For Which Diseases is Bone Marrow Transplant Beneficial? 🩸 A Comprehensive Guide
Executive Summary: Key Takeaways
A Bone Marrow Transplant (BMT), also known as a Hematopoietic Stem Cell Transplant (HSCT), offers a potentially curative treatment for numerous life-threatening conditions, primarily those affecting the blood and immune system. Specifically, we examine the major disease categories where bone marrow transplant is beneficial. These include malignant blood cancers like Acute and Chronic Leukemias, Lymphomas, and Multiple Myeloma. Furthermore, BMT is a vital intervention for non-malignant disorders such as Aplastic Anemia, Thalassemia, and Sickle Cell Disease. Finally, specific inherited metabolic and immunodeficiency syndromes, like Severe Combined Immunodeficiency (SCID), also find hope in this procedure. Successfully navigating BMT requires comprehensive pre-transplant preparation, a clear understanding of the risks, and a commitment to post-procedure care. We strongly encourage considering the global options available, including detailed resources on oncology department services, which provide world-class BMT treatment.
Understanding for which diseases is bone marrow transplant beneficial marks the first step toward exploring a powerful, often life-saving medical procedure. Bone marrow, the spongy tissue inside your bones, produces hematopoietic stem cells—the precursors to all blood cells: red cells, white cells, and platelets. When a disease damages these stem cells or requires the destruction of the existing, faulty blood-forming system, a BMT becomes necessary. Consequently, the procedure replaces damaged or diseased marrow with healthy stem cells, restoring the body’s ability to produce normal blood cells and immune function. Moreover, many patients pursuing this complex treatment often seek comprehensive guidance, which can range from understanding the procedure itself to exploring options for travel and recovery. For deeper procedural information, reading our comprehensive article on what is bone marrow transplant (BMT): types, risks, and recovery proves highly informative.
This authoritative guide clearly breaks down the spectrum of conditions where this specialized treatment provides the best, and sometimes the only, chance for a cure. It’s an essential resource for patients, caregivers, and medical professionals alike.
1. 🔬 The Core Mechanism: Why BMT Works for Specific Diseases
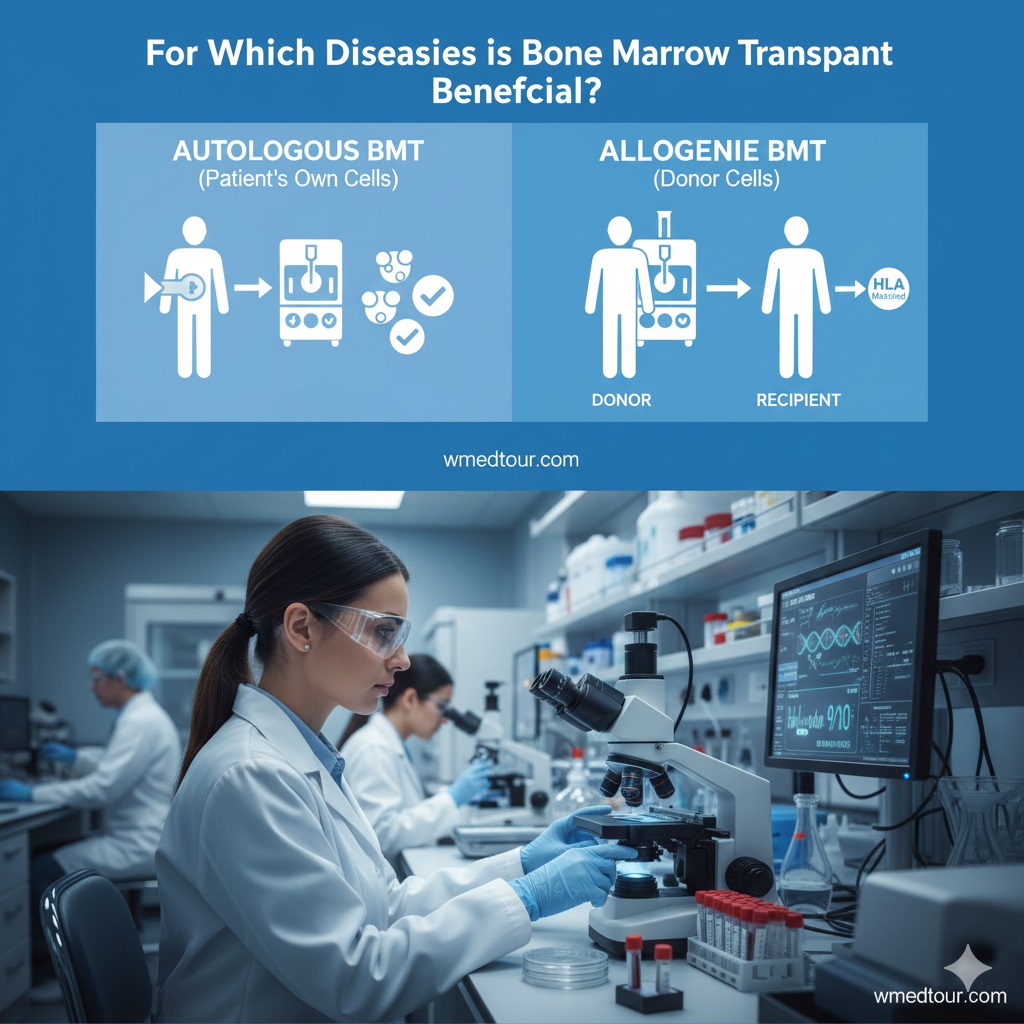
Before detailing the list of conditions, it is crucial to understand the fundamental principle behind BMT. In essence, the treatment corrects a deficiency or destroys a malignancy at the source. Thus, the stem cells, whether harvested from the patient (autologous) or a donor (allogeneic), must be transplanted to repopulate the recipient’s entire blood-forming system. Furthermore, this process necessitates a conditioning regimen, typically high-dose chemotherapy and/or radiation, to eliminate the diseased cells and suppress the recipient’s immune system to prevent rejection. The effectiveness of BMT, therefore, relies heavily on this systemic replacement and immune reset. In fact, many medical centers offer specific BMT treatments, such as the allogeneic BMT from a relative, which highlights the varied approaches to sourcing stem cells.
