🌍 IVF & ICSI Treatment — Step-by-Step Guide for International Patients ✈️
Your Definitive Medical Tourism Handbook for In Vitro Fertilization and Intracytoplasmic Sperm Injection.
✨ Executive Summary: Key Takeaways
The journey to parenthood through **IVF & ICSI Treatment** abroad is a profound decision, driven by the search for lower costs, reduced wait times, and advanced care. Consequently, this comprehensive guide simplifies the process into clear, manageable steps.
- **IVF & ICSI Treatment** represents a global standard; however, clinics specifically indicate ICSI for male-factor infertility.
- International patients typically need to plan for a **3-4 week stay** for a fresh transfer cycle.
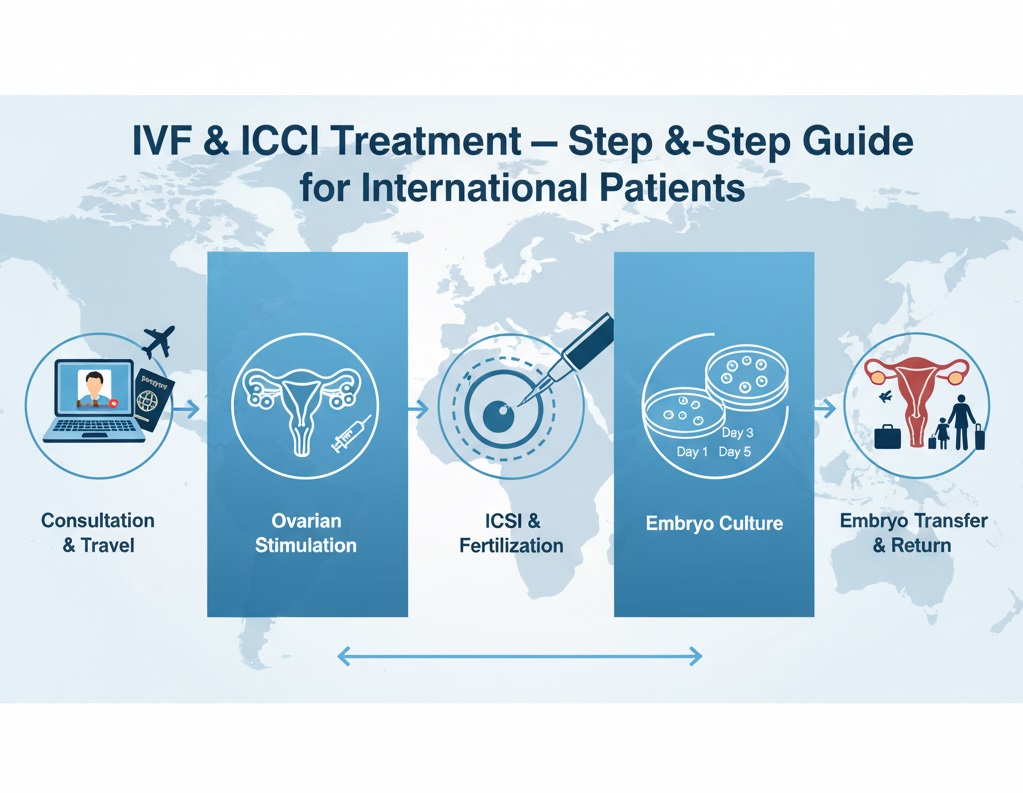
- The entire treatment breaks down into **5 core stages**: Pre-Cycle Preparation, Ovarian Stimulation, Egg Retrieval, Fertilization/Embryo Culture, and Embryo Transfer.
- Choosing a clinic demands meticulous research into **success rates, technology (e.g., PGT-A), and accreditation** in popular destinations like Turkey or Iran.
- Importantly, high-quality care is often accessible at a **fraction of the cost** compared to Western countries.
🔬 Understanding IVF and ICSI: The Foundations of Modern Fertility
Infertility affects millions of couples worldwide, therefore prompting many to explore the advanced options offered by medical tourism. Among these treatments, **IVF & ICSI Treatment** represents the pinnacle of assisted reproductive technology (ART). Understanding the core difference is essential for any international patient planning their journey.
