⭐ IVF or ICSI? Complete Differences + Cost + Success Rates in 2026 🔬
Navigating your crucial fertility choice with clarity and confidence.
Published by WMedTour | Fertility Articles
📝 Executive Summary: Key Takeaways
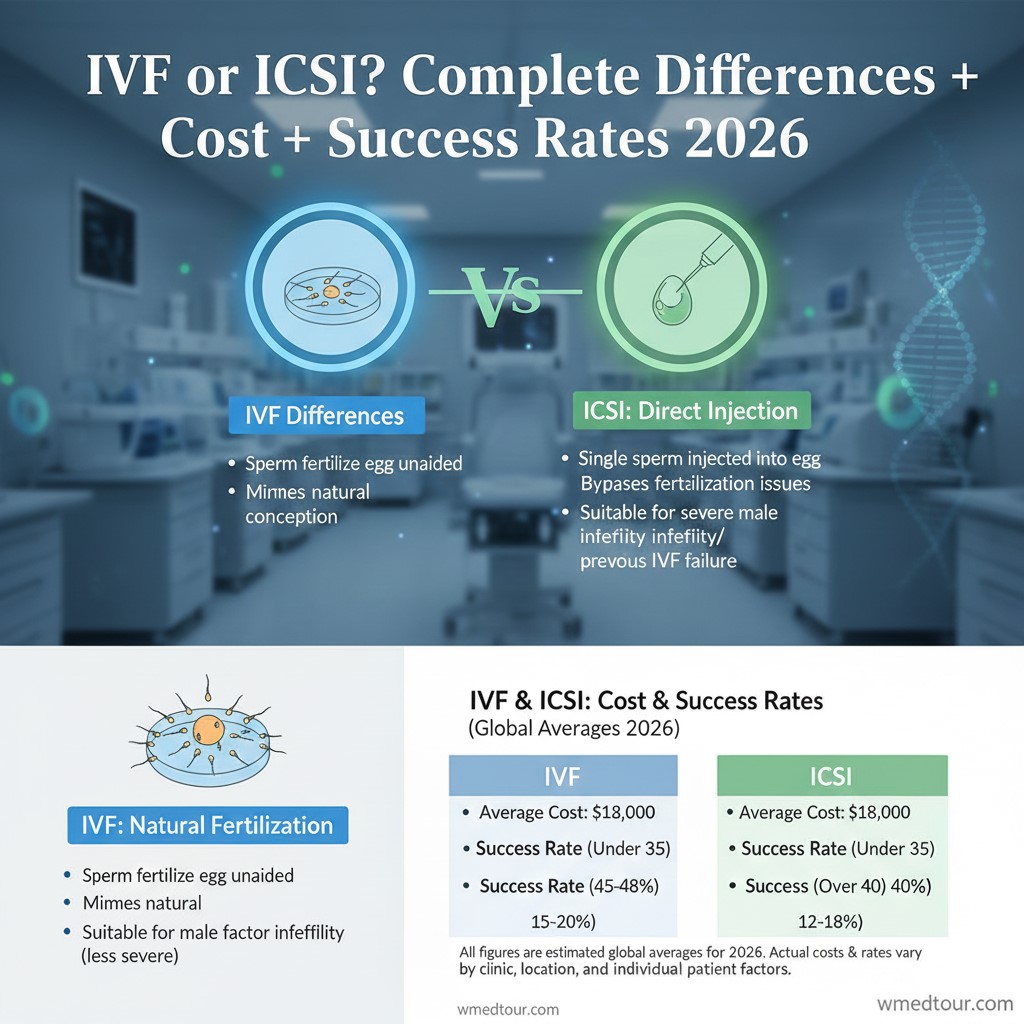
- Mechanism: Standard IVF relies on natural sperm selection; ICSI physically injects one sperm into the egg, bypassing barriers.
- Indication: Doctors primarily use ICSI for severe male factor infertility (low count/motility) or if previous IVF failed to fertilize. Conversely, they recommend standard IVF for tubal factors or ovulation issues.