BMT Types and Their Primary Roles
The type of transplant usually dictates the kind of disease it targets. For instance, **Autologous BMT**, which uses the patient’s own stem cells, generally treats cancers like Multiple Myeloma or Lymphoma. The goal here is to enable the patient to tolerate extremely high doses of chemotherapy, not to introduce a new immune system. On the other hand, **Allogeneic BMT** utilizes donor cells and is vital for genetic disorders or cancers that require a “graft-versus-tumor” (GVT) effect, where the donor’s immune cells actively seek out and destroy residual cancer cells.
[Image of Bone Marrow Transplant Procedure]2. 🩸 Malignant (Cancerous) Blood Disorders: Where BMT Excels
Malignant hematologic diseases constitute the largest category where bone marrow transplant is beneficial. The high-dose chemotherapy and radiation used in conditioning often eliminate residual cancer cells that standard chemotherapy missed. Furthermore, the allogeneic transplant adds the powerful GVT effect, offering an immunological punch against the malignancy. Consequently, BMT acts as both a potent chemotherapy delivery vehicle and an immune therapy.
Acute Leukemias: Aggressive Targets
Acute Leukemias, including Acute Myeloid Leukemia (AML) and Acute Lymphoblastic Leukemia (ALL), are primary indications for BMT, particularly when the patient is in remission but faces a high risk of relapse. Specifically, BMT becomes essential because these cancers originate directly in the bone marrow. Therefore, a stem cell transplant is the most effective way to eliminate the malignant clone and permanently repopulate the marrow with healthy cells. We recognize that finding specialized care for complex cases is crucial, and centers offering advanced hemato-oncology treatment are frequently sought by patients globally.
Pros and Cons for Acute Leukemias Treatment

Chronic Leukemias and Myeloproliferative Neoplasms (MPNs)
Chronic Myeloid Leukemia (CML) and other MPNs, while often managed initially with targeted therapies, may progress or become resistant to treatment. In these situations, BMT provides a curative option. Additionally, conditions like Myelodysplastic Syndromes (MDS) often transform into acute leukemia; therefore, BMT offers preemptive intervention, preventing life-threatening progression. Considering the complexity, patients often weigh various factors, including cost, by looking into resources like the cheapest country for cancer treatment in 2025.
