Minimally Invasive vs Open Colectomy: Pros, Cons and Recovery Differences 🏥
Executive Summary 📋
Choosing between surgical methods for colon resection is a pivotal decision for patients. This guide explores the critical nuances of Minimally Invasive vs Open Colectomy: Pros, Cons and Recovery Differences. Key takeaways include:
- Minimally invasive techniques offer significantly faster return to daily life.
- Open surgery remains the gold standard for complex, large-scale tumors.
- Laparoscopic and robotic approaches reduce post-operative pain and scarring.
- Recovery timelines vary from 2 weeks for invasive methods to 8 weeks for open surgery.
Who is This For? 👥
This comprehensive analysis serves individuals diagnosed with colon cancer, diverticulitis, or inflammatory bowel disease (IBD). Furthermore, it provides medical professionals and caregivers with evidence-based comparisons to guide patient counseling. If you are exploring options within general surgery or looking for a specialist at our oncology department, this roadmap clarifies what to expect during your hospital stay and beyond.
Defining the Surgical Landscape 🌐
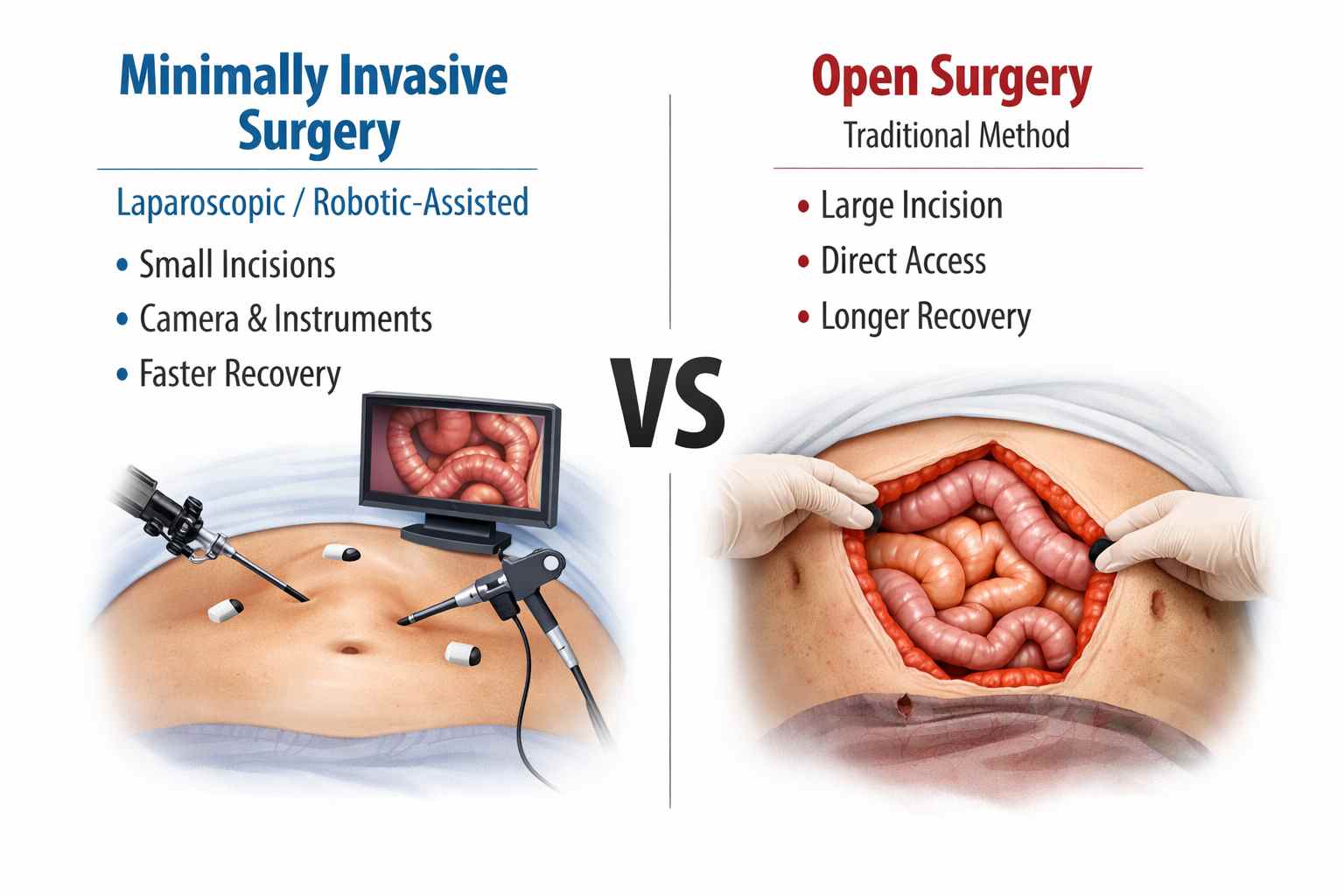
When a surgeon removes part or all of the colon, the technique used determines the patient’s immediate future. Minimally Invasive vs Open Colectomy: Pros, Cons and Recovery Differences often centers on how the surgeon accesses the abdomen. Historically, an open colectomy required a large vertical incision. Conversely, modern medicine emphasizes smaller ports. These smaller entries facilitate the use of cameras and specialized instruments.
