What Are Intersex Variations & When Is Surgery Considered? — Essential Context for Every Visitor
Executive Summary: Key Takeaways
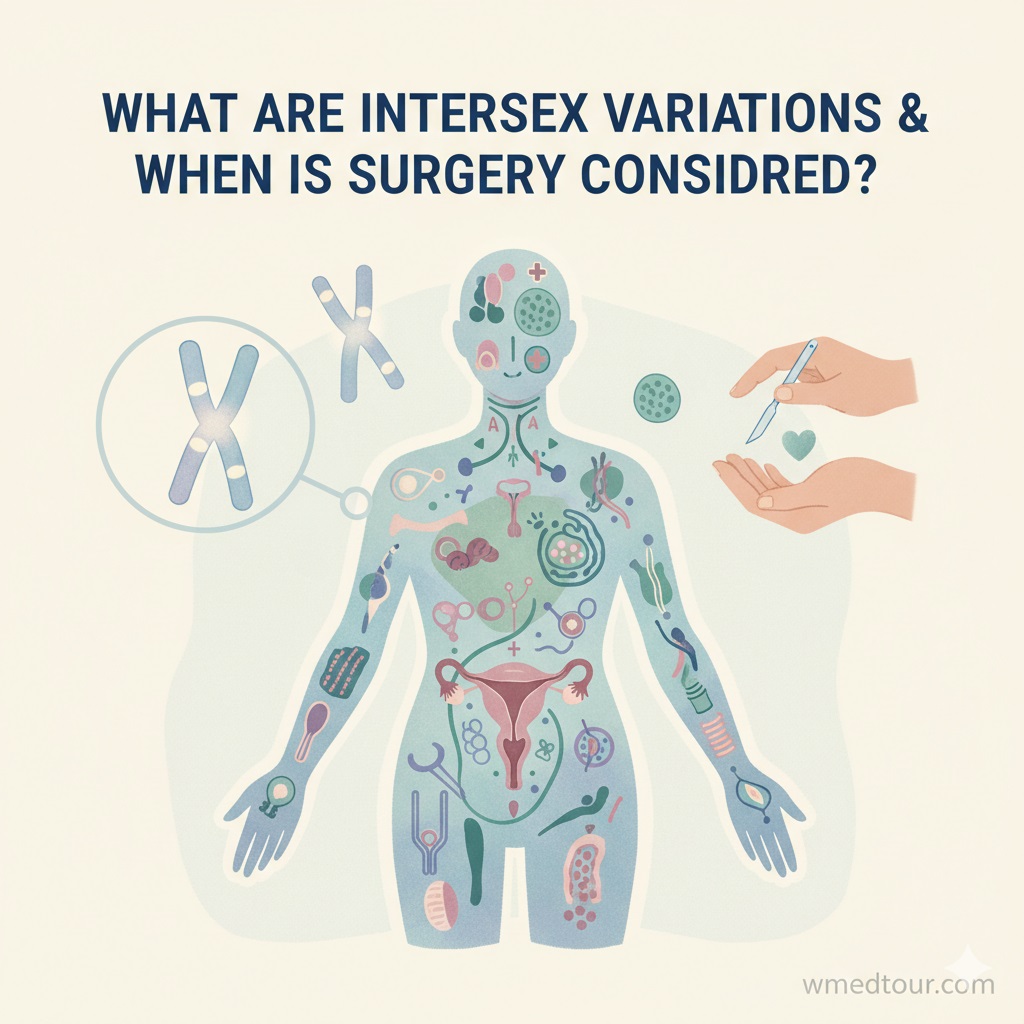
Intersex variations, which doctors often term Differences of Sex Development (DSD), refer to innate variations in a person’s sex characteristics, including chromosomes, hormones, or anatomy. In short, being intersex is simply a natural part of human biological diversity, affecting up to 1.7% of the global population. This foundational guide, therefore, provides critical ethical context for care.
- To begin with: Intersex is an umbrella term for dozens of different biological conditions, notably not a single one.
- Furthermore, treatment for an intersex variation falls into two categories: necessary (that is, to ensure organ function or prevent life-threatening conditions) and elective (in other words, for cosmetic or social reasons).
