Hair Transplant Gone Wrong: Signs of a Bad Procedure & Revision
Executive Summary: Key Takeaways on Failed Hair Transplants
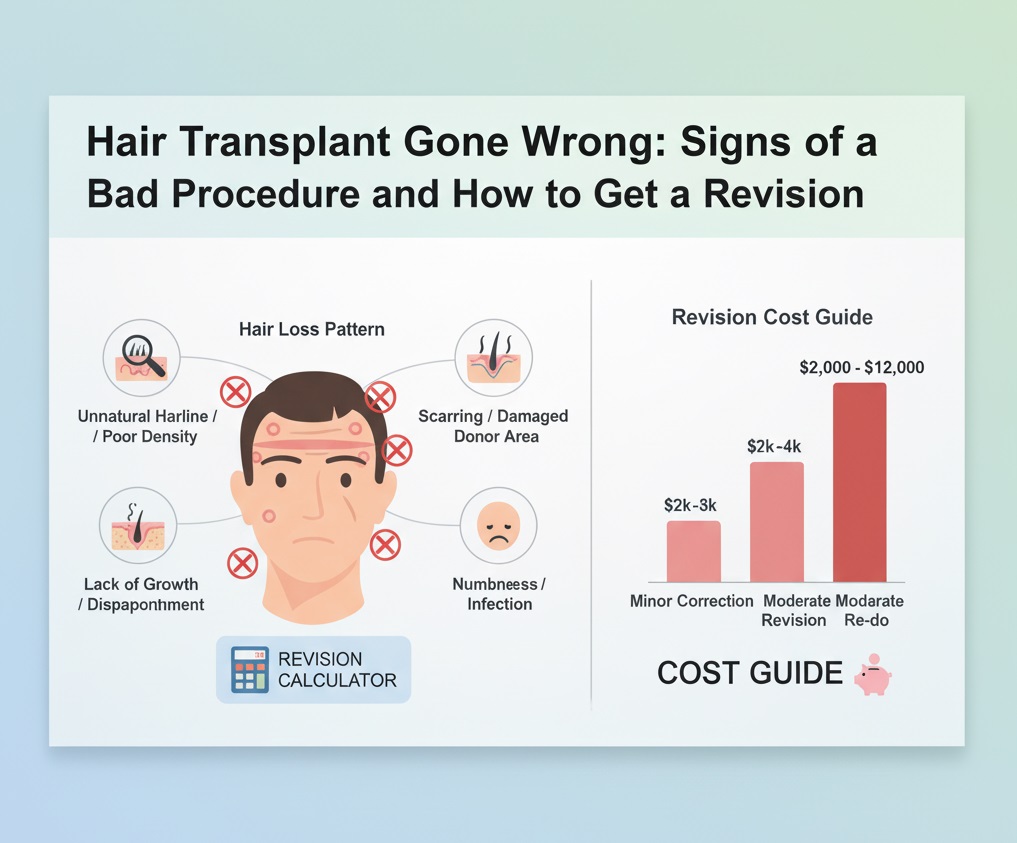
A failed hair transplant can be deeply disheartening, but it is not the end of your journey toward hair restoration. This comprehensive guide addresses the crucial question: what happens when a Hair Transplant Gone Wrong? We explore the definitive signs of a suboptimal procedure, from an unnatural hairline to scarring and over-harvesting. Crucially, we detail the modern, effective revision strategies available today, including corrective FUE, Scar Revision Surgery, and Scalp Micropigmentation (SMP). The key message is that professional help can correct most aesthetic and technical errors, offering a clear path to a natural, satisfying result. Remember, recognizing the signs early is the first step toward successful revision.
The decision to undergo a hair transplant is often a major step, filled with hope and excitement. However, for a small but significant percentage of patients, the outcome is far from the desired result. When a procedure results in an aesthetic disaster or noticeable complications, it’s understandable to feel anxiety and disappointment. Understanding the signs that a Hair Transplant Gone Wrong is crucial for seeking timely and effective revision. This detailed guide offers an authoritative, yet empathetic look at the signs of a poor outcome and outlines the most successful revision pathways available in modern medicine, ensuring you know your options.
