💎 Kidney Stone Treatment Surgery: The Definitive Guide to Modern Procedures
Navigating the pain and fear associated with kidney stones is tough. This comprehensive guide simplifies the choices for Kidney Stone Treatment Surgery, detailing everything you need to know about the modern, minimally invasive options available today.
✨ Executive Summary: Key Takeaways
Kidney stones, unfortunately, are a common and incredibly painful condition. While small stones may pass naturally, large or complex stones often require a definitive Kidney Stone Treatment Surgery. This section highlights the crucial points you need to grasp:
- The three primary surgical options are ESWL (shockwaves), URS (scope through the urethra), and PCNL (small incision for large stones).
- The choice of procedure depends on stone size, location, composition, and patient health. There is no one-size-fits-all solution.
- Modern surgical techniques are overwhelmingly minimally invasive, significantly reducing recovery time and hospital stays.
- Success is not just about removal; it's about prevention. A metabolic workup and lifestyle changes are essential post-surgery to prevent recurrence.
- For those considering medical travel, excellent urological care, including complex Kidney Stone Treatment Surgery procedures, is globally accessible. Understanding global regulations is key. (Global Regulations Guide)
🏥 When is Kidney Stone Treatment Surgery Necessary?
Many kidney stones pass spontaneously—a process hydration and pain management often aid. This, however, is often only true for stones smaller than 5 millimeters (mm).
Indicators for Surgical Intervention
An intervention becomes mandatory when the stone is larger, blocks the urinary tract, causes unrelenting pain, or leads to infection. Doctors will then recommend definitive Kidney Stone Treatment Surgery.
Significantly, the American Urological Association (AUA) guidelines strongly recommend intervention for stones greater than 10 mm, especially if symptomatic. Moreover, doctors also consider stones lodged in the ureter for over a month candidates for urgent removal because of the risk of permanent kidney damage.
Therefore, understanding the stone's size and location is the first critical step in choosing the right surgical path. Furthermore, certain types of stones, such as Struvite stones, have direct links to infection and demand complete removal, often via surgery, to eliminate the bacteria that formed them.
Factors Driving the Surgical Decision
Consequently, the decision to proceed with a Kidney Stone Treatment Surgery is rarely arbitrary. It depends heavily on several key patient and stone characteristics:
- Size and Location: Large stones (over 10-15 mm) or stones located in difficult-to-reach areas often necessitate more invasive options like PCNL.
- Symptoms and Complications: Persistent, severe pain (renal colic) that does not respond to medication, or signs of kidney infection (NIH Source), demand immediate surgical clearance.
- Anatomy: Unusual urinary tract anatomy or a solitary functioning kidney might alter the preferred surgical approach, prioritizing safety and stone clearance.
- Stone Composition: Hard stones, such as Cysteine or Calcium Oxalate Monohydrate, often resist non-invasive treatments like ESWL, making Ureteroscopy a better choice.
🛠️ Comprehensive Guide to Kidney Stone Treatment Surgery Options
Fortunately, surgical approaches for stone removal have evolved dramatically. They now cause far less trauma than traditional open surgery, focusing instead on keyhole techniques and energy-based fragmentation. Choosing the right method is paramount for effective stone clearance and minimizing recovery time. Indeed, this area of medicine, which falls under the Urological Surgery Department, requires high specialization.
🌊 1. Extracorporeal Shockwave Lithotripsy (ESWL)
The Non-Invasive Technique
ESWL is the least invasive of the Kidney Stone Treatment Surgery options. Specifically, it uses focused, high-energy acoustic shockwaves generated outside the body to target and shatter the stone into tiny pieces. The patient then passes these fragments naturally over the following days or weeks. This is typically an outpatient procedure that avoids any incisions or internal instrumentation.
Efficacy and Limitations
Consequently, ESWL remains a popular choice for stones less than 10-15 mm located in the kidney, often proving highly effective. However, success depends heavily on the stone’s hardness and location. Therefore, a patient may require several sessions to achieve complete stone fragmentation. This can lead to extended periods of passing fragments and related pain, which is similar to initial recovery phases in other procedures.
Pros and Cons of ESWL
✅ Pros
- Minimally invasive (no incision).