- Crucially, current global medical consensus strongly advocates for delaying all non-medically necessary surgeries on infants and children until the individual is mature enough to provide full, informed consent.
- Consequently, best practice involves a multidisciplinary team focusing on open disclosure, psychological support, and above all, respecting the individual’s bodily autonomy above social norms.
Defining Intersex Variations: A Spectrum of Biological Sex
We often think of human sex as strictly binary: male or female. However, biology is much more diverse than this simple dichotomy suggests. Indeed, Intersex variations exist when a person is born with anatomy, chromosomes, or hormone patterns that do not fit neatly into typical definitions of male or female. Simply put, it’s a natural phenomenon, not a disorder, thereby emphasizing that biological sex is a spectrum.
To help you visualize this, the percentage of people with an intersex trait is comparable to the number of people born with red hair. Therefore, approaching this topic with empathy and authority is absolutely essential. Although the medical field often uses the term Differences of Sex Development (DSD), for clarity, we use intersex variation here to emphasize biological diversity and align with community preference.
Furthermore, understanding these biological differences can shed light on complex areas, such as the legal and medical paths discussed in our guide to Gender Confirmation Surgery Legal Countries and Transgender Surgery Legal Countries Guide 2025. We encourage you to explore our Departments and the work of specialized Doctors, too.
Key Types of Intersex Variations (DSD)
In the first place, Intersexuality encompasses a broad array of conditions. Transitioning from the general definition, let’s explore three foundational types. Ultimately, understanding these categories is the first step in understanding why surgical timing is so critical.
1. Conditions Affecting Chromosomes (Sex Chromosome DSD)
For example, these variations involve atypical combinations of X and Y chromosomes. Klinefelter Syndrome (XXY) is a common example where a male is born with an extra X chromosome. Similarly, Turner Syndrome (XO) affects females with only one X chromosome. Consequently, these are systemic genetic variations that typically require hormone management but rarely immediate surgical intervention (Source: MedlinePlus).
2. Conditions Affecting Hormone Production (46, XX DSD)
The most common condition in this category is Congenital Adrenal Hyperplasia (CAH), whereby an individual with XX chromosomes may have masculinized genitalia due to the overproduction of androgens. Most importantly, CAH often requires immediate hormone treatment to prevent life-threatening salt-wasting crises, thus proving that hormone management can be a matter of medical urgency.
3. Conditions Affecting Hormone Response (46, XY DSD)
Androgen Insensitivity Syndrome (AIS) is a prime example. In this condition, individuals with XY chromosomes are unable to fully respond to male hormones, with the result that they exhibit female external characteristics. People with this intersex variation are often raised female, nonetheless, surgical considerations (like gonad removal for cancer risk) remain highly contentious, and hence, often delayed for patient consent.
We believe in providing transparent information. For instance, for context on other types of complex medical journeys, please review our comprehensive guides on Cardiovascular Surgery and Oncology treatments.
When Is Surgery Truly Considered for Intersex Variations?
The question of surgery is fraught with both medical necessity and profound ethical dilemmas. Therefore, we must rigorously differentiate between life-saving procedures and those performed for cosmetic or psychosocial ‘normalization.’
Category A: Medically Necessary or Urgent Surgery
In certain situations, which are thankfully rare, a surgical procedure is truly urgent. For instance, sometimes an anatomical structure prevents the outflow of urine or blood, thereby posing an immediate risk to organ function or life. Furthermore, some specific gonadal tissues carry a high, demonstrable risk of malignancy (cancer). In these cases, gonadectomy (surgical removal of the gonads) might be considered a necessary preventative measure, although even this decision requires careful, case-specific risk assessment and, ideally, patient consultation whenever possible. Major children’s hospitals stress the need for a highly specialized DSD team to make this delicate determination (Source: Children’s Hospital of Philadelphia).
Category B: Elective, Non-Medically Necessary Surgery
Historically, the majority of surgeries performed on intersex infants were elective. In essence, these procedures aimed to:
- Cosmetic Normalization: Altering the appearance of the external genitalia to make them look unequivocally male or female.