- Cost: ICSI invariably costs more than standard IVF because it requires specialized equipment and significant embryologist time. Globally, these costs vary substantially.
- Success Rates: When indicated, ICSI achieves significantly higher fertilization rates. However, the final clinical success rates (live birth) for IVF and ICSI are often comparable once fertilization occurs.
1. Understanding the Core Difference: IVF vs. ICSI
Couples facing infertility receive treatment options, often focusing on In Vitro Fertilization (IVF). However, a significant subset of patients requires a variation called Intracytoplasmic Sperm Injection (ICSI). Therefore, understanding the distinction between these two procedures remains critically important for making informed choices regarding your fertility path.
🥚 Standard In Vitro Fertilization (IVF)
Standard IVF constitutes the foundational assisted reproductive technology (ART). Specialists retrieve the patient’s eggs and the partner’s (or donor’s) sperm. Consequently, they place high concentrations of sperm and a few eggs together in a laboratory dish. This process mimics natural conception: the strongest sperm must penetrate the outer layer of the egg independently to initiate fertilization. Therefore, doctors typically use standard IVF when infertility stems from tubal blockage, endometriosis, or unexplained factors, where sperm function is normal. This approach offers a powerful solution for many, representing a standard therapeutic choice for fertility problems.
💉 Intracytoplasmic Sperm Injection (ICSI)
ICSI represents a targeted, advanced technique often performed alongside standard IVF procedures. With ICSI, the embryologist selects a single, healthy-looking sperm. Then, they use a microscopic needle to inject that sperm directly into the egg’s cytoplasm. This step entirely bypasses the need for the sperm to penetrate the egg’s outer layers on its own. Consequently, ICSI dramatically increases the chance of fertilization for couples dealing with severe male factor infertility or other specific challenges. Thus, the procedure often guarantees fertilization where standard methods might fail. For instance, ICSI treatment provides hope for men with extremely low sperm count or poor motility.
2. Complete Differences: Mechanism, Indications, and Use
While both procedures share the initial stages—ovarian stimulation and egg retrieval—they diverge fundamentally during the fertilization stage. Moreover, the reasons doctors recommend each procedure differ significantly, depending largely on the specific cause of infertility. We outline these crucial distinctions below.
⚙️ Mechanism of Action
The core difference centers on sperm selection. Standard IVF allows natural selection: thousands of sperm surround the egg, and one naturally enters. Conversely, ICSI involves mechanical intervention: a skilled embryologist manually selects and injects one sperm. Therefore, the ICSI process requires highly specialized micro-manipulation equipment and significant expertise. This manual step essentially guarantees the sperm and egg meet, overcoming biological barriers that prevent natural fusion. However, some debate exists whether this bypass of natural selection affects long-term outcomes. Furthermore, the ICSI procedure requires a higher initial investment in laboratory setup and staffing, reflecting its technical complexity.
📋 Primary Indications for Each Technique
Physicians use different diagnostic results to determine the most effective approach. Specialists typically recommend standard IVF when the female partner possesses tubal factors (e.g., blocked fallopian tubes) or ovulatory dysfunction, provided the male partner demonstrates normal semen parameters. Alternatively, doctors prescribe ICSI primarily for severe male factor infertility, including very low sperm counts (oligozoospermia) or poor sperm movement (asthenozoospermia). Moreover, ICSI is mandatory when retrieving sperm surgically from the testicles (e.g., TESA or PESA). Furthermore, ICSI becomes the preferred, if not required, method for advanced procedures like Preimplantation Genetic Testing (PGT), preventing contamination from stray sperm.
3. Cost Analysis: ICSI is More Expensive
Cost remains a major factor for prospective parents pursuing assisted reproduction. Generally speaking, ICSI adds a significant cost to the base IVF cycle price. We investigate the reasons for this cost difference.