What is In Vitro Fertilization (IVF)?
In Vitro Fertilization, literally meaning “fertilization in glass,” involves combining an egg with sperm outside the body in a laboratory dish. Following successful fertilization, the embryologist cultures the resulting embryo for several days before the doctor transfers it to the woman’s uterus. IVF remains the standard treatment for various causes of infertility, including tubal issues, endometriosis, or unexplained infertility.
→ Explore IVF treatment options
What is Intracytoplasmic Sperm Injection (ICSI)?
ICSI represents a specialized form of IVF. Instead of simply placing the sperm and egg together, a highly skilled embryologist uses a tiny needle (micropipette) to inject a single, carefully selected sperm directly into the center of the egg. This technique dramatically increases the chance of fertilization, especially in cases of severe male-factor infertility, where sperm count or motility is very low, or when the clinic uses surgically retrieved sperm. Consequently, for many international couples, clinics often perform **IVF & ICSI Treatment** together.
Pros and Cons of ICSI
✅ ICSI Pros
- Achieves a significantly **Higher Fertilization Rate** in cases of male infertility.
- Is essential for **surgically extracted sperm** (e.g., TESA, TESE).
- Reduces the chance of **failed or low fertilization** in couples with previous IVF failures.
- PGT preparation: Ensures only one sperm fertilizes the egg, preventing potential genetic contamination.
❌ ICSI Cons
- Requires **more advanced equipment and expertise** than standard IVF.
- Incurs a slightly **higher cost** per cycle due to the complex procedure.
- The sperm selection process bypasses **natural selection**, although current research shows no significant increase in birth defects.
- It carries a risk of **egg damage** during the injection process, though this happens rarely.
🗺️ The International Patient Journey: A 5-Step IVF & ICSI Treatment Guide
For patients traveling overseas, planning becomes paramount. The typical **IVF & ICSI Treatment** cycle needs synchronization to maximize egg production, thus requiring careful coordination with the clinic abroad. We break down the process into five clear stages for international patients. Therefore, to ensure full preparation, we recommend reviewing our Fertility Treatments Pre-Travel Checklist.
Step 1: The Pre-Cycle Preparation and Initial Consultation 📞
This phase primarily utilizes remote communication, minimizing your required time abroad. It’s where the clinic lays the groundwork for your successful **IVF & ICSI Treatment**.
- **Remote Consultation & Planning:** The international patient sends all existing medical records (ultrasounds, blood tests, semen analysis) to the chosen clinic. The fertility specialist reviews the case and designs a personalized treatment protocol. Learn more about how to manage the online consultation guide for IVF abroad.
- **Diagnostic Testing:** Required tests include ovarian reserve markers (AMH, FSH, AFC), infectious disease screening, and a comprehensive semen analysis. In addition, in some cases, further fertility check-ups may become necessary.
- **Travel and Visa Logistics:** Secure your travel arrangements and necessary medical visas. You will likely need to plan for a stay of 20-30 days for a fresh cycle. Consider resources like the Medical Visa Definitive Patient Handbook.
Step 2: Ovarian Stimulation (Approx. 10-14 Days) 💉
Ovarian stimulation proves crucial for a successful IVF/ICSI cycle. Its goal is to encourage the ovaries to produce multiple mature eggs, as opposed to the single egg typically produced in a natural cycle.
- **Medication Protocol:** Starting on Day 2 or 3 of your menstrual cycle, you’ll begin daily injections of Follicle-Stimulating Hormone (FSH) and/or Luteinizing Hormone (LH).
- **Monitoring:** This phase demands frequent monitoring via blood tests (measuring estrogen and progesterone levels) and transvaginal ultrasounds (to measure follicular growth). Consequently, international patients often start this phase locally and travel right before the next stage, or complete the entire phase at the clinic abroad.
- **Trigger Shot:** Once the majority of follicles reach the optimal size (17-20mm), the clinic administers a final injection (the “trigger shot,” usually hCG) precisely 34-36 hours before the egg retrieval.