- Outpatient procedure (short recovery).
- Minimal need for anesthesia.
❌ Cons
- Requires stones to be passable; the patient must excrete fragments.
- Lower success rate for large or hard stones.
- Risk of "Steinstrasse" (stone street) requiring follow-up URS.
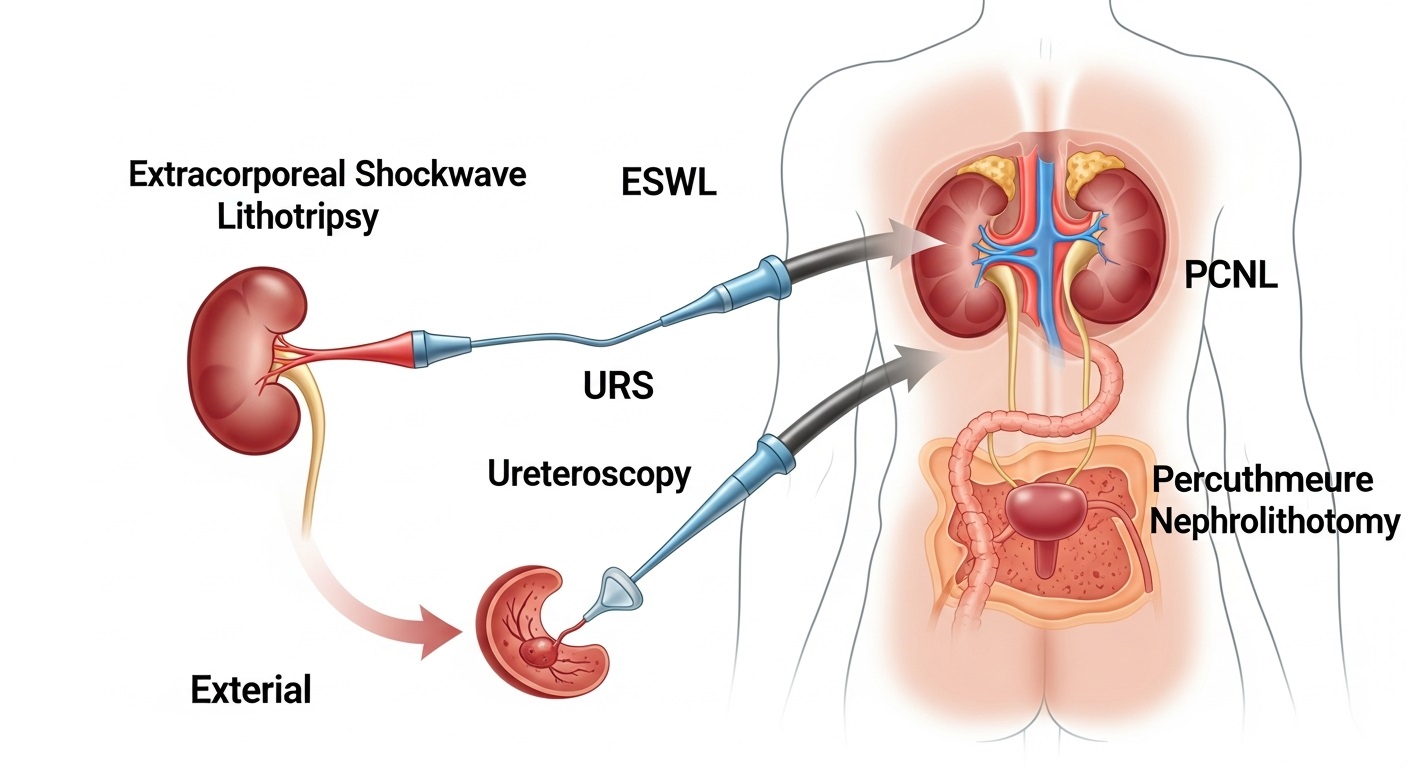
🔦 2. Ureteroscopy (URS)
Ureteroscopy involves passing a thin, flexible telescope (ureteroscope) through the urethra and bladder up into the ureter or kidney. Once the surgeon visualizes the stone, they can either grasp it with a basket or fragment it using a laser (Holmium laser lithotripsy). This technique, a crucial form of Kidney Stone Treatment Surgery, provides immediate stone clearance and allows the surgeon to treat stones anywhere in the ureter or kidney.