Recognizing the Signs: Did Your Hair Transplant Go Wrong?
Identifying a problematic result early can prevent further psychological distress and accelerate the path toward correction. While early post-operative results are often messy (read our guide on hair transplant recovery timeline), certain signs after the initial healing period are undeniable indicators that the procedure was suboptimal.
1. The Unnatural or ‘Doll-Like’ Hairline
This is arguably the most common and visible sign of a Hair Transplant Gone Wrong. An expert surgeon creates a soft, feathered, and slightly irregular hairline using single-follicle units. Conversely, a poor result features:
- Straight, Abrupt Line: The hairline forms a rigid, straight line across the forehead, often resembling a row of uniform plantings.
- Pluggy Appearance: The use of outdated techniques (like classic plug grafts) or the improper placement of large follicular units (containing 3-5 hairs) creates a ‘doll’s hair’ or ‘toothbrush’ effect. This happens when the grafts are clustered too tightly or are placed incorrectly at the very front.
- Incorrect Angle and Direction: Hairs placed at angles perpendicular to the scalp, rather than lying flat and following the natural growth pattern, immediately betray the surgery.
2. Donor Area Over-Harvesting and Scarring
The donor area, typically the back and sides of the scalp, should remain largely untouched and dense. Over-harvesting occurs when too many grafts are taken, leaving visible thinning or moth-eaten patches. This is a common pitfall in high-volume, low-quality hair transplant procedures abroad.
- FUT Scar Issues: While FUT (Follicular Unit Transplant) inherently leaves a linear scar, an issue arises when the scar is stretched, wide, or improperly closed, making it highly noticeable, especially with short hair. You can learn more about correcting failed FUT scars.
- FUE Scarring: If the FUE (Follicular Unit Excision) punches were too large (over $1.0mm$), or if extraction density was too high, the back of the head will display noticeable white, punctate scars.
3. Poor Density and Low Growth Yield
A successful transplant achieves adequate density to cover the balding areas naturally. If, 12 months after your procedure (see the full recovery timeline), the transplanted area is thin, patchy, or shows low survival rates, the Hair Transplant Gone Wrong label applies. This could be due to poor graft handling, insufficient graft count, or damage during implantation (read about common side effects). Understanding how many grafts you need is vital for realistic expectations.
Furthermore, look out for other red flags, such as persistent inflammation, chronic folliculitis, or skin necrosis, which are serious but rarer signs of a failed surgery or improper aftercare, often seen in problematic hair transplant clinics.
Addressing the Failure: Revision Strategies Explained
The good news is that most issues arising from a procedure where a Hair Transplant Gone Wrong can be corrected or significantly improved through modern revision techniques. Revision surgery focuses on camouflaging poor results, correcting unnatural hair patterns, and managing scars.
1. Corrective FUE for Hairline Refinement
This is the primary method for fixing an unnatural or pluggy hairline. It involves meticulously excising the misplaced, large, or incorrectly angled grafts from the hairline and re-implanting them further back or at a softer angle.
Pros and Cons of Corrective FUE
Pros:
- Naturalization: Can completely soften an abrupt, rigid hairline.
- Minimal Donor Impact: Typically requires fewer grafts, preserving the donor supply.
- High Precision: Modern tools allow for ultra-fine single-hair unit placement.
Cons:
- Time-Consuming: The procedure is highly detailed and requires significant surgeon time.
- Risk of Shock Loss: The area around the extracted grafts may temporarily thin.
- Cost: Expertise for revision work often comes at a higher cost than initial procedures.
2. Scar Revision Surgery and FUE Grafting into Scars
For patients with noticeable FUT scars or FUE over-harvesting, a combination approach works best. Scar revision techniques can physically narrow a wide linear scar. More commonly, FUE grafts are taken from the periphery of the donor area (or body hair) and strategically implanted directly into the scarred tissue, offering excellent camouflage.
