, it is the preferred method for couples with a medical need, such as avoiding severe X-linked genetic disorders, and for those prioritizing the highest possible Fetal Gender Selection Success Rates 2026 for family balancing.
⚙️ The PGT-A Process for Gender Selection
Initially, the patient undergoes ovarian stimulation, followed by egg retrieval and fertilization to create embryos in a laboratory setting. Subsequently, an embryologist performs an embryo biopsy, carefully extracting a few cells from the outer layer of the blastocyst (trophectoderm). Next, these cells are genetically analyzed. This analysis not only determines the number of chromosomes (checking for aneuploidy, which reduces miscarriage risk) but also, critically, identifies the sex chromosomes (XX or XY). The PGT-A testing process ensures that only the chromosomally normal embryo of the desired gender is transferred back into the uterus.
📈 PGT-A Success Rates: Beyond Gender
The genetic certainty of the selected embryo is the primary advantage of PGT-A. The accuracy for gender identification is nearly flawless, resting at >99.9%. However, it is vital to differentiate gender accuracy from the overall live birth rate. Therefore, the final live birth success rate is determined by the patient’s age, the clinic’s proficiency, and the embryo’s quality. The PGT Fetal Gender Selection Guide offers more details on these variables.
👍 Pros of PGT-A
- ✅ Near-Perfect Gender Certainty: The Fetal Gender Selection Success Rates 2026 for gender identification are essentially 100% for the specific embryo transferred.
- ✅ Comprehensive Health Screening: Moreover, PGT-A simultaneously screens for chromosomal abnormalities (aneuploidy), thereby increasing IVF efficiency and reducing the risk of miscarriage significantly.
- ✅ Optimal Embryo Selection: Consequently, it allows for the selection of the healthiest and most viable embryo, leading to higher overall pregnancy rates per transfer.
- ✅ Medical Necessity: Furthermore, it is the only reliable method for preventing the transmission of X-linked diseases.
👎 Cons of PGT-A
- ❌ High Invasiveness: Since it necessitates a full IVF cycle, it requires extensive medication and a surgical egg retrieval procedure for the woman.
- ❌ Significant Cost: As a result, the combined cost of IVF and PGT-A makes it the most expensive gender selection option. The cost of fetal gender selection 2025 remains a major factor.
- ❌ Ethical and Legal Hurdles: Moreover, PGT-A for non-medical reasons (family balancing) is strictly prohibited in most Western countries, necessitating medical travel. Understanding the legal landscape is paramount.
🧪 MicroSort: The Sperm Sorting Alternative
MicroSort is a pre-conception method that aims to increase the concentration of X-bearing (female) or Y-bearing (male) sperm in a sample before fertilization. Therefore, it is less invasive, particularly when paired with Intrauterine Insemination (IUI), thus avoiding the full IVF cycle required by PGT-A. However, this simplicity comes at the expense of accuracy, a key factor when evaluating Fetal Gender Selection Success Rates 2026.
🧬 The MicroSort Mechanism and Limitations
The technique leverages the fact that X chromosomes are significantly larger than Y chromosomes, meaning X-bearing sperm contain approximately 2.8% more DNA than Y-bearing sperm. To exploit this difference, sperm are stained with a fluorescent dye that binds to the DNA. Subsequently, a flow cytometer passes the sperm, one by one, through a laser. X-bearing sperm glow brighter and are sorted into a separate collection tube using an electrical charge. However, this physical sorting is not perfectly efficient, and thus, the sorted sample always contains a mix of both X and Y sperm, leading to the lower success rates discussed below.
📉 MicroSort Success Rates: The Trade-off
MicroSort’s Fetal Gender Selection Success Rates 2026 reflect the inherent limitations of physical sorting:
- For Female Selection (X-bearing sperm): Accuracy is typically around 90-93%.
- For Male Selection (Y-bearing sperm): Conversely, accuracy is lower, typically around 73-77%.
Therefore, while MicroSort significantly skews the odds, it offers no guarantee. Moreover, the overall pregnancy success rate is dependent on the subsequent procedure used, whether it is IUI or ICSI.
👍 Pros of MicroSort

- ✅ Less Invasive: Especially when combined with IUI, it avoids the extensive procedures required for PGT-A/IVF.
- ✅ Lower Cost (with IUI): Consequently, it is a more budget-friendly option than the full PGT-A/IVF combination.
- ✅ Ethical Preference: Because no embryos are screened or discarded, some couples find it ethically preferable. Comparing gender selection methods on ethics is crucial.
👎 Cons of MicroSort
- ❌ Low Certainty: The accuracy range (73-93%) means a high chance of not achieving the desired gender on the first try, which may necessitate multiple cycles.
