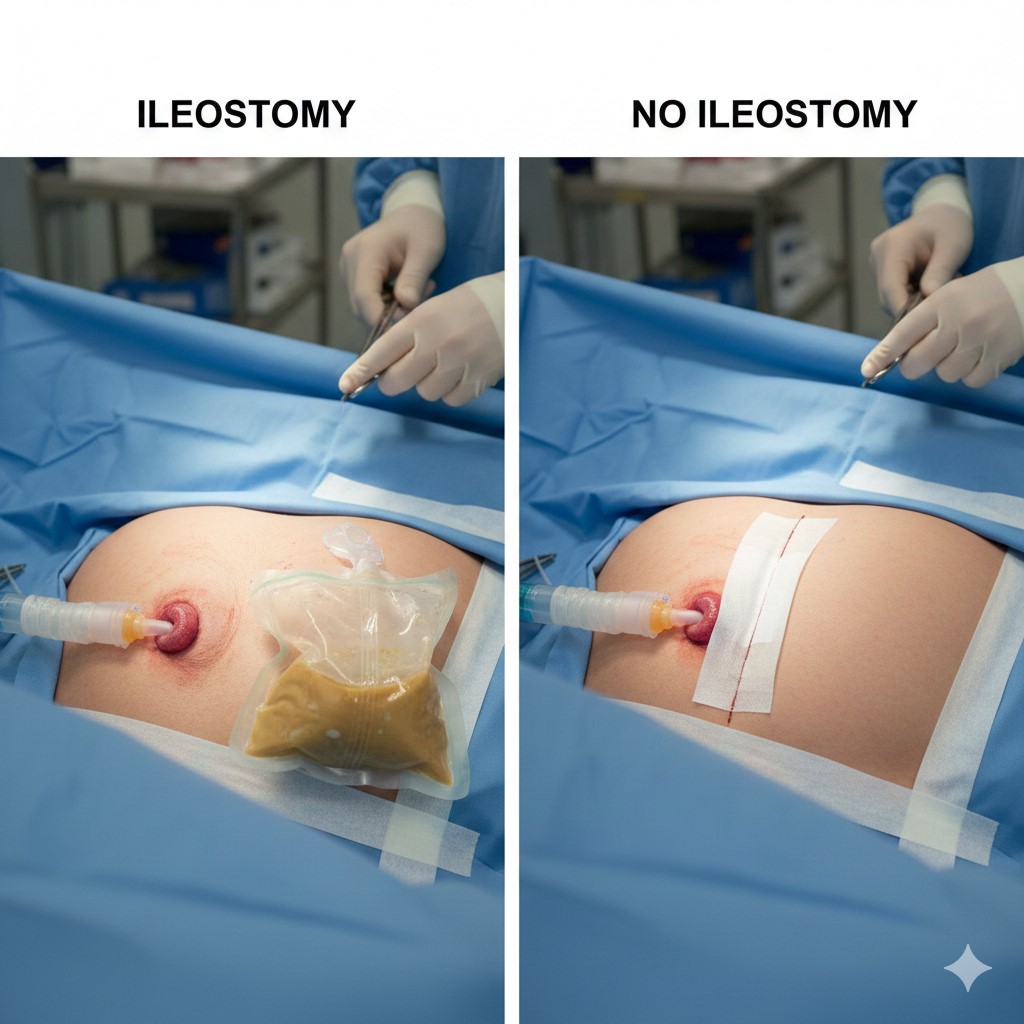
🩺 Ileostomy or No Ileostomy? What to Expect After a Colectomy
📋 Executive Summary
Deciding between ileostomy or no ileostomy is a pivotal moment for patients undergoing a colectomy. This guide clarifies the surgical paths available today. We explore the functional differences, recovery timelines, and psychological impacts of living with or without a stoma. Key takeaways include:
- ✅ Ileostomy: Often temporary, it allows the bowel to heal safely.
- ✅ No Ileostomy (Primary Anastomosis): Restores natural continuity but carries specific risks.
- ✅ Choice Factors: Diagnosis, nutritional status, and surgeon expertise are critical.