Because the surgeon removes the fragments, the patient avoids the painful process of passing stones afterward, a significant advantage over ESWL. Furthermore, doctors prefer URS for stones lodged in the ureter and for patients taking blood thinners. Typically, most URS procedures involve placing a temporary stent to prevent the ureter from swelling and blocking urine flow during healing. This is common practice in modern urological interventions, including those for urological oncology care.
Pros and Cons of URS
✅ Pros
- High stone-free rate (immediate clearance).
- Effective for stones in the ureter and hard stones.
- Excellent visualization of the urinary tract.
❌ Cons
- Requires general anesthesia.
- Stent placement often causes bladder irritation and flank pain.
- Small risk of ureteral injury.
⛏️ 3. Percutaneous Nephrolithotomy (PCNL)
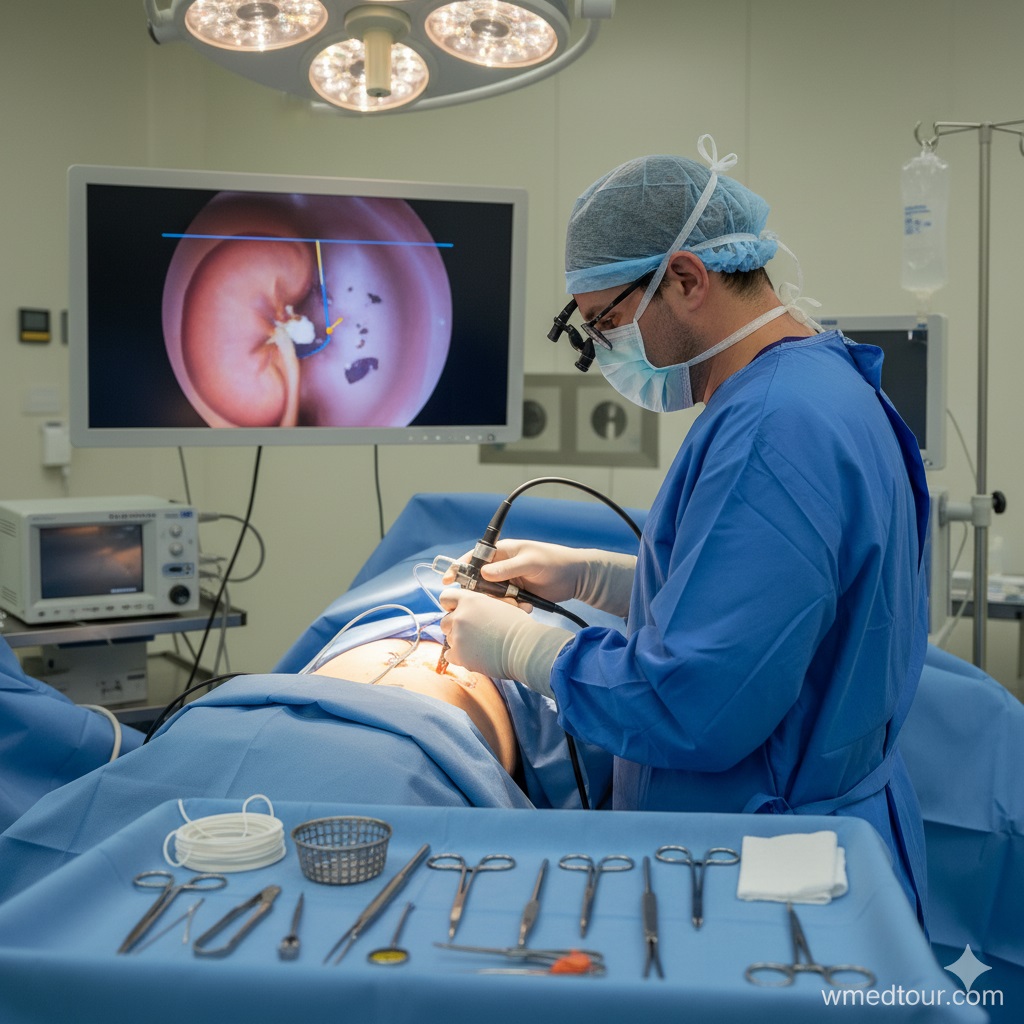
Percutaneous Nephrolithotomy is the gold standard for large or complex stones. Surgeons typically reserve it for stones exceeding 20 mm, or for Staghorn Calculi that fill the entire renal pelvis. This procedure involves making a small incision (about 1 cm) in the patient's back to create a tunnel directly into the kidney. The surgeon then inserts a nephroscope, fragments the stone, and removes it directly. As an advanced Kidney Stone Treatment Surgery, PCNL offers the highest stone-free rate for complex cases.