- ❌ No Genetic Screening: Unlike PGT-A, it provides no information on the embryo’s chromosomal health, thus not reducing aneuploidy-related miscarriage risk.
- ❌ Limited Availability: MicroSort is not widely available globally due to regulatory challenges.
📋 PGT-A vs. MicroSort: A Direct Comparison Table
To help you quickly assess the core differences, the table below synthesizes the crucial data points regarding Fetal Gender Selection Success Rates 2026, costs, and clinical implications.
| Feature | PGT-A (Embryo Screening) | MicroSort (Sperm Sorting) |
|---|---|---|
| Gender Selection Accuracy | >99.9% (Near Perfect) | Female: 90-93%; Male: 73-77% |
| Required Procedure | Full IVF Cycle + Biopsy | IUI or IVF/ICSI |
| Genetic Health Screening | Yes (Aneuploidy) | No |
| Invasiveness for Woman | High | Low (with IUI) to Moderate (with IVF) |
| Relative Cost | Highest | Moderate (Lower upfront cost) |
🌎 The Global Landscape: Why International Travel is Often Necessary
The high reliability of PGT-A for achieving specific Fetal Gender Selection Success Rates 2026 has intensified the ethical debate surrounding non-medical sex selection. Consequently, many major nations, including Canada, the UK, and Australia, impose strict bans on PGT-A for non-medical family balancing. Therefore, individuals seeking these high-accuracy services often turn to international medical tourism. As a result, the choice of clinic and country is critical, requiring meticulous research into both quality and local laws. You must choose a reputable clinic and understand the global medical treatment regulations.
🇮🇷 Iran: A Leading Destination for Advanced Fertility Care
Specifically, Iran has rapidly emerged as a prominent destination for advanced fertility treatments, including high-quality PGT-A services. The country’s commitment to modern medical infrastructure, competitive pricing, and experienced specialists in gynecology and fertility makes it a highly viable option for international patients. For this reason, couples seeking reliable Fetal Gender Selection Success Rates 2026 often choose Iran, where the procedure is managed within specific legal and ethical frameworks that prioritize patient safety and choice. Detailed information on medical tourism in Iran is available. However, patients must also understand the medical travel visa process before planning their journey.
In contrast, countries like Germany and Turkey, while excellent for overall medical tourism, have differing regulations regarding elective gender selection. Medical travel to Germany and medical travel to Turkey require careful verification of current gender selection policies.
🎯 Who is This Guide For?
Understanding the variance in Fetal Gender Selection Success Rates 2026 is vital for several groups of individuals and professionals:
- Couples Seeking Family Balancing: Parents who already have children of one gender and seek the high certainty of PGT-A for a child of the other gender. PGT-A is the most effective method here, provided they can access it legally.
- Carriers of Sex-Linked Diseases: Absolutely, PGT-A is mandatory for couples who need to prevent the inheritance of conditions like Hemophilia or Muscular Dystrophy, which are linked to the sex chromosomes.
- Patients Already Undergoing IVF: If a couple is already pursuing IVF for infertility, adding PGT-A provides a dual benefit—gender selection (where legal) and aneuploidy screening—for a relatively marginal additional cost.
- Those Prioritizing Non-Invasiveness: Individuals who strongly prefer to avoid the full IVF procedure might choose MicroSort combined with IUI, even though they must accept the lower success rates.

Exploring the medical methods and complex ethical landscape of Fetal Gender Selection worldwide.
📝 Case Study: Maximizing Success with PGT-A
Consider the experience of Sarah and Adam. They had two sons and deeply desired a daughter for family balancing. Because their primary goal was a high-certainty outcome, they immediately recognized PGT-A was the appropriate method, given its high Fetal Gender Selection Success Rates 2026. They traveled to an internationally accredited clinic in Iran, which is known for advanced PGT-A services. After undergoing an IVF cycle, 15 eggs were retrieved, resulting in 7 healthy embryos. Subsequently, PGT-A analysis revealed 4 embryos were chromosomally normal, two of which were female. Following mandatory counseling and informed consent, they transferred one healthy female embryo. Ultimately, Sarah achieved a successful pregnancy, welcoming a healthy baby girl. This case demonstrates the necessity of utilizing PGT-A when gender certainty is the absolute priority, despite the invasiveness and travel involved.
❓ Frequently Asked Questions (FAQ) About Gender Selection Success
We address the most crucial questions regarding the accuracy and efficacy of PGT-A and MicroSort. Furthermore, we urge patients to research Fetal Gender Selection Risks and Success Rates thoroughly.