- ✅ Recovery: Modern techniques in general surgery significantly improve long-term quality of life.
🤔 Who is This For?
This comprehensive resource is designed for patients facing colon or rectal surgery. It is equally valuable for caregivers and healthcare professionals. If you are struggling with Crohn’s disease, ulcerative colitis, or colorectal cancer, this article provides clarity. We aim to replace fear with facts. Whether you are browsing our articles or preparing for a consultation, this is your primary roadmap.
🏗️ Understanding the Basics: Ileostomy or No Ileostomy?
A colectomy involves removing part or all of the large intestine. Afterward, the surgeon must decide how you will pass waste. This leads to the central question: ileostomy or no ileostomy? An ileostomy creates an opening (stoma) on the abdomen. Waste then exits into an external bag. Conversely, a “no ileostomy” outcome means the surgeon reconnects the remaining bowel. This is known as a primary anastomosis.
The choice depends on many medical variables. For instance, in gastrointestinal oncology, the location of a tumor often dictates the procedure. If the connection is very low or risky, a temporary ileostomy provides a safety net. This prevents life-threatening leaks into the abdominal cavity.
💡 The Role of Inflammation
Heavy inflammation often tips the scales. In cases of severe colitis, the tissue may be too fragile for immediate reconnection. Surgeons prioritize your safety over convenience. Consequently, an ileostomy might be the wisest short-term solution. You can learn more about these risks in our FAQ section.
📊 Side-by-Side Comparison: Ileostomy vs. No Ileostomy
| Feature | Ileostomy | No Ileostomy (Anastomosis) |
|---|---|---|
| Waste Elimination | Via an external pouch (stoma) | Via the natural rectum/anus |
| Surgical Complexity | Moderate; may require a second surgery | High; requires healthy tissue fusion |
| Risk of Leakage | Lower risk of internal infection | Higher risk of anastomotic leak |
| Lifestyle Impact | Requires appliance management | Frequent bowel movements initially |
🌟 The Pros and Cons Breakdown
🔹 Option 1: The Ileostomy Path
An ileostomy is often a life-saving bridge. Because it diverts waste, the surgical site remains clean. This is vital when the body is malnourished or weakened by chemotherapy.
- Pros: Significantly reduces the risk of sepsis. It allows the distal bowel to rest completely. It provides peace of mind during the initial healing phase.
- Cons: Requires learning stoma care. There is a potential for skin irritation around the site. A second minor surgery is usually needed for reversal.
🔹 Option 2: The No Ileostomy Path
Many patients prefer “no ileostomy” to maintain their body image. However, this path requires ideal conditions. The blood supply to the bowel must be perfect. Furthermore, the patient should not be on high-dose steroids.
- Pros: No external pouching system. Avoids the psychological hurdle of a stoma. Restores natural bowel function immediately.
- Cons: Risk of an anastomotic leak (a surgical emergency). Potential for “LARS” (Lower Anterior Resection Syndrome). Increased urgency and frequency of bathroom visits.
🛣️ The Patient Roadmap: What to Expect
Navigation through surgery involves several stages. First, you will have a pre-operative consultation. During this time, the surgeon assesses your anatomy. They will discuss the likelihood of ileostomy or no ileostomy based on your specific scans.
1. Preparation Phase
Your team will optimize your health. This might include nutritional shakes or specific exercises. You may also meet an enterostomal therapy (ET) nurse. They mark the potential stoma site just in case.
2. The Operation
The surgeon performs the colectomy. If they find the tissue is too inflamed, they will create the ileostomy. This is a real-time decision made for your safety. They prioritize your long-term health over immediate convenience.
3. Early Recovery
In the hospital, you will start walking early. If you have an ileostomy, you will learn to empty the bag. If you have no ileostomy, the staff will monitor your first bowel movement closely. For complex cases, air ambulance services are available for international transfers.
🏥 Case Study: Sarah’s Journey
Sarah, a 34-year-old teacher, suffered from severe Ulcerative Colitis. She was terrified of having a stoma. She researched ileostomy or no ileostomy options extensively. During her proctectomy, her surgeon noticed significant rectal inflammation.