Step 3: Egg Retrieval and Sperm Collection 🥚
This procedure marks the first one performed once you arrive at the international clinic for your **IVF & ICSI Treatment**.
- **Egg Retrieval:** Performed under light sedation, the physician uses an ultrasound-guided needle to gently extract follicular fluid containing the eggs. The procedure is brief, typically taking 20-30 minutes.
- **Sperm Collection:** The male partner provides a semen sample on the same day. For cases requiring ICSI, the embryologist isolates the best, healthiest sperm. If TESE or TESA is required, they also perform the retrieval procedure at this time.
Step 4: Fertilization and Embryo Culture 🧬
In the laboratory, decisions determine the fate of the eggs and sperm, marking the successful fusion of **IVF & ICSI Treatment**.
- **Fertilization:**
- **IVF:** Embryologists combine eggs and tens of thousands of sperm in a petri dish.
- **ICSI:** The embryologist microinjects a single sperm into each mature egg.
- **Embryo Culture:** The team monitors the fertilized eggs (zygotes) in a specialized incubator. They typically culture them for 3 to 5 days, allowing them to reach the cleavage (Day 3) or the blastocyst (Day 5) stage.
- **Genetic Testing (Optional):** If patients opt for Preimplantation Genetic Testing (PGT), the team performs a biopsy of the Day 5 blastocyst before freezing (cryopreserving) it for a future Frozen Embryo Transfer (FET) cycle.
Step 5: Embryo Transfer (Fresh or Frozen) 🤱
This stage represents the final, most critical step of the **IVF & ICSI Treatment** cycle.
- **Fresh Transfer:** The doctor transfers a high-quality embryo (usually 3 or 5 days old) to the uterus using a thin catheter, guiding the procedure with ultrasound. This is generally a painless procedure requiring no anesthesia.
- **Frozen Embryo Transfer (FET):** If PGT was performed, or if the clinic recommends a break before transfer, the patient will return for a separate, shorter cycle. This cycle focuses solely on preparing the uterine lining (endometrium) for the frozen embryo transfer.
- **Post-Transfer Care:** The international patient receives vital instructions for the “two-week wait.” This includes continuing prescribed hormonal support (progesterone, estrogen) until the pregnancy blood test.
→ For more detail, read the ultimate step-by-step guide to the IVF process
🧑⚕️ Who is This For? Ideal Candidates for International IVF & ICSI Treatment
Medical tourism for fertility is not a one-size-fits-all solution. Instead, it is especially suited for patients facing specific challenges:
The Primary Candidates:
- **Cost-Sensitive Couples:** Patients facing prohibitively high costs in their home country. Affordable, high-quality centers in destinations like Turkey or Iran can offer up to 70% savings. Discover the cheapest IVF trusted centers abroad 2025.
- **Couples with Severe Male Factor Infertility:** Cases requiring mandatory ICSI, TESE, or TESA often seek specialized laboratories with high ICSI success rates.
- **Patients Seeking Specific Technologies:** Those who require advanced options like Preimplantation Genetic Testing (PGT-A/PGT-M) or fertility preservation treatments.
- **Patients Facing Long Wait Times:** In countries with national healthcare systems, wait lists for treatment can span months or even years. Conversely, international travel offers immediate access to care.
- **Individuals Seeking Legal Access to Services:** Certain countries have more permissive laws regarding donor gametes (egg or sperm donation) or surrogacy, making them viable options for international patients. Refer to our guide on fertility treatments abroad, including egg donation.
📊 Success Rates and Cost Comparison of IVF & ICSI Treatment
Success rates are the most important metric, but one must interpret them carefully. Credible sources, such as the Centers for Disease Control and Prevention (CDC) in the US, generally show an inverse relationship between a woman’s age and the success of ART. Furthermore, the type of procedure—standard IVF or **IVF & ICSI Treatment**—can impact the initial fertilization rate.
Why are Success Rates Difficult to Compare?