Lymphomas (Hodgkin and Non-Hodgkin)
For aggressive or relapsed lymphomas, BMT is a standard treatment option. Typically, an autologous transplant is preferred for patients who have achieved remission but whose disease has a high chance of recurrence. The purpose is to allow for mega-doses of chemotherapy. However, allogeneic BMT is sometimes utilized for relapsed Hodgkin Lymphoma or specific refractory Non-Hodgkin Lymphoma subtypes, providing that immune system reset. It is important to note that BMT is often used as a consolidation step following initial treatment phases, demonstrating its critical role in advanced cancer care. Moreover, new cellular therapies like TCR T-cell receptor therapy are constantly being explored as alternatives or complementary treatments.
Multiple Myeloma
Multiple Myeloma, a cancer of plasma cells, frequently uses autologous BMT as a component of first-line therapy, particularly after induction chemotherapy. The transplant significantly prolongs remission and overall survival for eligible patients. Consequently, it has become an integrated standard of care, maximizing the depth of response to the initial chemotherapy. Patients and their families must familiarize themselves with the full spectrum of treatment options available for this specific cancer, often found in dedicated resources covering the oncology department services.
Pros and Cons for Autologous BMT in Myeloma
3. 🩸 Non-Malignant (Non-Cancerous) Blood Disorders
Though often associated with cancer, a significant number of non-malignant, inherited, or acquired blood disorders are perfectly suited for BMT, as they fundamentally stem from faulty blood-forming stem cells. The goal in these cases is solely curative: to replace a defective hematopoietic system with a healthy one. Consequently, BMT transforms a chronic, life-long management problem into a potential one-time fix. [Image of different types of blood cells produced by bone marrow]
Severe Aplastic Anemia (SAA)
In Severe Aplastic Anemia, the bone marrow simply stops producing enough blood cells, often due to an autoimmune attack on the stem cells. BMT, especially from a matched sibling donor, represents the most successful and established treatment option, offering excellent long-term survival rates. The introduction of donor stem cells effectively resets the manufacturing plant. This procedure is critical for ensuring the patient has a functional, self-sustaining blood system.
Pros and Cons for Aplastic Anemia Treatment
Inherited Hemoglobinopathies: Thalassemia and Sickle Cell Disease
These two genetic disorders involve defects in the hemoglobin molecule, leading to chronic anemia, organ damage, and a drastically reduced quality of life. BMT is curative, as it replaces the defective stem cells producing the faulty hemoglobin with donor cells that produce normal, healthy hemoglobin. Patients considering this path often need extensive counseling and pre-procedure preparation, which often starts with a comprehensive health checkup to assess overall health.
Thalassemia Major
For patients with Thalassemia Major, who require lifelong, repeated blood transfusions and resulting iron overload, BMT provides a complete cure, eliminating the need for further transfusions or chelation therapy. However, the timing of the transplant, ideally performed in childhood before major organ damage occurs, is paramount to success. This consideration means that families must often act quickly when exploring options, including specialized centers overseas, which requires understanding logistical elements like securing a medical visa.
Sickle Cell Disease (SCD)
SCD, characterized by painful vaso-occlusive crises and chronic organ damage, is also curable with BMT. Although less frequently performed than BMT for Thalassemia, its success rate, especially in pediatric patients, is prompting wider application. Consequently, it shifts the focus from managing severe, episodic pain to focusing on long-term recovery and health maintenance.
Other Inherited Bone Marrow Failure Syndromes
Other conditions, like Fanconi Anemia and Shwachman-Diamond Syndrome, also lead to bone marrow failure and a high risk of developing leukemia. For these patients, BMT is a critical intervention, not just to correct the marrow failure but also to reduce the probability of malignant transformation. This preventative and curative dual action makes BMT an indispensable tool in pediatric hematology.

4. ✨ Inherited Immunodeficiency and Metabolic Disorders
Beyond the blood cells themselves, certain genetic disorders affecting the immune system or the body’s metabolism are also treated successfully with BMT. This is because hematopoietic stem cells are also the origin of all immune cells, and in some cases, can deliver missing enzymes to other parts of the body.
Severe Combined Immunodeficiency (SCID)
SCID, often called “Bubble Boy Disease,” results from a congenital defect in T- and B-lymphocyte function. Without a functioning immune system, these children face extreme vulnerability to infections. BMT is a complete cure, offering these infants a chance at a normal life. In fact, early diagnosis and treatment with BMT are crucial for survival. This is perhaps one of the clearest examples of for which diseases is bone marrow transplant beneficial in a pediatric context; for more on related topics, see our guide on pediatric cancer early signs.