- Surgical Assignment: Creating internal tracts or structures to match the assigned gender.
However, many adults who underwent these procedures as children have reported significant physical and psychological harm, including loss of sexual sensation, scarring, and profound distress when their innate gender identity later conflicted with their surgically altered body. Consequently, this historical practice is now widely condemned by human rights bodies and indeed, increasingly rejected by leading medical associations. Thus, the ethical focus has fundamentally changed.
The Ethical Shift: Prioritizing Informed Consent
The global consensus on care for an intersex variation has undergone a paradigm shift, moving away from a model focused on cosmetic adjustment and towards one rooted in patient autonomy. Leading institutions now adhere to the principle that electively irreversible procedures should be deferred until the patient can give full, informed consent. This means, in particular, waiting until the individual reaches adolescence or adulthood.
Pros and Cons: Early Intervention vs. Deferred Consent
| Surgical Approach | Pros (Historical Argument) | Cons (Modern Criticism) |
|---|---|---|
| Early Surgery (Infancy/Childhood) | Reduces parental distress; moreover, facilitates easier birth registration and societal integration into a binary gender system. | Irreversible loss of sexual function/sensation; violation of bodily autonomy; plus, potential mismatch with later adult gender identity. |
| Deferred Surgery (Adolescence/Adulthood) | Preserves all sexual potential; above all, honors the individual’s right to self-determination; and thus, ensures full, informed consent. | May lead to periods of parental or childhood anxiety regarding physical difference; consequently, requires significant psychosocial support. |
A 2020 consensus statement by the European Society for Pediatric Endocrinology and Lawson Wilkins Pediatric Endocrine Society (Source: The Lancet) strongly affirms that procedures that are not essential for life or function should be postponed until the individual can participate meaningfully in the decision-making process. Indeed, the right to bodily integrity is paramount, much like complex decisions in neurosurgery or general surgery.
Case Journey: The Power of Deferred Consent
Imagine the case of Alex, born with an intersex variation presenting with ambiguous genitalia, and assigned female at birth based on the higher likelihood of fertility preservation and anticipated gender alignment. Unlike historical models, Alex’s parents followed the modern DSD protocol:
- Infancy: No cosmetic surgery was performed. Instead, the medical team focused on ensuring Alex’s urinary tract was functional—the only necessary intervention.
- Childhood: Alex was raised openly in the assigned gender. Importantly, her parents received counseling on open communication, avoiding secrecy about her difference. The focus was on psychological health.
- Adolescence: Alex received comprehensive education on her specific intersex variation, her anatomy, her hormonal profile, and the surgical options. Then, through psychological support, she affirmed her female identity.
- Adulthood (Age 22): Alex decided to undergo a minimal surgical procedure to further align her external body with her affirmed identity, but only after carefully weighing the risks to sexual sensation. Because the surgery was performed with her full, informed consent, the psychological outcome was overwhelmingly positive.
This hypothetical yet realistic journey demonstrates the long-term success of the “wait-and-see” approach, clearly prioritizing autonomy over expediency.
Who is This For?
This authoritative foundational explainer provides essential context for everyone involved in the DSD/Intersex community:
- New Parents: To begin with, to offer hope and the most current, ethical treatment protocols, thereby moving beyond outdated, damaging surgical practices.
- Medical Practitioners: Specifically, to ensure all professionals, from those in Urological Surgery to the Gynecological Surgery Department, adhere to the modern standards of informed consent.
- Advocates & Policy Makers: And finally, to provide clear, evidence-based data supporting the need to protect the bodily integrity of intersex children.
The principles of ethical decision-making discussed here also guide highly sensitive areas, such as the debate around Fetal Gender Selection Ethics and the pre-procedure checks required for complex reproductive treatments like ICSI Treatment and PGT-A/IVF. Moreover, our information about Global Medical Treatment Regulations and our Contact Us page are always available for further inquiries.
The Future of Care: Multidisciplinary and Patient-Driven
The gold standard for care involves a Multidisciplinary Team (MDT). Primarily, this team ensures that all aspects of an intersex variation—hormonal, genetic, social, and psychological—are addressed holistically. The team’s primary responsibility is providing the family with accurate information, psychosocial support, and the space to make decisions without the pressure of irreversible, non-urgent surgery. Consequently, the success of this model is being validated across the globe. The NIH recognizes the immense psychological component of this care, thus emphasizing the role of mental health professionals (Source: NIH).