Given the complexity and invasiveness compared to ESWL and URS, PCNL requires general anesthesia and a short hospital stay, usually 2-4 days. This technique demands highly specialized skills, making the choice of clinic and surgeon critical, especially when considering medical travel. Consequently, we emphasize proper vetting when choosing a surgeon abroad. Furthermore, modifications like Mini-PCNL and Ultra-Mini PCNL use smaller tracts, successfully reducing post-operative pain and blood loss while maintaining efficacy, according to research from The Journal of Urology.
Pros and Cons of PCNL
✅ Pros
- Highest stone-free rate for large and complex stones.
- Definitive, often single-session treatment.
- Direct stone removal prevents fragment passage pain.
❌ Cons
- More invasive (small incision).
- Longer hospital stay (2-4 days) and recovery time.
- Small risk of bleeding or injury to adjacent organs.
🤖 4. Laparoscopic/Robotic Stone Removal (Rare Cases)
Laparoscopic or robotic surgery serves a tiny subset of highly complicated cases. These might involve anatomical abnormalities (e.g., horseshoe kidney), strictures, or situations where PCNL and URS have failed. While not a primary treatment for most simple stones, this advanced form of Kidney Stone Treatment Surgery allows surgeons to remove stones through several small ports in the abdomen or flank. They use it particularly if simultaneous corrective surgery (like a pyeloplasty to fix a blockage) is required. This aligns with the increasing global trend toward robotic surgery, which emphasizes minimal invasiveness for maximal efficacy. Consequently, the cost implications of these technologies are significant, making global price comparison a relevant factor for patients.
⚖️ Comparing Kidney Stone Treatment Surgery Techniques
When evaluating the best procedure, a direct comparison of the key metrics proves incredibly illuminating. However, the final decision always rests with a qualified urologist. They consider all variables to ensure the highest stone-free rate and quickest recovery possible.
| Feature | ESWL (Shockwave) | URS (Ureteroscopy) | PCNL (Keyhole Surgery) |
|---|---|---|---|
| Ideal Stone Size | < 15 mm | Any size in the ureter; < 20 mm in the kidney | > 20 mm or complex stones (e.g., Staghorn) |
| Invasiveness Level | Non-invasive | Minimally invasive (no incision) | Minimally invasive (1 cm incision) |
| Hospital Stay | Outpatient (Discharge same day) | Outpatient or Overnight (Rarely more than 1 night) | 2–4 Days |
| Primary Recovery Time | 1–2 Days | 2–4 Days (Stent discomfort may last longer) | 2–4 Weeks |
| Stone Clearance | Fragments passed over time (Lowest Stone-Free Rate) | Immediate fragmentation and removal (High Stone-Free Rate) | Immediate removal (Highest Stone-Free Rate) |
🗺️ Patient Journey: A Case Study in Kidney Stone Treatment Surgery
Case Profile: Mr. Omar's Challenge (The Large Stone)
Mr. Omar, a 55-year-old manager, began experiencing sudden, debilitating flank pain—classic renal colic. Initial imaging revealed a 2.5 cm (25 mm) stone in the renal pelvis of his left kidney. Given the size and composition (calcium oxalate), the urology team immediately ruled out ESWL and URS as primary treatments.
They determined this was due to the high likelihood of requiring multiple sessions and low clearance rates for a stone of this magnitude. This would have put undue stress on the patient.