At WMedTour, we believe in informed choices. Whether you are consulting with Dr. Abdulaziz Temiz or another expert, understanding the “why” behind the technique is vital. Technology has advanced so rapidly that many traditional “open” cases now utilize robotic assistance. This evolution has transformed the patient experience globally, especially in leading hubs like Iran and Turkey.
Minimally Invasive Colectomy: The Modern Standard ✨
A Minimally Invasive Colectomy is a type of colon surgery performed through small incisions rather than a large abdominal cut. It includes laparoscopic and robotic-assisted techniques.
Key points:
- Procedure: A tiny camera and specialized instruments are inserted through small “keyhole” incisions to remove the diseased part of the colon.
- Benefits:
- Smaller scars
- Less postoperative pain
- Shorter hospital stay (usually 2–5 days)
- Faster return to normal activities
- Techniques:
- Laparoscopic: Surgeon operates with instruments guided by a camera.
- Robotic-assisted: Surgeon controls robotic arms for greater precision and 3D visualization.
- Use: Ideal for localized colon problems, early-stage cancer, diverticulitis, or polyps that require surgery.
Minimally invasive colectomy aims to treat the condition effectively while minimizing trauma and speeding up recovery.
The Pros of Minimally Invasive Approaches
The primary advantage involves reduced physical trauma. Smaller incisions mean less blood loss and a lower risk of wound infections. Consequently, patients report much lower pain scores. This reduction in pain translates to a decreased reliance on opioid medications. Moreover, the aesthetic result is superior, as the scars are often barely visible after a year. Most importantly, bowel function typically returns faster, allowing patients to resume eating sooner.
The Cons of Minimally Invasive Approaches
Despite the benefits, MIS is not always suitable for everyone. It requires high-level technical expertise and specialized equipment. Because of the complexity, the time spent under anesthesia in the operating room might be longer. Additionally, if the surgeon encounters unexpected scar tissue or bleeding, they may need to “convert” to an open surgery mid-procedure. This risk is something we discuss extensively in our frequently asked questions.
Open Colectomy: The Traditional Powerhouse 🏛️
An open colectomy is a traditional colon surgery performed through a large abdominal incision, usually 6–8 inches long, to remove a diseased or damaged portion of the colon.
Additional details:
- Why it’s used: Open colectomy is preferred for complicated cases, large tumors, extensive scar tissue, or emergency situations where minimally invasive techniques aren’t safe.
- Procedure: The surgeon exposes the colon directly, removes the affected segment, and reconnects the remaining healthy parts (anastomosis).
- Recovery: Hospital stays are usually longer, around 5–8 days, with slower return to normal activities compared to laparoscopic or robotic surgery.
- Risks: Higher chance of wound infection, more noticeable scars, and greater postoperative pain.
- Outcome: Despite being more invasive, open colectomy is highly effective for removing diseased colon sections and resolving serious conditions such as cancer, blockages, or severe diverticulitis.
It remains an important option when precision and full access are critical for patient safety.
The Pros of Open Surgery
Open surgery offers the most direct access to the organs. Surgeons can manually feel the tissues, which is sometimes necessary to ensure all cancerous cells are removed. For patients with multiple previous abdominal surgeries, scar tissue (adhesions) can make laparoscopic entry dangerous. In these scenarios, an open approach is actually the safer choice. It also eliminates the risk of “conversion” since the surgeon already has full access.
The Cons of Open Surgery
The major drawback is the recovery period. A large incision takes longer to heal and carries a higher risk of incisional hernias. Patients generally experience more post-operative pain and require longer hospital stays. Furthermore, there is a higher incidence of lung complications, like pneumonia, because deep breathing is painful after a large abdominal cut. This makes early mobility, as discussed in our pre-operative consultations, even more critical.