To ensure Sarah’s safety, the surgeon chose a temporary ileostomy. Initially, Sarah was devastated. However, three months later, her body had healed perfectly. She underwent a successful reversal. Today, Sarah lives without a bag and has regained her quality of life. Her story highlights that an ileostomy is often just a temporary detour on the road to health.
💰 Global Cost Analysis Table
Medical tourism offers affordable paths for colectomy. Below is an estimated cost comparison for the procedure including ileostomy or no ileostomy management.
| Country | Estimated Cost (USD) | Included Services |
|---|---|---|
| USA / UK | $35,000 – $60,000 | Hospital stay only |
| Iran | $4,000 – $7,000 | Surgery, VIP Transfer, Hotel |
| Turkey | $8,000 – $12,000 | Surgery, Accommodation |
| India | $5,000 – $9,000 | Surgery, Nursing care |
🌍 Recovery & Medical Tourism with WMTour
Choosing to travel for surgery can reduce stress. At WMTour Iran, we provide end-to-end support. From your first telemedicine consultation to post-op care, we are here. Our vetted doctors specialize in minimally invasive techniques. This often increases the chances of a “no ileostomy” outcome.
Patients often combine their recovery with a peaceful stay in Mashhad. You can explore Mashhad locations while you heal. We handle the logistics, so you focus on health. Our team ensures that your journey is as smooth as possible.
⚠️ Medical Disclaimer
This content is for informational purposes only. It does not constitute professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice because of something you have read on this website. For more details, visit our official FAQ or contact us directly.
❓ Frequently Asked Questions (FAQ)
1. Can I live a normal life with an ileostomy?
Yes, you absolutely can live a full, active life with an ileostomy. Many people return to sports, swimming, and travel without any restrictions. Modern ostomy appliances are discreet and odor-proof. In fact, many professional athletes and models live with stomas successfully. The key is proper education and finding the right supplies for your body. Once you master the routine, it becomes a small part of your daily hygiene, much like brushing your teeth. Many find that the ileostomy actually gives them their life back by removing the pain of chronic illness.
2. How long does a temporary ileostomy usually last?
A temporary ileostomy typically remains in place for 3 to 6 months. This duration allows the internal connection (anastomosis) to heal completely without being stressed by waste flow. Your surgeon will perform tests, such as a contrast enema, to ensure there are no leaks before planning the reversal. If you are undergoing chemotherapy, the reversal might be delayed until your treatment is finished. The timing is always personalized to your recovery speed and nutritional status. Most patients find that the wait is worth the long-term safety it provides for their bowel health.
3. Is the choice between ileostomy or no ileostomy always up to me?
While your preferences are vital, the final decision is often made during surgery. The surgeon must evaluate the health of the tissue and the blood supply. If the conditions are unsafe, they will choose an ileostomy to prevent life-threatening complications. This is why it is important to discuss all possibilities during your consultation. Trusting your surgeon’s clinical judgment is crucial for a successful outcome. They want the same thing you do: a safe surgery and a healthy recovery.
4. What are the symptoms of an anastomotic leak if I have no ileostomy?
An anastomotic leak is a serious complication where the internal connection fails. Symptoms include severe abdominal pain, high fever, and a rapid heart rate. You might also notice a sudden drop in blood pressure or signs of sepsis. If you experience these after surgery, you must seek emergency medical attention immediately. Surgeons monitor patients very closely in the first week for these specific signs. Early detection often allows for quick intervention, which might include placing a temporary ileostomy to allow the area to heal. Understanding these risks is a key part of choosing ileostomy or no ileostomy.
5. Does a “no ileostomy” result mean I will go to the bathroom more often?
Yes, especially in the first few months after a colectomy. Because the colon’s job is to absorb water and store waste, its removal changes your habits. You may experience increased frequency and urgency, sometimes called “clustering.” Over time, the small intestine adapts and begins to take over some of these functions. Pelvic floor physical therapy can also help manage these changes effectively. Many patients find that their habits stabilize significantly after the first year. Comparing ileostomy or no ileostomy outcomes involves weighing this frequency against the management of a stoma bag.