💸 Why ICSI Increases Cost
The increased cost of ICSI stems directly from the need for advanced micro-manipulation technology and the specialized human labor involved. First, the laboratory requires specialized equipment, including a micromanipulator and high-power microscopes, representing a substantial capital investment. Second, a highly trained embryologist must perform the injection procedure manually, demanding considerable time and skill. This manual intervention distinguishes ICSI from the simpler, less hands-on process of standard IVF. Consequently, the fee for ICSI typically adds $1,000 to $2,500 to the total IVF cycle cost, depending on the clinic and country. Understanding the global cost of ICSI treatment helps patients budget effectively.
🌍 Global Price Comparison
Geographic location heavily influences the final price for any fertility treatment. For instance, IVF and ICSI procedures in North America or Western Europe carry substantially higher price tags than those offered in popular medical tourism destinations. Countries like Turkey or Iran offer excellent care at significantly reduced rates, attracting international patients. We advise prospective parents to check the inclusive costs carefully. Often, clinics quote the base IVF price separately from the ICSI add-on, along with costs for medication and egg donation fees if applicable. Therefore, obtain a comprehensive quote encompassing all expected services before committing. Furthermore, patients often find more affordable options through organized medical travel packages.
4. Success Rates: Fertilization vs. Live Birth
Patients often ask, “Does ICSI improve our chances?” The answer requires separating the fertilization rate from the ultimate clinical success rate—the live birth rate. This distinction provides vital perspective for anyone exploring IVF success rates by age.
📈 Fertilization Rate Metrics
ICSI is a technical success at the fertilization level. When severe male factor infertility is the issue, standard IVF may achieve a low fertilization rate (e.g., under 20%). Conversely, ICSI typically achieves fertilization in 70% to 85% of injected eggs, directly overcoming the sperm-related barrier. Thus, ICSI almost guarantees fertilization for couples who otherwise would have few, if any, embryos to transfer. This initial step remains critical for moving forward in the fertility process.
👶 Clinical Success (Live Birth Rate)
Significantly, the live birth rate for ICSI does not automatically surpass that of standard IVF. Once fertilization successfully occurs, the resulting embryo’s quality—and the subsequent chances of successful implantation—depend primarily on the age of the female partner and the overall health of the gametes. Research consistently shows that for non-male factor infertility, using ICSI instead of standard IVF provides no additional benefit to the live birth rate. Therefore, specialists strictly reserve ICSI for cases where the specific clinical indication warrants its use. Consult high-ranking university sources, such as reports from the Centers for Disease Control and Prevention (CDC), for detailed, uncompetitive, and authoritative statistics on both procedures.
5. Detailed Comparison: Features and Suitability
The following table summarizes the key operational, financial, and clinical differences between the two fertilization methods. This side-by-side view helps solidify the decision-making process for patients and practitioners alike.
| Feature | Standard IVF | ICSI |
|---|---|---|
| Fertilization Method | Natural sperm penetration (mass action) | Single sperm injected manually into the egg |
| Primary Indication | Tubal factor, ovarian factors, unexplained infertility | Severe male factor infertility, previous low fertilization, PGT |
| Relative Cost | Base IVF cost (lower) | Base IVF cost + significant ICSI add-on (higher) |
| Risk of Fertilization Failure | Higher risk if male factor is present | Significantly lower (high success in achieving fertilization) |
| Need for Embryologist Skill | Standard technical skill | Highly specialized micro-manipulation skill |
6. The Advantages and Disadvantages of Each Path
✅ Standard IVF: Pros and Cons
Pros of Standard IVF
- Natural Selection: Allows the most capable sperm to fertilize the egg naturally.
- Lower Cost: Avoids the substantial added expense of the ICSI procedure.
- Established Safety: Represents the most time-tested and globally standardized ART technique.
Cons of Standard IVF
- Risk of Total Failure: Faces a higher risk of zero or low fertilization if undetected male factor issues exist.