Direct Comparison: Minimally Invasive vs Open Colectomy 📊
To better understand Minimally Invasive vs Open Colectomy: Pros, Cons and Recovery Differences, let’s look at the key data points in this comparison table.
| Feature | Minimally Invasive (Laparoscopic/Robotic) | Open Surgery |
|---|---|---|
| Incision Size | 3-5 small ports (0.5 – 1.5 cm) | 1 large incision (15 – 25 cm) |
| Average Hospital Stay | 2 to 4 days | 5 to 8 days |
| Post-Op Pain | Lower; usually managed with pills | Higher; often requires IV pain pump |
| Risk of Infection | Low | Moderate |
| Bowel Function Recovery | Rapid (24 – 48 hours) | Slower (3 – 5 days) |
Recovery Differences: What to Expect at Home 🏠
The divergence in Minimally Invasive vs Open Colectomy: Pros, Cons and Recovery Differences becomes most apparent once you leave the hospital. Patients who undergo MIS often feel “back to normal” by week three. However, open surgery patients often struggle with fatigue and incision pain well into the second month.
Early Activity and Diet
Regardless of the method, walking is your best medicine. After an appendectomy or a colectomy, moving helps the intestines wake up. For invasive methods, you might start eating solid food by day two. For open surgery, you may stay on a clear liquid diet for several days. We recommend consulting our checkup department for post-surgical nutritional monitoring.
Long-term Restrictions
Lifting restrictions are more stringent for open surgery. Because the large abdominal muscle was cut, there is a high risk of hernia if you lift heavy objects too soon. Minimally invasive patients must still be careful, but their risk is significantly lower. We always suggest a follow-up telemedicine consultation to verify when it is safe to return to the gym.
The Patient Roadmap: Your Journey with WMedTour 🗺️
Navigating colon surgery can be daunting, but a structured roadmap helps. Here is how WMedTour supports your Minimally Invasive vs Open Colectomy: Pros, Cons and Recovery Differences journey:
- Step 1: Medical Review. Send us your scans and reports via contact us.
- Step 2: Surgeon Match. We connect you with experts in laparoscopic surgery.
- Step 3: Travel Logistics. We arrange your stay in medical-friendly hotels in Mashhad or Istanbul.
- Step 4: The Procedure. High-tech surgery in JCI-accredited hospitals.
- Step 5: Recovery Support. On-ground assistance for medications and follow-up care.
Case Study: A Tale of Two Recoveries 🌟
Consider the case of Michael and Sarah, both 55 years old and diagnosed with sigmoid diverticulitis. Michael chose a traditional open colectomy in his home country. He spent seven days in the hospital and could not return to his office job for seven weeks. Sarah opted for a robotic-assisted colectomy through WMedTour in Turkey. She was discharged on day three. Surprisingly, Sarah was taking light walks through the local markets by day six and returned to her remote work within two weeks. This real-world divergence highlights why Minimally Invasive vs Open Colectomy: Pros, Cons and Recovery Differences is a topic every patient must research.