Many clinics report their success rates as “Clinical Pregnancy Rate per Embryo Transfer,” which represents the highest possible number. A more honest and internationally comparable metric, however, is the **Live Birth Rate per Embryo Transfer**. Always ask for age-specific data, as the quality of the eggs remains the single biggest predictor of success. Importantly, therefore, a patient must conduct thorough research.
For example, live birth rates from non-donor eggs typically decrease from ~50% for women under 35 to less than 5% for women over 44, regardless of where the treatment is performed (Source: American Society for Reproductive Medicine). Consequently, managing expectations based on age-specific data proves vital.
IVF/ICSI Global Cost Comparison Table (2025 Estimates)
The dramatic price difference serves as the primary motivator for pursuing **IVF & ICSI Treatment** abroad. These are estimates for a single cycle, excluding medication, PGT, or travel costs.
| Country/Region | Estimated IVF/ICSI Base Cost (USD) | Average Wait Time |
|---|---|---|
| USA / Western Europe | $12,000 – $25,000+ | Immediate access (high cost) |
| Turkey (e.g., Istanbul) | $3,500 – $6,000 | Immediate access (low cost) |
| Iran (e.g., Tehran, Mashhad) | $2,500 – $4,500 | Immediate access (lowest cost) |
| India / Asia | $3,000 – $5,500 | Immediate access |
*Note: This data is an estimation. Medication costs can add $3,000 – $6,000 USD to the total. Explore cost comparisons for other medical procedures as well.
📖 Case Study: Maria and David’s International ICSI Journey
To fully illustrate the process, consider the hypothetical journey of Maria (38) and David (40) from Australia. They faced high costs and a diagnosis of low sperm motility (Oligoasthenozoospermia).
The Challenge and The Choice
In Australia, a single IVF cycle exceeded $15,000, not including specialized ICSI fees. After researching medical tourism options and reading our guide on Medical Travel Turkey 2025, they chose a highly-accredited clinic in Istanbul for their **IVF & ICSI Treatment** cycle. Consequently, the base cost was nearly 70% lower there.
Maria and David’s Timeline:
- **Month 1 (Australia):** They held an initial online consultation with the Turkish specialist. Maria completed preliminary blood work and a baseline ultrasound locally. The clinic finalized the treatment plan, which included mandatory ICSI due to David’s diagnosis.
- **Month 2 (Turkey – Weeks 1 & 2):** Maria and David travel to Istanbul. Maria starts the **Ovarian Stimulation** phase, with the clinic monitoring her closely. This intensive monitoring is why a minimum 14-day stay is required.
- **Month 2 (Turkey – Week 3):** Egg Retrieval and Sperm Collection (via standard ejaculate, with ICSI planned) occurred. The team retrieved eight eggs, and subsequently, they injected all of them with sperm (ICSI). Six successfully fertilized.
- **Month 2 (Turkey – Week 3, Day 5):** Two embryos reached the blastocyst stage. The doctor performed a **Fresh Embryo Transfer** of one high-quality blastocyst. The remaining embryo was frozen.
- **Month 2 (Turkey – Week 4):** They enjoyed a post-transfer rest period and cultural activities in Istanbul before returning home.
- **Post-Trip:** The pregnancy test performed two weeks later showed a positive result.
This journey highlights the efficiency of undergoing all critical stages of the **IVF & ICSI Treatment** in a concentrated time frame abroad, consequently offering both cost savings and timely access to specialized care.
⚖️ Navigating the Legal and Ethical Landscape Abroad
When seeking **IVF & ICSI Treatment** internationally, ethical and legal considerations become critically important. What is legal in one country may, conversely, be heavily regulated or illegal in another.
Key Ethical Differences for International Patients
- **Embryo Disposition and Donation:** Laws governing embryo storage duration and whether patients can donate them to other couples or science vary widely.
- **Surrogacy:** Many countries, including most of Europe and even Turkey, impose strict or outright bans on surrogacy. Conversely, countries like the US or Georgia maintain well-established, legal frameworks. For legal guidance, consult the European Society of Human Reproduction and Embryology.