- Limited Use: Unsuitable for couples requiring sperm retrieval via biopsy or those pursuing PGT screening.
❌ ICSI: Pros and Cons
Pros of ICSI
- Guaranteed Fertilization: Achieves high fertilization rates even with minimal, poor-quality, or surgically retrieved sperm.
- Essential for PGT: Prevents cross-contamination by extraneous sperm when performing genetic testing.
- Overcomes Failure: Offers the only path forward for couples with a history of complete fertilization failure in previous IVF cycles.
Cons of ICSI
- Increased Cost: Significantly raises the total treatment expense due to technology and labor. For example, check the cost of the cheapest IVF centers abroad.
- Bypassed Selection: Bypasses the natural selection process, potentially introducing slightly elevated risks depending on the specific cause of male infertility (consult a genetics specialist).
7. Who is This For? Making the Right Choice
Determining whether to proceed with IVF or ICSI depends entirely on clinical diagnosis. Patients should avoid choosing based solely on success rates or cost; instead, they must follow the specific medical indications.
👩🦱 Ideal Candidates for Standard IVF
Standard IVF remains the gold standard for couples experiencing female-factor infertility. These factors include blocked or damaged fallopian tubes, ovulation disorders, and mild endometriosis. Furthermore, doctors often recommend standard IVF for couples with unexplained infertility who have normal semen analysis results. In these cases, the sperm possesses the functional capacity to fertilize an egg, and the standard approach offers the necessary assistance to bypass other physical barriers. Consequently, these patients enjoy the lower cost and more natural selection process of standard IVF.
👨🦰 Ideal Candidates for ICSI
ICSI is a necessity for several groups. Primarily, men with severe oligozoospermia (very low sperm count), asthenozoospermia (poor motility), or teratozoospermia (abnormal morphology) require ICSI. Secondly, physicians mandate ICSI when sperm comes directly from the testicles or epididymis using surgical extraction techniques. Thirdly, ICSI becomes necessary when previous standard IVF cycles resulted in total fertilization failure. Fourthly, laboratories often require ICSI when performing PGT-A or PGT-M to ensure accuracy. The use of ICSI for these indications provides the highest chance of achieving viable embryos.
8. Patient Journey Example: Choosing the Right Path
📖 Case Study: The Decision Between IVF or ICSI
Sarah (35) and Mark (37) sought fertility treatment after three years of trying. Doctors identified no major issues with Sarah’s ovarian reserve or fallopian tubes. However, Mark’s semen analysis revealed severe oligoasthenozoospermia—a very low sperm count combined with poor motility.
The fertility clinic immediately recognized the primary obstacle. Consequently, the specialist strongly recommended ICSI. Mark questioned the added expense, asking if standard IVF was a viable option. The doctor explained that, given Mark’s sperm profile, standard IVF carried a near 90% risk of complete fertilization failure. Thus, ICSI was not merely an option but a technical necessity.
Sarah and Mark accepted the recommendation, understanding the choice maximized their chance of getting even one embryo. Ultimately, the ICSI procedure achieved a high fertilization rate, yielding several quality embryos, leading to a successful pregnancy after an embryo transfer. Therefore, this example shows that the sperm quality, not just the cost, dictates the decision between IVF or ICSI. For similar options globally, see the Fertility Treatments Abroad Guide.