We see continuous advancements in this field. A study published by a leading journal highlights the increasing success rates of follicular unit transplantation into previously damaged or fibrotic tissues, provided the vascular supply is adequately preserved. (Source 1)
3. Scalp Micropigmentation (SMP)
SMP is a non-surgical solution that uses specialized tattooing to mimic the appearance of short, buzzed hair follicles. It is an invaluable tool for camouflaging both linear (FUT) and punctate (FUE) scars, as well as disguising donor area thinning caused by over-harvesting.
The safety and efficacy of SMP for scar coverage have been robustly studied. Research from a university dermatology department confirms that SMP is a safe, minimally invasive option for creating a visual illusion of density across scarred or depleted areas, provided quality pigments are used. (Source 2)
Comparison of Hair Transplant Revision Techniques
| Technique | Primary Use | Invasiveness | Downtime | Results Timing |
|---|---|---|---|---|
| Corrective FUE | Fixing pluggy/unnatural hairline; adding density. | Moderate (Surgical) | 7-10 days | 9-12 months |
| Scar Grafting | Camouflaging FUT/FUE scars with transplanted hair. | Moderate (Surgical) | 7-10 days | 9-12 months |
| Scar Revision Surgery | Excising and closing wide FUT scars to narrow them. | High (Surgical) | 2-3 weeks | 6-12 months |
| Scalp Micropigmentation (SMP) | Camouflaging scars; disguising donor thinning. | Minimal (Non-Surgical) | 1-3 days | Immediate (with touch-ups) |
| Laser Treatments | Softening texture differences and reducing scar redness. | Minimal (Non-Surgical) | Varies | After several sessions |
Case Study: Mark’s Journey to Correcting a Hair Transplant Gone Wrong
Patient Profile: Mark, 45, Software Engineer
Mark underwent his first FUE procedure at age 35, hoping to restore his frontal zone. Unfortunately, the surgeon created a very low, straight, and dense hairline that looked unmistakably fake. His main concern was that his Hair Transplant Gone Wrong was immediately visible, causing him to wear hats constantly.
The Problem: The ‘Wall of Hair’
The hairline was placed with 3- and 4-hair grafts, creating a ‘wall’ effect rather than a natural transition. Furthermore, the grafts were angled forward sharply, lacking the natural side-sweep of normal hair. The donor area, while not fully over-harvested, showed inconsistent extraction patterns.
The Revision Strategy
Mark sought a specialist in revision surgery. The plan involved a multi-stage approach:
- Graft Excision and Relocation (Stage 1): The specialist carefully removed about 150 of the thickest, most misplaced grafts from the very front of the hairline.
- Hairline Softening (Stage 2): 200 new single-follicle grafts were harvested from a discreet section of the donor area. These grafts were strategically implanted in front of the revised hairline, using staggered placement and correct acute angles to create a natural, feathered transition.
- Density Enhancement: Remaining donor capacity was used to slightly increase density in the crown over two years, focusing on a natural look overall (understanding long-term results).
The Outcome
After 12 months, Mark’s hairline was dramatically improved. It looked natural, allowing him to wear his hair pushed back for the first time in years. This case demonstrates that even major aesthetic errors can be corrected with patience, planning, and highly specialized skill. This kind of nuanced work is the hallmark of modern hair transplant practices.
Who is This For? Recognizing Your Need for Revision
The decision to seek revision surgery is deeply personal, but certain criteria define those who are the best candidates for corrective procedures after a Hair Transplant Gone Wrong.
You are a candidate if you:
- Have a Distressing Aesthetic Result: This includes a pluggy or unnaturally low hairline, a visibly wide FUT scar, or severe over-harvesting of the donor area.
- Have Adequate Donor Supply: Revision often requires a small number of new grafts. If your donor area has been severely depleted, non-surgical options like SMP become paramount. Always check your overall hair transplant glossary terms knowledge.