Inborn Errors of Metabolism (IEMs)
Specific IEMs, such as Mucopolysaccharidosis (MPS, like Hurler Syndrome) and Adrenoleukodystrophy (ALD), can cause severe neurological damage due to the buildup of toxic substances. Furthermore, donor hematopoietic stem cells successfully engraft and differentiate into cells (like microglia in the brain) that produce the missing enzyme. This halts or slows disease progression, fundamentally altering the patient’s prognosis. Therefore, BMT represents an effective form of cellular enzyme replacement therapy for these conditions.
Pros and Cons for Inherited Disorders Treatment
5. 📊 Comparison of BMT Applications and Success Factors
Understanding which condition receives which type of BMT is essential for anticipating outcomes and risks. Furthermore, successful BMT hinges on factors like patient age, disease stage, and the quality of the Human Leukocyte Antigen (HLA) match. Consequently, evaluating all these elements helps define the likelihood of a successful engraftment and recovery.
The Role of HLA Matching
The success of allogeneic BMT depends critically on finding a suitable donor, generally involving a high-resolution HLA match. Consequently, patients without a matched sibling may require a search for an unrelated donor (MUD) or consider alternative sources, such as cord blood or haploidentical donors, which offer a partial match. The availability of resources like haploidentical BMT options ensures that more patients have access to this life-saving treatment.
Comparison Table: BMT Applications by Disease Category
| Disease Category | Primary Indication | Preferred BMT Type | Primary Goal |
|---|---|---|---|
| Acute Leukemias (e.g., AML, ALL) | High-risk/Relapse | Allogeneic | Graft-versus-Tumor (GVT) Effect & New Marrow |
| Multiple Myeloma | First Remission/Consolidation | Autologous | Intense Chemotherapy Delivery |
| Severe Aplastic Anemia | Marrow Failure | Allogeneic | Marrow Repopulation |
| Thalassemia/Sickle Cell Disease | Genetic Hemoglobin Defect | Allogeneic | Genetic Correction/Cure |
| SCID/MPS (Metabolic) | Immune/Enzyme Deficiency | Allogeneic | Enzyme or Immune System Restoration |
6. 🗺️ The Patient Journey: A Case Study in Thalassemia
To illustrate the clinical application of BMT, consider the hypothetical journey of a young patient. This narrative highlights the transformative power of knowing for which diseases is bone marrow transplant beneficial.
Case Study: Layla, 7, with Thalassemia Major
Layla, a seven-year-old girl, lived with Thalassemia Major in a location where specialized care was difficult to access. She required blood transfusions every three weeks, and chelation therapy for iron overload, which severely impacted her schooling and energy levels. After consulting with a specialist who affirmed that Thalassemia Major is one of the diseases for which bone marrow transplant is beneficial, her family sought options abroad, specifically in a center known for pediatric hematology excellence. Initially, they found a 10/10 matched sibling donor, which offered the highest chance of success. The family utilized resources like the global medical tourism guide to plan their journey. Following pre-transplant conditioning, Layla received her sibling’s stem cells. Her engraftment, the process where the new cells took root, was smooth, though the first 100 days were intensely monitored to mitigate risks like GVHD. Six months post-BMT, Layla’s blood work showed normal hemoglobin levels and she was transfusion-independent. She returned home one year later, cured of the condition that had dominated her young life, successfully illustrating the life-changing impact of BMT.
7. 👤 Who is This For? Defining the Ideal BMT Candidate
The patient profile for BMT is highly specific. This treatment is generally reserved for patients with life-threatening hematologic or immune disorders who meet stringent criteria. Essentially, the procedure is an intense intervention with significant risks; therefore, the potential for cure must clearly outweigh these risks. Consequently, the suitability is determined by a multidisciplinary team.
Key Candidate Criteria
- Disease Status: For cancers, the patient should ideally be in first or second complete remission. For non-malignant disorders, the disease must be progressive or severe enough to justify the transplant risk.
- Organ Function: The patient must have adequate heart, lung, liver, and kidney function, as the conditioning chemotherapy is toxic to these organs.
- Age: Younger patients generally tolerate BMT better. Although age limits have been extended, excellent physiological health remains paramount.
- Donor Availability: Access to a high-quality, matched donor is a critical factor for allogeneic BMT success.