The Kidney Stone Treatment Surgery Decision: PCNL
The definitive recommendation was Percutaneous Nephrolithotomy (PCNL), the most efficient form of Kidney Stone Treatment Surgery for large stones. Since Mr. Omar was considering combining his treatment with other services while traveling, he decided to look at highly specialized centers in the Middle East. After consulting with his chosen provider, he traveled to a top hospital in Iran known for its expertise in minimally invasive urological procedures, consulting with a renowned specialist.
Procedure and Recovery Timeline
- Day 1 (Surgery): Mr. Omar underwent the PCNL procedure under general anesthesia. The surgeon achieved 98% stone clearance in a single session, confirming the procedure's efficacy. They left a temporary nephrostomy tube in place.
- Day 2–3 (Inpatient Care): He received excellent post-operative care, with pain effectively managed. The surgical team monitored his kidney function closely, utilizing the hospital's advanced diagnostic capabilities.
- Day 4 (Discharge): The team removed the nephrostomy tube, and he was discharged with oral antibiotics and detailed instructions, including the pre-travel resources and checklists he had used to prepare.
- Post-Discharge: He stayed locally for another week for follow-up and stent removal. Ultimately, within two weeks, he returned to his routine, completely stone-free and focused on prevention through detailed dietary counseling, a necessary step following any complex stone removal procedure.
👤 Who is This For?
The information regarding Kidney Stone Treatment Surgery is vital for several groups:
Patients with Identified Stones
If you have recently received a diagnosis of a kidney stone, especially one greater than 5 mm, or are experiencing severe, chronic pain, this guide provides the necessary knowledge for an informed discussion with your urologist. For example, if your stone sits in the lower pole of the kidney, URS might be a better choice than ESWL, a subtlety an informed patient should know. Therefore, it helps you weigh the options between ESWL, URS, and PCNL based on your specific stone properties.
Medical Tourists Seeking Value and Quality
Individuals exploring global healthcare options—whether for specialized care, cost savings, or immediate access—must understand the precise procedure they require. The quality of Kidney Stone Treatment Surgery available in medical tourism hubs is globally competitive, often at a significantly lower cost. Therefore, due diligence in vetting specialists and facilities is essential, just as one would research the pricing for major orthopedic procedures.
Healthcare Professionals
Primary care physicians, nurses, and administrative professionals involved in patient counseling or medical records will find this a useful, consolidated reference. The focus on pros, cons, and recovery timelines aids in setting realistic patient expectations and facilitating referrals. Furthermore, staying current on the evolution of minimally invasive techniques is crucial. For further reading on surgical departments, see our section on minimally invasive urological surgery.
🌍 Global Considerations for Kidney Stone Treatment Surgery
Increasingly, patients look beyond local borders for high-quality, specialized care. When it comes to Kidney Stone Treatment Surgery, many international centers offer cutting-edge technology and experienced surgeons, often at highly competitive price points. This is particularly true for complex procedures like PCNL and flexible Ureteroscopy utilizing laser lithotripsy. For general knowledge on global care, explore our global medical tourism guide.
Quality and Accreditation Verification
The core challenge in medical travel involves verifying quality. Therefore, always seek hospitals with international accreditations (JCI, ISO) and surgeons who are board-certified and demonstrate high-volume experience in the specific Kidney Stone Treatment Surgery you need. This diligence mirrors the scrutiny applied to sensitive areas like kidney donation legalities, where ethical and legal standards are paramount.
Advanced Technology and Technique
Modern kidney stone care relies heavily on technology. Centers that invest in flexible digital ureteroscopes and high-power Holmium or Thulium lasers generally achieve better stone-free rates. Consequently, when researching clinics, ask specifically about their equipment. For example, the use of miniaturized PCNL equipment (Mini-PCNL) demonstrates a commitment to reducing invasiveness, reflecting trends also seen in advanced PCNL procedures.
Standardization in Global Urology
The standard of care for urological surgery remains consistently high in many top international hospitals. A detailed study by the University of California, San Francisco (UCSF), for instance, emphasizes that outcomes for ESWL and URS are generally standardized across major centers globally, provided the equipment and surgeon expertise are equivalent. However, complexities can arise when stones are calcified. In such situations, the energy source, like a laser, must be state-of-the-art to ensure complete stone disintegration.