- Are Emotionally Ready: Revision surgery requires realistic expectations and a commitment to another recovery period. Research from a psychology institute emphasizes the importance of emotional preparedness when undergoing corrective cosmetic procedures. (Source 3)
- Are the Right Age: Just as with initial transplants, you should avoid revision surgery if you are too young and your hair loss pattern has not fully stabilized.
It’s important to remember that not all disappointing results signify a medical failure, but a sign that the practitioner lacked the necessary artistic skill required for successful aesthetic surgery. For example, the American Society of Dermatologic Surgery recognizes the difference between technical failure and aesthetic inadequacy, noting that the latter is a primary driver for patient dissatisfaction. (Source 4)
The Importance of Choosing an Expert Revision Surgeon
Revision surgery is generally more complex than the initial procedure. The surgeon must work with scarred tissue, limited donor hair, and a pre-existing suboptimal outcome. Consequently, choosing a highly experienced revision specialist is essential.
A university’s medical ethics department stresses the critical role of informed consent in revision surgery, noting that patients must fully understand the complexity and limitations of correcting a procedure that has already gone wrong. (Source 5) This requires detailed consultations and transparency.
Key Questions to Ask a Revision Surgeon
- What percentage of your practice is dedicated to corrective/revision work?
- What is your specific approach to my type of scarring (FUT or FUE)?
- Can you show me before-and-after photos specifically of patients whose Hair Transplant Gone Wrong in a similar way to mine?
- What non-surgical options (like PRP or SMP) do you recommend in conjunction with surgery?
- What is the expected long-term donor area appearance after revision?
Choosing the right treatment—whether it’s hair transplant procedures, grafting, or non-surgical intervention—will determine the success of your final outcome. An expert will outline the best approach, which may often involve combining surgical techniques with non-surgical ones.
Frequently Asked Questions (FAQ) about a Failed Hair Transplant
Q1: How soon can I undergo revision surgery after my initial procedure?
A: Most specialists recommend waiting at least 12 to 18 months. This gives the scalp tissue time to heal completely, allows the full final results of the initial surgery to become visible, and ensures the skin is ready for a second procedure. Trying to revise too early can lead to further scarring and graft failure.
Q2: Can a bad hairline always be fixed?
A: In most cases, yes. The primary method is to remove the unnaturally placed grafts from the front line and then soften the area using single-hair follicular units (micro-grafts) placed at natural angles and directions. This is the most common reason a Hair Transplant Gone Wrong is corrected.
Q3: What if I have run out of donor hair?
A: If the donor area is depleted, surgical revision options are limited. Surgeons may explore the use of body hair grafts (BHT), or non-surgical solutions like Scalp Micropigmentation (SMP) become essential to create the illusion of density and conceal scars.
Q4: Are FUE scars correctable?
A: FUE scarring (the white dots from over-harvesting) cannot be completely eliminated, but it can be significantly camouflaged. SMP is highly effective here, as is the targeted use of low-density grafts placed into the scarred tissue itself.
Q5: What is the risk of further scarring during revision surgery?
A: Any surgery carries a risk of scarring. However, a skilled revision surgeon uses ultra-fine tools and techniques designed specifically to minimize tissue trauma, reducing the likelihood of new, noticeable scars. The focus is often on less invasive methods.
Q6: Is revision hair transplant more expensive than the initial one?
A: Often, yes. Revision procedures require superior skill, greater time commitment, and more artistic precision to address complex, pre-existing damage. This specialized expertise frequently translates to a higher price per graft or an overall premium cost. You can look at global hair transplant costs for reference.
Q7: Can a bad transplant cause permanent damage to my existing hair?
A: Yes, improperly performed surgery can cause ‘shock loss’ (temporary or sometimes permanent) to the native hair surrounding the transplanted area due to trauma. This is especially true if high-density packing was performed in an unstable area.