9. Advanced Considerations: PGT and Embryo Selection
Many patients opt to combine their fertilization cycle with genetic screening
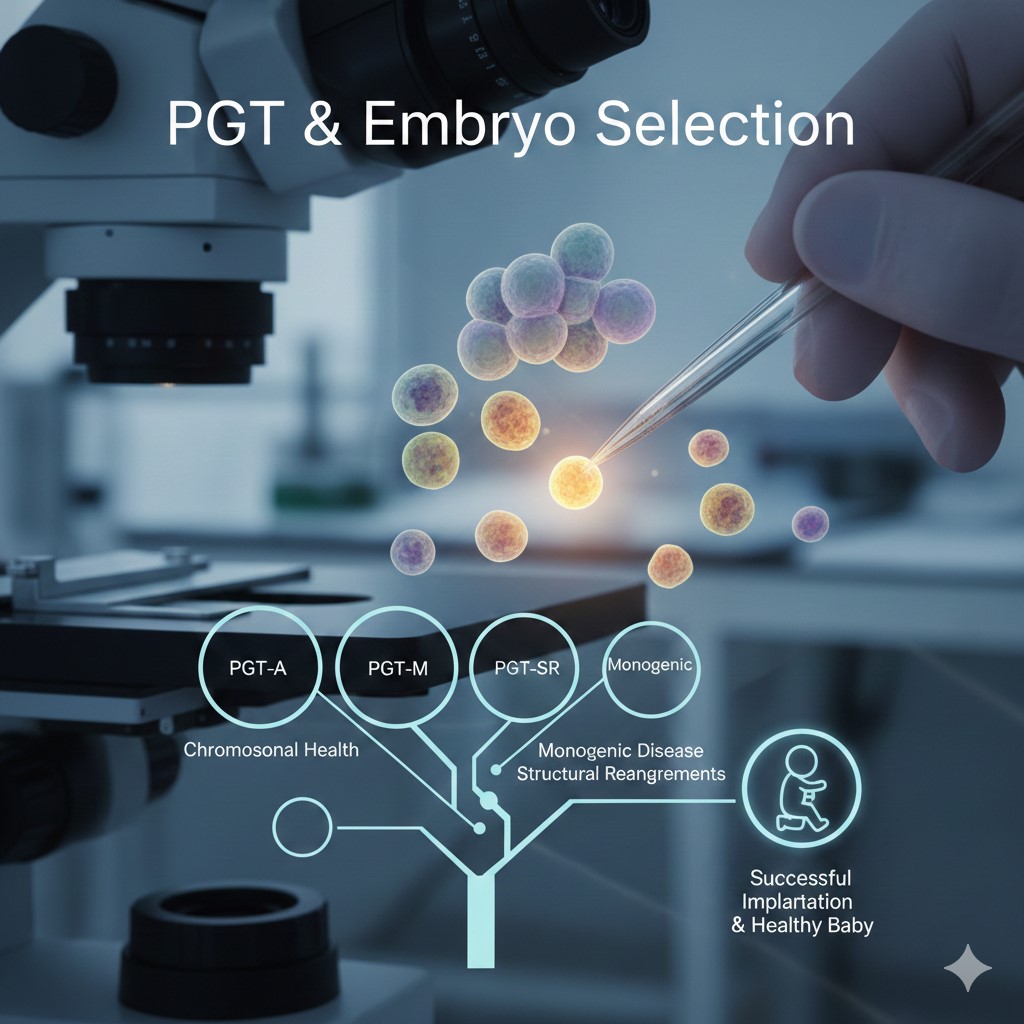
. This decision adds another layer of complexity to the choice between IVF or ICSI.
🧬 PGT Requirements and ICSI
Preimplantation Genetic Testing (PGT) involves biopsying a few cells from the embryo to test for chromosomal or genetic disorders. To ensure accurate results, laboratories must prevent any contamination from residual sperm DNA. Consequently, most fertility clinics mandate ICSI when performing PGT (including PGT-A for aneuploidy screening or PGT-M for monogenic diseases). The ICSI procedure meticulously cleanses the egg of extraneous sperm, providing a clean environment essential for the genetic testing process. This requirement often makes the choice automatic for couples seeking genetic screening or pre-conception gender selection.

🤖 New Methods in Fertilization
The field of ART rapidly evolves. New methods, including advanced sperm selection techniques and artificial intelligence integration, seek to improve both standard IVF and ICSI outcomes. Researchers explore techniques that better mimic natural selection, even within the lab environment, potentially refining the sperm selection process for ICSI. Furthermore, new non-invasive genetic testing methods (NiPGT) might reduce the contamination risk, challenging the universal ICSI requirement for all PGT cycles in the future. Learn more about these developments in our guide on New Methods in IVF.