The Trend Toward Minimally Invasive Care
The focus on minimally invasive techniques for stone removal is part of a broader trend in surgery. Furthermore, advancements in this area are leading to faster recovery times and less discomfort. This is similar to how technological advancements are changing procedures in plastic surgery, where precision tools allow for superior results and quicker healing. Consequently, when researching global options, look for centers showcasing evidence of high stone-free rates and low complication rates.
Post-Procedure Metabolic Workup is Non-Negotiable
Successful stone removal represents only half the battle; preventing recurrence is the ultimate goal. Recurrence rates for kidney stones are high—up to 50% within five years without preventative measures. Therefore, a high-quality surgical package must include a thorough post-operative metabolic workup, involving blood and 24-hour urine tests, and detailed dietary counseling. The patient must consider this preventative focus non-negotiable.
The Importance of Lifestyle Management
A paper published by The New England Journal of Medicine (NEJM) highlights that patient education on dietary changes based on stone composition is the single most effective tool for preventing future events. This emphasizes that the surgical part of the journey, while critical, must transition into a lifestyle management phase. This phase should be detailed and personalized. Thus, when comparing medical travel options, ensure the center provides a robust plan for the post-operative metabolic workup and follow-up.
🌱 Long-Term Outlook and Prevention After Kidney Stone Treatment Surgery
The long-term outlook following successful Kidney Stone Treatment Surgery is excellent, provided the underlying metabolic cause is addressed. For the vast majority of patients, life returns to normal quickly, without recurring episodes of renal colic. Nevertheless, the post-surgical period requires vigilance.
Prevention: The Real Cure
Analysis of the removed stone provides the map for prevention. Once the composition is known (Calcium Oxalate, Uric Acid, Struvite, etc.), doctors can begin targeted treatment. For instance, high fluid intake is a universal recommendation. However, for calcium oxalate stone formers, decreasing sodium and animal protein intake is critical. Furthermore, for uric acid stone formers, doctors typically prescribe medications that alkalinize the urine, a nuanced medical approach that requires specialist guidance. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) strongly emphasizes a dedicated follow-up plan for stone formers.
Importance of Follow-up Appointments
Regular check-ups with a urologist or nephrologist (kidney specialist) are vital. These appointments ensure that no new stones are forming and that the long-term health of the kidney is preserved. Ultimately, this ongoing relationship proves critical for managing chronic conditions.
Logistics and Quality in Global Care
The selection of an appropriate treatment center, whether domestically or internationally, should prioritize expertise and comprehensive post-care. Many patients find that international options provide a superior blend of high-tech care and affordability. However, the patient must always remember that successful stone removal, particularly a complex Kidney Stone Treatment Surgery, represents only the first step in a long-term commitment to kidney health. This requires a dedicated focus on dietary and lifestyle modifications. Thus, when evaluating options, ensure the surgical team provides a robust plan for the post-operative metabolic workup and follow-up.
The Long-Term Success Equation
The overall success of the Kidney Stone Treatment Surgery is often determined by adherence to these post-operative protocols. The meticulous planning required for recovery is paramount to ensuring successful outcomes. The dedication to follow-up should be as thorough as the pre-operative checklists used by patients preparing for travel for any major procedure.
Remember that the success of any Kidney Stone Treatment Surgery is not merely measured by the procedure's outcome but by the long-term prevention strategy you put in place. The best centers understand this distinction. For patients globally, choosing the right surgical path and the right partner for prevention makes all the difference in achieving a stone-free life.
❓ Frequently Asked Questions (FAQ) about Kidney Stone Treatment Surgery
To provide clarity and address common concerns, here are comprehensive answers to the most frequent questions regarding surgical interventions for kidney stones.
1. Can all kidney stones be treated with non-surgical methods?
No. While small stones (< 5mm) often pass spontaneously, stones larger than 10-15 mm, stones causing intractable pain or infection, or stones completely blocking urine flow usually require a surgical intervention like ESWL, URS, or PCNL.