- **Genetic Screening (PGT) and Gender Selection:** The use of PGT-A for non-medical purposes, specifically for gender selection or family balancing, serves as a major factor driving medical tourism. While it remains illegal or heavily restricted in many countries (e.g., Canada, UK), it is legal in popular medical tourism spots like the US, Thailand, and Iran. Always ensure your clinic provides comprehensive counseling and informed consent.
- **Gamete Donation (Egg/Sperm):** The availability of anonymous versus non-anonymous donors, and the strictness of screening, differs by jurisdiction.
Pre-Travel Due Diligence Checklist
Before committing to an international **IVF & ICSI Treatment** center, you must take the following steps:
- **Verify Accreditation:** Check that the clinic holds accreditation from reputable national bodies and, ideally, by international standards (e.g., ISO, JCI). We only partner with vetted institutions, such as those listed in our partner hospital directory.
- **Understand Local Law:** Confirm the legality of your required procedures (e.g., PGT, donor eggs) within the chosen country.
- **Get Written Contracts:** Ensure all costs, guarantees, and the plan for unused embryos are clearly documented.
💡 Advanced Techniques Combined with IVF & ICSI Treatment
The field of reproductive medicine is rapidly evolving, and thus international centers are often at the forefront of implementing new technologies to improve the success of **IVF & ICSI Treatment**.
Preimplantation Genetic Testing (PGT-A/M/SR)
PGT is the most significant advancement, enabling embryologists to screen embryos for chromosomal and genetic disorders *before* transfer. This involves biopsying the embryo (often a blastocyst), followed by genetic analysis. Importantly, New methods in IVF, such as AI-driven embryo selection and non-invasive PGT (niPGT), are further refining this process. This process is complex, but understanding PGT-A vs. MicroSort success rates proves crucial if gender selection is a goal.
Key PGT Options:
- **PGT-A (Aneuploidy):** Screens for the correct number of chromosomes (e.g., detects Down syndrome). This improves implantation rates and reduces miscarriage risk.
- **PGT-M (Monogenic/Single-Gene Disorder):** Screens for specific inherited conditions (e.g., Cystic Fibrosis).
- **PGT-SR (Structural Rearrangements):** Screens for chromosomal translocations or inversions.
Other Complementary ART Techniques
- **Assisted Hatching (AH):** Embryologists create a small opening in the embryo’s outer shell (zona pellucida) just before transfer to help it implant in the uterine lining.
- **Endometrial Receptivity Analysis (ERA):** A test to determine the optimal window for embryo transfer; this is particularly useful for patients with repeated implantation failure.
- **Sperm Selection Methods (e.g., Microfluidics, PICSI):** These advanced techniques help select the best sperm for ICSI, further improving the fertilization and embryo quality within the context of **IVF & ICSI Treatment**.
❓ Frequently Asked Questions (FAQ) for International Patients
Navigating international fertility treatment raises many practical and medical questions. Here are answers to the most common queries, compiled from international patient experiences.
Addressing Common Concerns About IVF & ICSI Logistics
What is the primary difference between IVF and ICSI?
The fundamental difference lies in how the sperm fertilizes the egg. In standard IVF, thousands of sperm are placed in a dish with the egg, allowing natural fertilization. Conversely, in ICSI (Intracytoplasmic Sperm Injection), a single, healthy sperm is manually injected directly into the center of the egg. Clinics typically use ICSI for cases of severe male factor infertility.
How long should international patients plan to stay for IVF & ICSI Treatment abroad?
Most standard IVF cycles require an international stay of approximately **three to four weeks**. This period successfully covers the ovarian stimulation phase, egg retrieval, fertilization, and fresh embryo transfer. However, if you opt for a frozen embryo transfer (FET), you may return for a much shorter trip later, or you may coordinate the stimulation and monitoring phases with a local doctor before traveling for the final procedures.
Is ICSI always necessary with IVF?
No, ICSI is not always necessary. Clinics typically recommend it when a significant male factor issue exists, such as low sperm count, poor motility, or poor morphology. Furthermore, doctors use it when surgically retrieved sperm is utilized, when standard IVF previously failed fertilization, or sometimes in cases involving preimplantation genetic testing (PGT) to reduce the risk of contamination. Explore ICSI options here.