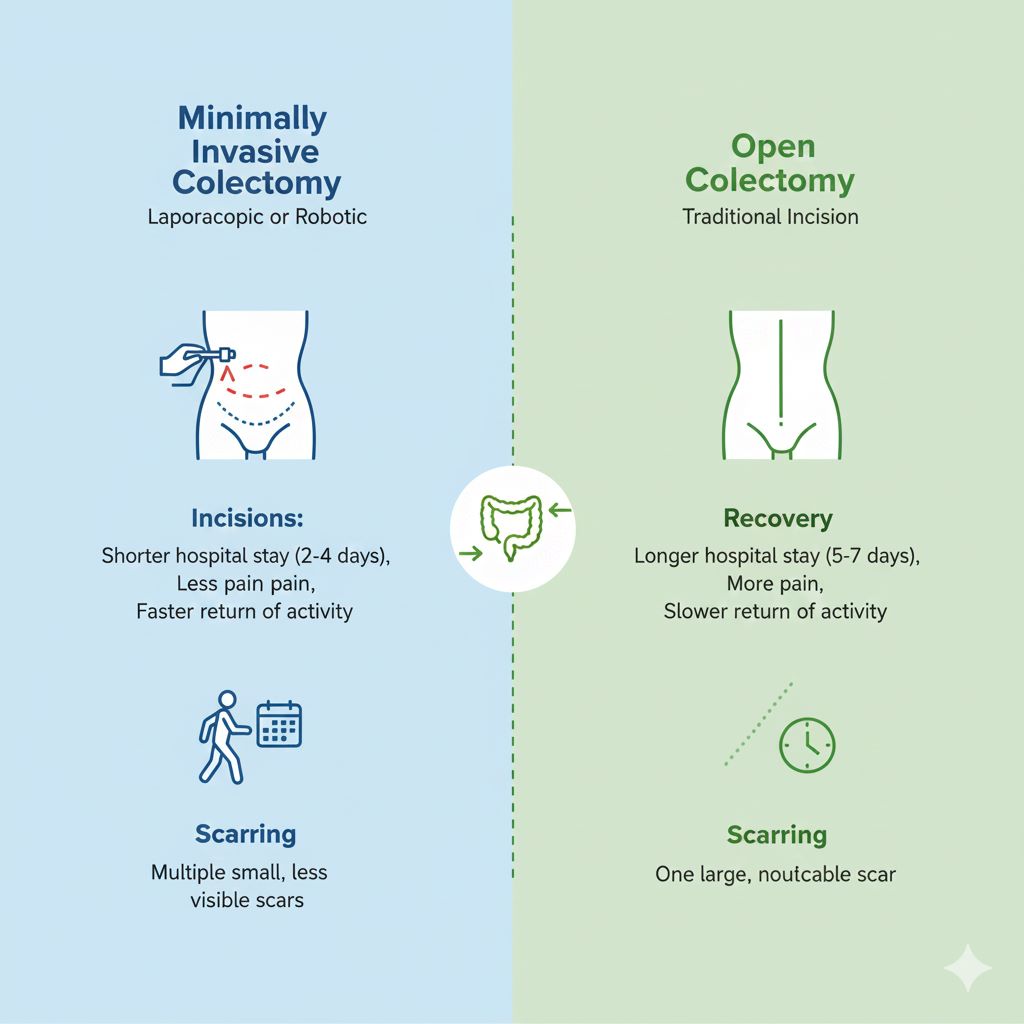
Surgery has come a long way! Today, many patients are candidates for Minimally Invasive (laparoscopic or robotic) surgery, which uses tiny cameras and small ports. However, Open Surgery remains a vital, life-saving option for more complex cases.
While the internal work on the colon is often similar, the way we get there affects your immediate recovery, scarring, and time spent in the hospital. Check out our comparison guide to see how these two methods stack up.
Always discuss with your surgeon which approach is safest and most effective for your specific needs! 🤝✨
Cost Analysis: Surgical Packages 💰
The cost of surgery is a major factor in medical tourism. Below is an approximate comparison of global prices for colectomy procedures.
| Destination | Minimally Invasive Cost (USD) | Open Surgery Cost (USD) |
|---|---|---|
| USA / UK | $35,000 – $50,000 | $30,000 – $45,000 |
| Iran (WMedTour) | $4,500 – $6,500 | $3,500 – $5,000 |
| Turkey | $8,000 – $12,000 | $7,000 – $10,000 |
Recovery & Tourism: Healing in Serenity 🌴
Why recover in a sterile room when you can heal in a beautiful destination? Many of our patients find that the psychological boost of “Healing Tourism” speeds up their recovery. After a tour in Iran or exploring the Bosphorus, the stress of surgery fades away. This is especially true for minimally invasive patients who are mobile enough to enjoy gentle sightseeing within a week. We ensure your itinerary remains low-impact, prioritizing your health at every step.
Medical Disclaimer ⚠️
The information provided here is for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. For high-level research, please refer to university sources such as Harvard Health or Johns Hopkins Medicine.
Frequently Asked Questions (FAQ) ❓
1. Can every patient choose a minimally invasive colectomy?
Unfortunately, no. While most patients are candidates for MIS, certain factors make open surgery necessary. These include very large tumors that cannot be removed through a small port, severe obesity, or extreme scar tissue from previous operations. Your surgeon will make the final determination during your pre-surgical assessment. The goal is always safety over technique. If the risk to the patient is too high, the surgeon will choose the open approach to ensure the best clinical outcome. We facilitate second opinions to ensure you are getting the most advanced care possible.