FAQ: Important Answers About Intersex Variations
- Is an intersex variation a rare condition?
No, actually. Using a broad definition of biological variation, up to 1 in 60 people have an intersex trait. While specific, rare DSDs are less common, intersexuality is a recognized form of human biological diversity.
- Is intersex the same as having a disorder?
Medically, the term ‘Differences of Sex Development’ (DSD) is sometimes used, which implies a clinical difference. However, many intersex advocates argue that it’s a difference, not a deficit, and should not be pathologized unless it poses a direct health risk.
- What is the role of psychological counseling for parents?
Counseling helps parents process the diagnosis, manage anxiety, communicate openly and age-appropriately with their child about their body, and critically, resist societal pressures for immediate cosmetic surgery.
- Can the gender assignment change later in life?
Yes. Because gender identity develops over time, a person with an intersex variation may discover their internal sense of gender does not align with the gender assigned at birth. This is why deferring irreversible surgery is so vital.
- Are there long-term health risks if elective surgery is delayed?
Delaying elective (non-urgent) surgery carries no physical health risk. In fact, it preserves delicate sexual tissue and functionality, thereby preventing potential damage associated with premature procedures.
- How do DSD teams preserve fertility options?
By deferring gonadal surgery (unless the cancer risk is extremely high and proven), the MDT team preserves all potential fertility tissue until the patient is old enough to discuss options like sperm or egg retrieval, or tissue banking.
- Is secrecy or “hiding” the condition ever recommended?
Absolutely not. Modern care protocol strongly advises against secrecy. Open, age-appropriate disclosure of the intersex variation is linked to better psychological outcomes, greater self-acceptance, and stronger family trust.
- What is the difference between Intersex and Non-binary?
Intersex refers to biological sex traits. Non-binary refers to a gender identity that is not exclusively male or female. An intersex person can identify as non-binary, or they can identify as male or female.
- Do all intersex people require hormone therapy?
No. Only individuals with specific conditions, such as CAH (for life-saving management) or those needing pubertal induction, require hormone therapy. However, many people with an intersex variation have normal, balanced hormonal systems.
- Can an intersex person be fully heterosexual or homosexual?
Yes. Sexual orientation (who a person is attracted to) is independent of both biological sex and gender identity. In other words, Intersex people have all the same orientations as non-intersex people.
- What if a procedure is minimally invasive—can it still be done on a child without consent?
If a procedure is truly cosmetic or elective, even if “minimally invasive,” ethical standards still demand that it is postponed until the patient can consent, since it sets a precedent for surgical intervention.
- Where can I find support groups for intersex individuals and families?
The best starting point is often a university-affiliated DSD clinic, which typically maintains a directory of certified peer support organizations. Organizations like the Stanford Children’s DSD program actively work with support networks (Source: Stanford Children’s Health).
Further resources on specialized medical tourism, including Pre-Travel Resources and Checklists, and information on the Best Plastic Surgeons in Dubai or even complex cancer procedures in our Lung and Thoracic Surgery Department, all stress the fundamental importance of ethical and informed consent.
Final Considerations: Advocacy and Autonomy
Understanding what are intersex variations & when is surgery considered is crucial to modern, ethical medicine. Furthermore, it requires us to listen to the lived experiences of intersex adults who faced non-consensual surgeries. By delaying irreversible, non-urgent procedures, we honor the fundamental right to bodily integrity, thereby ensuring that individuals, rather than doctors or parents, ultimately control their own bodies.
For instance, for individuals researching other complex procedures requiring profound personal consent, consider guides on Fetal Gender Selection, Fetal Sex Determination, Gender Selection Methods 2025, and Fetal Gender Selection Best Countries 2025. Also, check our information on Orthopedic Treatment in Dubai and the work of our specialized Ophthalmology Department. Our dedication to ethical standards remains consistent across all medical specialties, including Checkup Departments and Dental procedures.