What tests are required before starting the IVF cycle?
Before starting the cycle, both partners undergo comprehensive testing. For the female partner, this includes ovarian reserve tests (AMH, FSH, Estradiol, Antral Follicle Count), infectious disease screening (HIV, Hepatitis B/C), and sometimes a uterine evaluation (ultrasound, hysteroscopy). In addition, the male partner requires a complete semen analysis and infectious disease screening.
Does the success rate of IVF & ICSI Treatment vary by country?
Yes, success rates can vary significantly, not just by country, but by clinic, the patient’s age, and the specific cause of infertility. Consequently, when comparing international centers, it is vital to look for clinics that report live birth rates per embryo transfer and adhere to international reporting standards. Always look beyond high-level advertising figures and ask for age-specific data. Consult our guide on fertility problems and IVF abroad.
What is Preimplantation Genetic Testing (PGT) and why is it used?
PGT involves taking a few cells from the embryo (typically at the blastocyst stage) to screen for genetic or chromosomal abnormalities before transfer. PGT-A screens for aneuploidy (incorrect number of chromosomes), PGT-M screens for specific single-gene defects, and PGT-SR screens for structural rearrangements. This helps improve success rates, reduce miscarriage risk, and importantly, in some regions, clinics use it for fetal gender selection or family balancing.
What medications are involved in the ovarian stimulation phase?
The main medications are Gonadotropins (FSH and/or LH, such as Follistim or Gonal-F) to stimulate the ovaries to produce multiple follicles. Patients also use medications to prevent premature ovulation (like GnRH antagonists or agonists) and an HCG trigger shot to mature the eggs just before retrieval. They typically self-administer these injections.
How is egg retrieval performed?
The clinic performs egg retrieval as a minor surgical procedure under light sedation or general anesthesia. The doctor uses a transvaginal ultrasound probe to guide a fine needle through the vaginal wall into the ovaries to gently aspirate the fluid from each follicle, which contains the eggs. The procedure usually takes about 20-30 minutes. Therefore, patients should plan for a brief recovery period immediately afterward.
What happens after the embryo transfer?
After the embryo transfer, patients enter the “two-week wait” phase, where they continue to take progesterone and sometimes estrogen to support the uterine lining. Approximately 9-14 days after the transfer, the clinic performs a blood test (beta-hCG) to determine if a pregnancy has been achieved. The clinic will provide clear instructions on follow-up care and when to stop medications.
Are there any ethical concerns to consider when traveling abroad for fertility treatment?
Yes, ethical considerations are crucial. Regulations governing embryo donation, sperm/egg donation, surrogacy, and genetic testing (like PGT for non-medical reasons) vary widely by country. Consequently, international patients must be fully aware of the legal and ethical landscape of their chosen destination and ensure the clinic adheres to high standards. We encourage patients to review our guide on global medical treatment regulations.
What is the typical cost range for an IVF & ICSI Treatment cycle abroad?
The cost can vary dramatically. Generally, in popular medical tourism destinations, a single IVF/ICSI cycle can range from $3,000 to $8,000 USD, excluding medications, travel, and accommodation. Consequently, this is often significantly lower than costs in Western countries. Always ask for an all-inclusive package price to avoid hidden fees and refer to our complete guide to egg donation IVF costs.
What defines a ‘fresh’ vs. a ‘frozen’ embryo transfer?
A ‘fresh’ embryo transfer occurs when the doctor transfers an embryo into the patient’s uterus 3 or 5 days immediately following egg retrieval and fertilization, all within the same cycle. Conversely, a ‘frozen’ embryo transfer (FET) involves thawing an embryo that was cryopreserved (frozen) in a previous cycle. Importantly, FETs are often preferred in PGT cycles or when the patient needs time for ovarian hyperstimulation symptoms to resolve.
We are dedicated to supporting you through every phase of your **IVF & ICSI Treatment** journey, ensuring clarity and transparency from the initial consultation to your return home. For more information, please visit our FAQ page.