2. Is the cancer cure rate the same for both methods?
Yes, numerous university-led studies have shown that long-term survival and cancer recurrence rates are identical. Whether you choose Minimally Invasive vs Open Colectomy: Pros, Cons and Recovery Differences, the oncological outcome depends on the surgeon’s skill in removing the affected tissue and lymph nodes. As long as the surgeon achieves “clear margins,” the technique does not negatively impact your chance of a cure. Many patients prefer specialized oncology centers for this reason. These centers often have the highest volume of MIS cases, leading to greater precision.
3. How long does the actual surgery take?
A typical colectomy takes between 2 to 4 hours. Minimally invasive procedures often take slightly longer because of the setup of the robotic or laparoscopic tools. However, the time difference is usually only 30 to 60 minutes. Factors like your anatomy and the complexity of the disease play a bigger role in surgical duration than the method itself. Your surgical team will provide a more accurate estimate after reviewing your diagnostic tests. Regardless of the time, the focus remains on a thorough and safe resection.
4. What is the “conversion rate” from laparoscopic to open?
The conversion rate typically ranges from 5% to 15%, depending on the surgeon’s experience. This happens if the surgeon encounters unexpected bleeding, complex anatomy, or if the tumor is stuck to other organs. It is important to view conversion as a sign of a responsible surgeon who prioritizes your safety. If you are having surgery in a high-volume center, like those in our international network, the conversion rates are often on the lower end. Your surgeon will discuss this possibility during your consultation so you are fully prepared.
5. Will I have a permanent stoma bag?
Most colectomies do not result in a permanent stoma. In many cases, the surgeon can reconnect the two ends of the colon immediately. This is called an anastomosis. However, if the bowel is very inflamed, a temporary stoma may be used for 2-3 months to let the area heal. A permanent stoma is usually only required if the very end of the rectum is removed. We provide extensive support for proctectomy patients who may face these lifestyle changes. Modern appliances are very discreet and allow for a full, active life.
6. When can I travel back home after surgery?
For minimally invasive surgery, we recommend staying in the destination city for at least 7 to 10 days. For open surgery, you should plan for 14 to 21 days before flying. This “buffer” time is essential to ensure no late complications arise and that you are mobile enough for the journey. We can arrange for air ambulance services if a patient needs to return sooner for any reason. However, most patients enjoy this time as a relaxing period of convalescence. Our team monitors your vitals daily during this time.
7. How do I choose the best surgeon for this?
Look for a surgeon who performs at least 20-30 colectomies a year and has specific training in MIS. High-volume surgeons have significantly lower complication rates. You should ask about their specific experience with robotic platforms if you are interested in that route. At WMedTour, we vet all our doctors for their credentials, success rates, and patient feedback. We provide you with their full profiles so you can make an informed decision. Choosing a surgeon you trust is the most important step in your recovery journey.
8. Does insurance cover surgery abroad?
Some international insurance plans do cover procedures abroad, especially if the cost is lower than in your home country. However, many patients choose WMedTour because our package prices are lower than their deductible or out-of-pocket costs at home. We provide all the necessary medical coding and documentation to help you file a claim with your provider. For more details on budgeting, check our medical tourism guide. We aim for transparency in every financial transaction.
9. What is the risk of an incisional hernia?
The risk of a hernia is about 10-15% for open surgery but drops to less than 2% for minimally invasive methods. This is because the abdominal wall remains much stronger with smaller incisions. If you do have open surgery, wearing an abdominal binder and avoiding heavy lifting for 8 weeks is vital. We also offer hernia repair services if a complication arises later in life. Post-operative care is a lifelong commitment to your abdominal health. Regular exercise also helps maintain muscle integrity.
10. Are there specific diets to follow after a colectomy?
Immediately after surgery, a “low-residue” diet is best. This means avoiding high-fiber foods like raw vegetables, nuts, and seeds for a few weeks. These foods can be hard for a newly reconnected colon to process. Gradually, you will reintroduce fiber to help stabilize your bowel movements. Every patient is different, so keeping a food diary is a great idea. We offer nutrition consultations to help you transition back to a normal, healthy diet. Hydration is also key, as the colon’s job is to absorb water.
11. Can I have plastic surgery at the same time?
Generally, it is not recommended to combine a major bowel surgery with elective cosmetic procedures. Colectomy is a “clean-contaminated” surgery, which carries a higher risk of infection than a “clean” procedure like a tummy tuck. Combining them could increase your risk of wound complications. It is better to wait until you are fully recovered—usually 6 to 12 months—before considering plastic surgery. Your body needs to focus all its healing energy on the colon first. We can help you plan these procedures in stages for maximum safety.