10. Frequently Asked Questions (FAQ) About IVF or ICSI
Q1: Does ICSI affect the quality of the resulting embryo?
A: No, the fertilization technique itself does not inherently affect embryo quality. Embryo quality depends on the underlying quality of the egg and sperm and the environment of the lab culture. ICSI simply achieves fertilization when natural entry fails.
Q2: What happens if standard IVF fails to fertilize any eggs?
A: If standard IVF results in zero fertilization, doctors will highly recommend using ICSI in subsequent cycles. This ensures that the technical barrier is bypassed, maximizing the chances of fertilization in the next attempt. This is a common indication for switching to ICSI.
Q3: Can ICSI be used with donor sperm or donor eggs?
A: Yes, absolutely. Clinics frequently use ICSI with both donor sperm and donor eggs. They may use ICSI with donor sperm if the male partner has fertility issues, or they may use ICSI with donor eggs as a precautionary measure to maximize the number of fertilized eggs. This is common practice, especially when utilizing services for gamete donation.
Q4: Is there an age limit for undergoing ICSI treatment?
A: The age limit for ICSI is the same as for standard IVF, and it primarily relates to the age of the egg provider. Success rates drop significantly after the age of 40, regardless of the fertilization method used, because egg quality declines.
Q5: Do I need ICSI if I am pursuing gender selection?
A: Yes. If you pursue gender selection via PGT (Preimplantation Genetic Testing), ICSI is essentially mandatory. PGT requires a contamination-free sample, and only the manual single-sperm injection of ICSI provides the necessary control to prevent stray sperm from skewing the genetic results. Review our guide on the cost of fetal gender selection for more details.
Q6: How long does the ICSI part of the procedure take?
A: The actual injection process is highly specialized but relatively quick. An experienced embryologist typically requires only a few minutes per egg once they have prepared the eggs and isolated the sperm.
Q7: Does ICSI require more medication or stimulation than IVF?
A: No. The medication protocols for ovarian stimulation remain identical for both standard IVF and ICSI. The difference only occurs in the laboratory, post-retrieval.
Q8: Does ICSI help prevent polyploidy (multiple fertilization)?
A: Yes, ICSI often helps minimize the risk of polyploidy (when multiple sperm enter one egg). With standard IVF, the risk exists, but ICSI mitigates this risk by ensuring only a single sperm is placed inside the egg.
Q9: Can we use half ICSI and half standard IVF for the eggs?
A: Yes, clinics often recommend this approach (called split fertilization) for couples with a normal sperm analysis but a history of low fertilization. This method hedges the risk, testing the natural fertilization ability while ensuring a batch of eggs is fertilized via ICSI.
Q10: Are ICSI embryos transferable to a surrogate?
A: Absolutely. Once fertilization and subsequent embryo development occur, the resulting embryos are genetically and functionally equivalent to IVF embryos. Therefore, they are entirely suitable for transfer into the uterus of a gestational carrier. See our guide on surrogacy legal countries for related information.
Q11: Does ICSI change the embryo transfer process?
A: No. The embryo transfer process remains completely identical for embryos created by either standard IVF or ICSI. The method of fertilization does not influence the transfer technique.
Q12: Where can I find non-competitor sources on success rates?
A: Seek data from non-profit and government sources. High-quality, reliable, and non-competitive data comes from national registries, such as the Human Fertilisation and Embryology Authority (HFEA) in the UK or the Society for Assisted Reproductive Technology (SART) in the US, along with university research publications (NEJM) and World Health Organization (WHO) reports.
Q13: Does ICSI require different types of consent?
A: Yes. Because ICSI is a distinct procedure with specific indications, most clinics require an additional informed consent form acknowledging the procedure, its risks, benefits, and the associated added cost. This ensures both partners understand the manual fertilization aspect.