Patients and their families must undertake thorough research and preparation. This includes understanding the potential need for other complex procedures, such as kidney transplantation in cases where the disease has already caused organ failure, or related general surgery procedures in the transplant surgery category.
8. 🛡️ Risks, Challenges, and Navigating the BMT Process
While we emphasize for which diseases is bone marrow transplant beneficial, it is also important to address the challenges. BMT is one of the most intensive medical procedures available. Therefore, understanding the risks is as crucial as understanding the benefits. Many patients explore international options for access to specialized care, which requires pre-travel planning and logistics, often detailed in a medical travel guide.
The Conditioning Regimen: Clearing the Way
The high-dose chemotherapy and radiation administered before the transplant (conditioning) effectively destroy the remaining diseased marrow. Furthermore, this intense therapy eradicates cancer cells and creates space for the new donor cells. However, this process also causes significant side effects, including severe nausea, fatigue, mucositis (painful mouth and throat sores), and temporary infertility. This phase is challenging, thus requiring expert supportive care.
Graft-versus-Host Disease (GVHD): The Immune Conflict
GVHD is the major complication of allogeneic BMT. In this condition, the newly transplanted donor immune cells recognize the recipient’s body as foreign and attack it. Symptoms can range from mild skin rashes to severe damage in the liver, gut, and lungs. Consequently, managing GVHD requires a delicate balance of immunosuppressive drugs to control the reaction while preserving the beneficial graft-versus-tumor (GVT) effect. New techniques, such as those used in allogeneic BMT from a non-relative, are constantly refining this balance.
Infection and Relapse: Post-Transplant Monitoring
In the months immediately following BMT, the patient is highly vulnerable to bacterial, viral, and fungal infections due to their suppressed immune system. Subsequently, the first year is dedicated to intense monitoring and prophylactic medication. On the other hand, for malignant diseases, the risk of relapse remains a concern; consequently, continuous surveillance, often involving advanced diagnostics like CTC liquid biopsy, is crucial for early detection and intervention.
9. ❓ Frequently Asked Questions (FAQ) About BMT Indications
When considering BMT, patients and caregivers frequently ask specific questions about the eligibility and success of the procedure for various diseases. Here are some of the most important, detailed answers.
1. Can a bone marrow transplant cure Acute Myeloid Leukemia (AML)? Yes, BMT, particularly allogeneic BMT, offers the highest probability of cure for AML patients, especially those who are in first complete remission and have high-risk disease features. It works by replacing the diseased cells and utilizing the donor’s immune system to eliminate residual leukemia.
2. Is BMT necessary for all types of Lymphoma? No, BMT is generally reserved for aggressive or relapsed lymphomas that have not responded adequately to standard first-line chemotherapy. Autologous BMT is more common for non-Hodgkin and Hodgkin Lymphoma to allow for high-dose chemo, but allogeneic BMT may be used for specific refractory cases.
3. For which diseases is bone marrow transplant beneficial if they are genetic, like Sickle Cell Disease? BMT is highly beneficial for genetic hemoglobinopathies like Sickle Cell Disease and Thalassemia Major. It serves as a curative treatment by permanently replacing the stem cells that carry the genetic mutation with healthy, non-mutated donor cells, thus eliminating the production of faulty hemoglobin.
4. Does BMT work for Solid Tumors, like Lung or Breast Cancer? Historically, BMT was explored for solid tumors, but its use is now very limited. BMT is primarily effective for hematologic (blood) cancers and disorders. Modern cell therapies and targeted treatments are now the focus for solid tumors. For information on other types of organ transplantation, review resources on lung transplantation.
5. How is Multiple Myeloma treated with BMT? Is it curative? Multiple Myeloma is typically treated using autologous BMT, which is used to deepen the patient’s remission after initial chemotherapy. It is not considered a definitive cure but can lead to long-term remission and survival. Allogeneic BMT is sometimes used but carries greater risk.
6. What is the required age limit for a BMT? There is no strict age limit, but generally, BMT is more feasible for younger patients (under 65 or 70) due to their ability to tolerate the intensive conditioning regimen. The patient’s overall physiological health and co-morbidities are more important than chronological age.
7. Is BMT a primary treatment for Myelodysplastic Syndromes (MDS)? Yes, BMT is the only potential cure for MDS, especially for high-risk patients. Since MDS can transform into Acute Myeloid Leukemia (AML), the transplant is often performed preemptively to prevent this life-threatening transformation.