1. Is PGT-A for gender selection available in the United States for non-medical reasons?
In short, access varies widely by clinic and state, as there is no universal federal ban. However, many reputable clinics follow ethical guidelines established by the American Society for Reproductive Medicine (ASRM), which advises against sex selection for non-medical reasons, thus making it difficult to find.
2. Why is MicroSort accuracy lower for male selection (Y-sperm)?
The physical difference is the key. Y-sperm, carrying the smaller Y chromosome, has only about 2.8% less DNA than X-sperm. Because this difference is very small, the technology has more difficulty separating the two populations cleanly, consequently leading to a lower purity rate for Y-sperm samples.
3. Does using PGT-A reduce the number of embryos available for transfer?
Yes, but for a positive reason. PGT-A only removes cells for testing, not the embryo itself. However, it identifies embryos that are aneuploid (chromosomally abnormal) or of the undesired sex, which would have failed to implant or resulted in a miscarriage anyway. Therefore, it reduces the number of embryos transferred, not the number of healthy, viable embryos available.
4. Can MicroSort be combined with IVF instead of IUI?
Absolutely. In fact, combining MicroSort with IVF/ICSI (Intracytoplasmic Sperm Injection) is often done to maximize the chance of pregnancy per cycle, even though this increases the cost and invasiveness. However, the overall gender accuracy remains limited by the MicroSort technique itself.
5. What is the main ethical concern about PGT-A for family balancing?
The primary concern revolves around two points: the morality of discarding healthy embryos of the undesired sex, and, subsequently, the potential for exacerbating societal gender bias or creating a “designer baby” culture. The ethics guide explores this deeply.
6. How long does a full PGT-A cycle take from start to embryo transfer?
Typically, the stimulation and retrieval phase takes about two weeks. Following this, the embryos develop for five to six days, and the PGT-A lab analysis takes an additional 7 to 14 days. Therefore, the entire process, leading up to a frozen embryo transfer, generally spans 4 to 6 weeks.
7. Is MicroSort a guaranteed way to avoid X-linked genetic diseases?
No, it is not guaranteed. Although MicroSort significantly enriches the sperm sample, its accuracy is imperfect. Therefore, to guarantee avoiding a disease carried on the X chromosome, PGT-A remains the only scientifically reliable method, as it tests the final embryo.
8. If I have unexplained infertility, should I still choose PGT-A over MicroSort?
Often, yes. Because PGT-A requires IVF, which is highly effective for many forms of infertility, and simultaneously screens for genetic issues, it offers the best chance for both pregnancy and gender selection. In contrast, MicroSort with IUI has lower overall pregnancy success rates. Addressing fertility problems abroad often begins with IVF.
9. Are the embryos subjected to PGT-A suitable for freezing and future use?
Yes. Generally, embryos undergo a biopsy, are immediately frozen (cryopreserved), and stored until the PGT-A results are available. Subsequently, any remaining, healthy embryos of the desired or another sex can be stored indefinitely for future family planning.
10. How does the age of the mother affect PGT-A success for gender selection?
Maternal age is a dominant factor. Although PGT-A accuracy for gender remains high, the probability of producing a chromosomally normal embryo of the desired sex decreases significantly with advanced maternal age. Therefore, a younger patient typically requires fewer IVF cycles to find a healthy, desired-sex embryo.
11. What is the likelihood of needing multiple MicroSort cycles for success?
The likelihood is higher than with PGT-A. Because MicroSort only enriches the sperm, and IUI has lower pregnancy rates per cycle than IVF, many couples require 3 to 6 IUI/MicroSort cycles to achieve both a pregnancy and the desired sex. In comparison, PGT-A typically achieves gender selection in one IVF cycle.
12. Can Non-Invasive Prenatal Testing (NIPT) replace PGT-A for gender selection?
No. NIPT is a screening tool used during pregnancy to check for fetal anomalies and sex. However, gender selection must occur before the embryo is implanted. Therefore, NIPT serves as confirmation of gender after conception, not as a method of pre-conception selection.
💡 Conclusion: Finalizing Your Decision
Ultimately, the choice between PGT-A and MicroSort for achieving desired Fetal Gender Selection Success Rates 2026 hinges on a clear assessment of priorities. If near-perfect gender certainty and the highest chance of a healthy embryo transfer are your goals, then PGT-A is the superior method, despite its higher cost and invasiveness. Conversely, if minimizing intervention and cost are paramount, then MicroSort offers a reasonable, albeit less accurate, alternative. We strongly recommend that you seek guidance from a fertility specialist and genetic counselor, especially when navigating the complex legal and ethical pathways of international treatment. Consult our Pre-Conception Gender Selection Guide for your next steps.