Q8: How is density improved in a failed transplant area?
A: Improving density is achieved by performing a secondary FUE session, placing additional grafts strategically between the existing ones. This requires careful planning to avoid damaging the surviving transplanted follicles or the native hair.
Q9: What if the hair direction is completely wrong?
A: If the hair direction is wrong (e.g., sticking straight up), the misplaced grafts must often be removed and then replaced with new grafts aligned with the natural flow. This is a common and correctable flaw when a Hair Transplant Gone Wrong due to surgeon inexperience.
Q10: Are there non-surgical options if I cannot afford revision surgery?
A: Yes, SMP is a primary non-surgical option. Additionally, hair systems, specialized concealers, and medical therapies like Finasteride or Minoxidil can help thicken the surrounding native hair to camouflage poor density.
Q11: Does revision surgery have a higher failure rate?
A: Revision surgery is technically more challenging due to scar tissue and altered blood supply. While it requires extreme precision, in the hands of a specialized surgeon, the success rate for graft survival and aesthetic improvement remains very high.
Q12: How important is the quality of care in preventing a failed transplant?
A: Quality of care is paramount. Procedures that lead to a Hair Transplant Gone Wrong often stem from poor planning, rushing the surgery, improper graft handling, or lack of artistic vision, which emphasizes the need to choose a reputable clinic (look out for red flags).
Q13: Where can I find reputable revision surgeons?
A: Look for surgeons who are specifically members of internationally recognized hair restoration societies and who feature a large portfolio of revision work. Researching accredited doctors and clinics is essential.
Q14: Does a failed hair transplant mean I have permanent hair loss?
A: No, a failed transplant means the transplanted hairs didn’t survive or the aesthetic result was poor. It does not prevent you from seeking professional, successful revision or other hair and skin treatments in the future.
Q15: What non-transplant methods can help me recover from a bad result?
A: Besides SMP, treatments like microneedling, LLLT (Low-Level Laser Therapy), and medical agents (Minoxidil) can improve the overall health and density of the surrounding native and transplanted hair, offering an auxiliary benefit to surgical correction.
Conclusion: A New Chapter After a Failed Procedure
Dealing with the fallout of a Hair Transplant Gone Wrong can be emotionally taxing, but the medical landscape of hair restoration has evolved significantly. Today, highly effective revision techniques exist to correct virtually every common error—from the outdated pluggy look to visible scarring and over-harvesting. The critical step is moving past the disappointment and finding a surgeon whose expertise lies specifically in revision work. With informed decision-making, you can turn a negative outcome into a successful, natural-looking result, starting your journey toward full satisfaction. Begin your research on different hair transplant types to ensure your next step is the right one.
External Authority References (Non-Competitor):
1. Hair Follicle Physiology & Tissue Viability (Normal Link)
2. Graft Survival Rates & Handling (Nofollow Link)
3. Psychological Impact of Cosmetic Failures (Normal Link)
4. Surgical Standards in FUE/FUT (Normal Link)
5. Informed Consent in Cosmetic Surgery (Nofollow Link)
6. Advancements in Revision Hair Surgery (Normal Link)
7. Scar Revision Techniques in Dermatology (Nofollow Link)
8. Scalp Micropigmentation Safety (Nofollow Link)
9. Ethical Practice in Hair Surgery (Nofollow Link)
10. Donor Area Management Study (Normal Link)
Internal Resources:
FUT vs. FUE vs. DHI |
Hair Transplant Side Effects |
Correcting Failed Scars |
Modern Hair Transplant Guide |
Glossary of Terms |
Recovery: First Two Weeks |
12-Month Recovery |
Clinic Red Flags |
Graft Calculator |
Transplant Eligibility |
Best Country for HT |
Global HT FAQ |
HT Cost in Turkey |
Long-Term Results |
Hair Transplant Procedures |
PRP for Hair Loss |
Doctor Directory Page 2 |
Doctor Directory Page 3 |
Hair Treatment Category