8. What role does BMT play in treating Severe Combined Immunodeficiency (SCID)? BMT is a curative treatment for SCID. The transplant introduces healthy donor stem cells that differentiate into fully functional T and B lymphocytes, effectively building an entire, functional immune system where none existed before. Early intervention is vital for a positive outcome.
9. Are there any autoimmune diseases where BMT is beneficial? Yes, autologous BMT is sometimes explored for severe, refractory autoimmune diseases like Systemic Sclerosis or Multiple Sclerosis. The goal is to “reset” the faulty immune system that is attacking the body’s own tissues. This application is less common but represents a growing area of research.
10. How can a patient find a donor for BMT? The search starts with the patient’s siblings. If no matched sibling is found, the search expands to the Unrelated Donor Registry. Advanced techniques, like haploidentical BMT (using a half-matched parent or child), offer an option when a fully matched donor is unavailable, thus expanding access to this life-saving therapy.
11. How do doctors determine if a patient with Acute Leukemia is eligible for BMT? Eligibility hinges on achieving remission, the patient’s overall fitness (performance status), the presence of favorable or unfavorable genetic markers, and their response to initial chemotherapy. A high-risk profile often makes BMT the mandatory next step.
12. What should I consider when looking abroad for BMT for my condition? When seeking BMT abroad, consider the hospital’s specific experience in treating your condition, the availability of specialized BMT units, donor matching infrastructure, and the total cancer treatment cost. Also, confirm the logistics, like the required duration of stay and post-transplant follow-up protocols.
13. Is Chronic Lymphocytic Leukemia (CLL) one of the diseases for which bone marrow transplant is beneficial? CLL is generally managed with targeted oral agents. Allogeneic BMT is reserved only for a very small subset of high-risk patients who have failed multiple lines of therapy, as it is a curative, though high-risk, last resort.
14. What other types of transplantation are available besides BMT for certain diseases? While BMT addresses blood and immune disorders, organ transplants address organ failure. For instance, severe heart failure may require heart transplant surgery. Similarly, diseases like end-stage renal failure require kidney transplantation. BMT belongs to the broader category of general surgery transplant procedures.
10. 🌍 Global Access to BMT: Exploring International Options
The complexity and cost of BMT often lead patients and their families to seek treatment in countries known for advanced medical infrastructure and specialized BMT centers. Understanding where to receive the best care is vital, particularly when searching for expertise in specific hematologic conditions. For instance, many specialized procedures are offered globally, including advanced diagnostic options and treatment protocols in hemato-oncology treatment in Iran, which draws international attention for its affordability and expertise. Therefore, the informed patient researches the reputation and success rates of international institutions.
Finding the Right Center
Selecting the best facility requires diligent research beyond just costs. Patients should vet the hospital’s experience with their specific disorder, ensuring they have an established BMT program and robust critical care support. Resources exist to guide patients in vetting potential treatment destinations and understanding the nuances of international care. For instance, detailed guides exist for patients researching global options, like those exploring medical travel to Turkey, a country increasingly recognized for its specialized oncology and transplant services. Making an informed choice ensures the best possible outcome.
The Importance of Preparation and Follow-up
International BMT requires extensive planning, encompassing the medical journey and logistical elements. Accordingly, securing the necessary medical visa and planning for the long recovery period (often several months in the destination country) are just as important as the procedure itself. Furthermore, post-transplant care is critical, requiring close monitoring and collaboration between the international center and the patient’s home country physicians. Patients must prepare for continuous surveillance to watch for signs of relapse or GVHD. Furthermore, it’s wise to review comprehensive guides on managing the travel and treatment process, such as the global medical tourism guide.
11. 📝 Final Thoughts on BMT and Disease Indications
In conclusion, the question, “for which diseases is bone marrow transplant beneficial?” has a clear answer: primarily life-threatening hematologic malignancies, marrow failure syndromes, and select genetic/metabolic disorders. Significantly, the procedure has evolved from a last resort to a standard, curative treatment for many of these conditions. Consequently, millions of lives have been saved, and the quality of life for survivors has dramatically improved. Therefore, anyone facing a diagnosis like severe Aplastic Anemia or high-risk Leukemia should thoroughly discuss BMT as a definitive treatment path with their specialist. Furthermore, considering all available options, including specialized global BMT programs, can open the door to a curative future. We encourage patients to seek comprehensive consultation and explore our dedicated services.