6. Can I still eat my favorite foods with an ileostomy?
Most people with an ileostomy can eventually return to a normal diet. In the beginning, you will need to follow a low-fiber diet to prevent blockages. Gradually, you will reintroduce different foods one at a time to see how your body reacts. Staying hydrated is the most important factor, as the colon is no longer there to absorb water. Certain foods like corn, nuts, and popcorn require extra caution and thorough chewing. Most patients find they can enjoy almost everything they loved before surgery. It is all about balance and listening to your body’s new signals.
7. How painful is the ileostomy reversal surgery?
Ileostomy reversal is generally much less invasive than the original colectomy. It is often a shorter procedure with a faster recovery time. Most patients stay in the hospital for 2 to 4 days afterward. The main challenge is waking up the bowel, which may have been “sleeping” for several months. You might experience some temporary diarrhea or urgency as your system adjusts. However, the surgical pain itself is usually well-managed with standard medications. Most people are back to their normal activities within a few weeks of the reversal procedure.
8. What should I pack for my medical tourism trip for this surgery?
When traveling with WMTour, pack comfortable, loose-fitting clothing that won’t irritate an abdominal incision. Include a robe, slip-on shoes, and all your current medications in their original packaging. If you are expecting an ileostomy, you don’t need to bring supplies, as the hospital provides them initially. However, bringing a small pillow for the car or plane ride home can help support your abdomen. Don’t forget your medical records and any diagnostic scans. Our support team will provide a detailed checklist specific to your destination, whether it is Iran, India, or Oman.
9. Are there long-term complications to living with no ileostomy?
While “no ileostomy” is the goal for many, it can lead to Lower Anterior Resection Syndrome (LARS). This condition involves unpredictable bowel movements and occasional incontinence. It is most common when the surgery is very low in the rectum. Fortunately, there are many treatments available, including dietary changes and medications. Some patients also use transanal irrigation to manage their symptoms. Discussing these long-term functional outcomes with your surgeon is vital. It helps you set realistic expectations for life after a colectomy. Knowledge is the best tool for long-term success.
10. How do I choose the best surgeon for a “no ileostomy” outcome?
Look for a board-certified colorectal surgeon with extensive experience in restorative procedures. Ask about their “anastomotic leak rate” and how often they perform reversals. Surgeons who use robotic or laparoscopic techniques often have better visualization of the delicate tissues. At WMTour, we vet our doctors based on these specific quality metrics. A good surgeon will be transparent about the risks and won’t promise a “no ileostomy” result if it isn’t safe. Their primary focus should always be your long-term health and safety.
11. Does having an ileostomy affect my ability to get pregnant?
Generally, having an ileostomy does not prevent a healthy pregnancy. Many women have successful pregnancies and healthy babies after a colectomy. However, scar tissue (adhesions) from any abdominal surgery can sometimes impact fertility. It is important to discuss your family planning goals with your surgical team. They can often use techniques that minimize adhesion formation. If you do become pregnant, your stoma might change shape as your belly grows. An ostomy nurse can help you adjust your appliance during this time. Most importantly, focus on your health first, as a healthy body is the best foundation for a future pregnancy.
12. Can I exercise and go to the gym with an ileostomy?
Yes, exercise is highly encouraged once you have fully recovered from surgery. You should start slowly with walking and gradually increase your intensity. It is important to wear a support belt to prevent parastomal hernias, which are common after abdominal surgery. Many people with stomas participate in weightlifting, running, and even contact sports. There are specific ostomy accessories designed to keep the pouch secure during vigorous activity. Staying active helps your digestion and improves your mental well-being. Always consult with your doctor before starting a new, intense exercise routine to ensure your body is ready.
For more information on digestive health or to book a consult, visit our Departments Page. We provide world-class care in gastrointestinal oncology and more.
External Authority References:
Harvard Health Publishing |
Johns Hopkins Medicine |
Mayo Clinic