2. What is the difference between a stent and a drain tube?
A stent (ureteral stent) is a thin, hollow tube placed inside the ureter during URS or PCNL to keep the tube open and ensure urine drainage from the kidney to the bladder. A drain tube (nephrostomy tube) is a temporary external tube inserted through the back directly into the kidney after a PCNL to drain urine or bleeding externally and stabilize the track.
3. Is general anesthesia always required for these procedures?
URS and PCNL typically require general anesthesia. ESWL can sometimes be performed with monitored sedation or regional anesthesia, but general anesthesia is often preferred to ensure the patient remains still for precise shockwave targeting. This is a crucial safety consideration.
4. What should I expect when passing stone fragments after ESWL?
Patients will pass small, sand-like fragments in the urine for days or weeks. This process can cause episodes of pain (renal colic) and blood in the urine. Increased fluid intake and prescribed pain medication are essential during this time.
5. How is the stone composition determined?
The stone fragments collected during URS or PCNL, or passed naturally after ESWL, are sent to a laboratory for chemical analysis. Knowing the composition (e.g., calcium oxalate, uric acid) is fundamental for planning long-term preventative care. The importance of this step cannot be overstated.
6. What is the primary indicator that I need PCNL instead of URS?
Stone size is the primary factor. Stones larger than 20 mm, or complex 'Staghorn' stones, are best treated with PCNL due to the superior stone-free rate, which minimizes the need for multiple, less effective, and costly follow-up procedures. This represents a significant investment in definitive care.
7. Can I travel internationally shortly after having a Kidney Stone Treatment Surgery?
While ESWL and URS allow for quicker travel, it is highly recommended to wait at least 3-7 days post-URS and 7-14 days post-PCNL. This allows the surgical site to stabilize and for any immediate complications (like significant bleeding or infection) to be managed before boarding a flight. Always follow your surgeon's specific medical travel clearance. Understanding the full scope of medical travel regulations is important here.
8. What does a metabolic workup involve, and why is it necessary?
A metabolic workup typically includes blood tests and one or two 24-hour urine collections. It is essential because it identifies the chemical imbalance (e.g., high calcium, low citrate) that caused the stone to form, allowing for tailored dietary and pharmaceutical prevention strategies. This is key to long-term success.
9. What are the signs of a potential post-operative infection?
High fever (above 101°F or 38.3°C), chills, persistent nausea, or pain that worsens dramatically after the initial recovery period are serious signs of infection or obstruction and require immediate medical attention. Never delay contacting your care team if these symptoms appear.
10. How long does the internal stent stay in after Ureteroscopy?
Stents are usually temporary, ranging from a few days to two weeks. The purpose is to prevent swelling and blockage. Surgeons typically remove them during a brief outpatient procedure once the ureter heals, ensuring complete clearance.
11. Is stone analysis performed for every patient who undergoes surgery?
Yes, stone analysis is a critical component of the post-operative plan. Medical professionals send all retrieved stone fragments to a lab to determine the exact chemical composition. Doctors then use this analysis to develop a personalized, long-term prevention strategy, drastically reducing the risk of recurrence.
12. Can I return to work immediately after ESWL or URS?
Patients typically return to light activity and work within one to two days after ESWL or URS, provided they are not experiencing severe pain from passing fragments or stent discomfort. However, PCNL requires significantly more recovery time, often two to four weeks, before patients can resume normal work duties.
13. What happens if a stone is too large for ESWL but too small for PCNL?
Ureteroscopy (URS) is the preferred treatment for stones that fall into this intermediate category (10 mm to 20 mm), especially those located in the ureter or the lower part of the kidney. URS offers a high stone-free rate with minimal invasiveness compared to PCNL, achieving complete clearance.
14. What are the long-term follow-up requirements for stone prevention?
Long-term follow-up typically involves initial post-surgical imaging (CT scan or X-ray) to confirm clearance, followed by the metabolic workup. Patients who form stones are generally advised to have annual follow-up visits with a urologist or nephrologist, including regular blood tests and repeat 24-hour urine collections to monitor the efficacy of the preventative regimen. This preventative diligence is as important as the initial surgery. (Preventive Care Guide)