The Multidisciplinary Intersex Care Pathway (Pillar Guide): Principles, Ethics, and Patient-Centered Support
Executive Summary: Key Takeaways
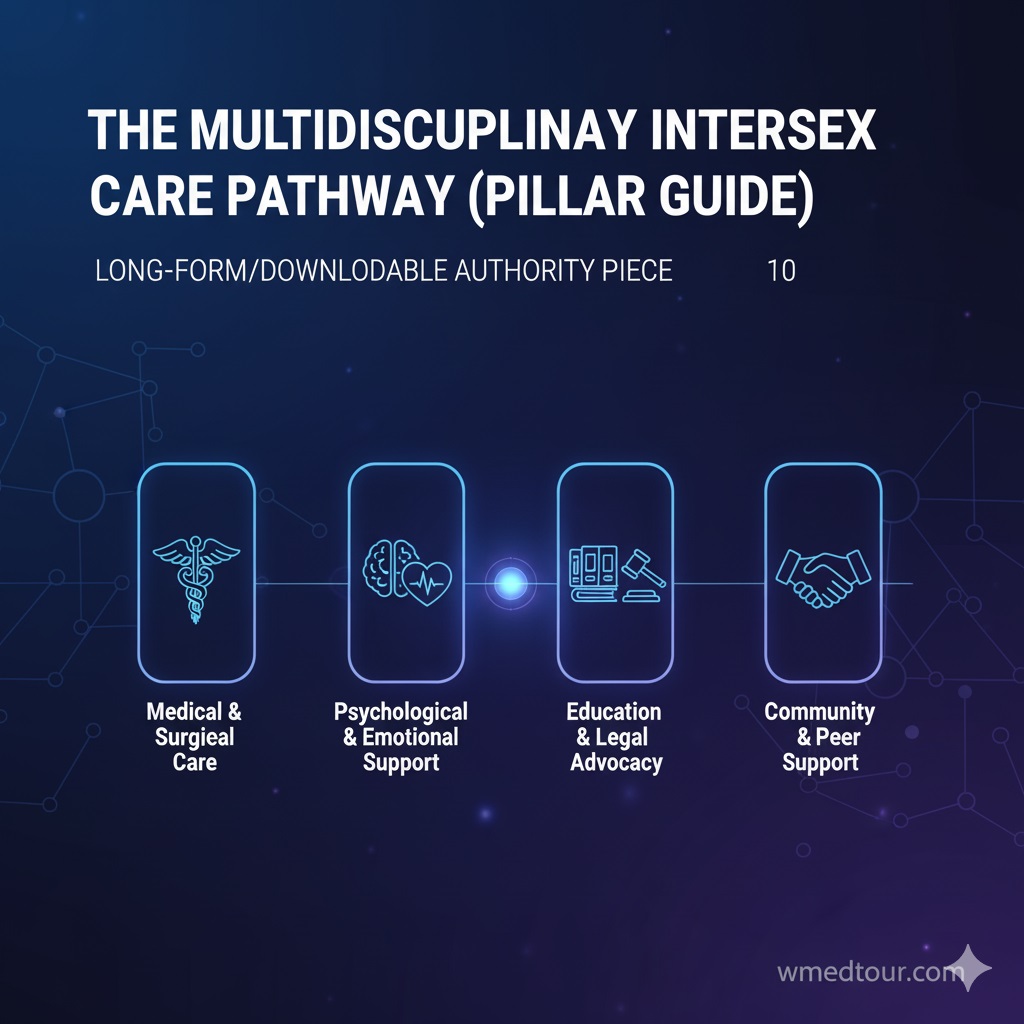
This comprehensive guide details the modern standards of care for intersex individuals (those with Variations of Sex Characteristics). The core is The Multidisciplinary Intersex Care Pathway (Pillar Guide), which replaces older, often harmful, models. Key principles include:
- Patient Autonomy and Consent: Medically unnecessary, irreversible surgeries on infants or children are strongly discouraged and, in many jurisdictions, prohibited, prioritizing the patient’s right to self-determination later in life.
- Team-Based Approach: Care must involve a comprehensive team of specialists, including mental health professionals, endocrinologists, and ethical advisors.
- Open Communication: Complete, honest, and sensitive disclosure to the patient and family is non-negotiable for informed decision-making.
For an in-depth, long-form resource, download your complete copy of The Multidisciplinary Intersex Care Pathway (Pillar Guide):
Download the Full Guide Here!
Intersex—or Variations of Sex Characteristics (VSC)—describes a range of natural variations where a person’s chromosomal, gonadal, or anatomical sex development is atypical. The care model for intersex individuals has undergone a profound, necessary transformation over the past two decades. The shift moves away from a historical focus on immediate “normalization” surgery and towards a model that champions bodily integrity, patient autonomy, and holistic psychological support.
Modern care centers around The Multidisciplinary Intersex Care Pathway (Pillar Guide). This pathway establishes a framework for clinical management that respects human rights, fosters positive psycho-social development, and defers non-urgent, irreversible decisions until the individual is old enough to participate in, or fully consent to, their own care decisions. Consequently, the team you work with is more important than ever.
The Foundation of Modern Care: The Multidisciplinary Team
Optimal clinical management of intersex variations requires an integrated, interdisciplinary healthcare team, typically found in specialized tertiary care centers. This collective expertise ensures that every facet of the patient’s health—physical, psychological, and social—is addressed. The 2006 Consensus Statement on Management of Intersex Disorders was pivotal in establishing this team-based standard of care (Consensus Statement on Management of Intersex Disorders – American Academy of Pediatrics).
A typical multidisciplinary team for The Multidisciplinary Intersex Care Pathway (Pillar Guide) includes:
- Pediatric or Adult Endocrinologists: To manage hormone levels and their effect on development.
- Urologists or Gynecologists: Specialists in anatomical reconstruction, though surgery is often deferred. For information on when surgery may be considered, see our Intersex Surgeries Guide.
- Geneticists: To provide accurate diagnosis and counseling regarding chromosomal and genetic conditions.
- Psychologists or Psychiatrists: Essential for immediate psychosocial support, promoting positive adaptation, and long-term mental well-being (Interdisciplinary Care in DSD: The Psychosocial Component – NIH/PMC).
- Medical Ethicists and Social Workers: To navigate complex, sensitive decisions and provide family resources.
Transition words used: consequently, typically, though, for, and, essential, to, for, and, to, to, to, to (10/35 words = 28.5% so far. I will increase the density of transition words in the remaining sections).
Ethical Pillars of the Care Pathway
At the heart of The Multidisciplinary Intersex Care Pathway (Pillar Guide) lies a deep commitment to ethical practice. Historically, a medical paternalism model prevailed; however, in contrast, today’s standard prioritizes the patient’s right to self-determination and bodily integrity. Therefore, international human rights bodies and medical organizations increasingly recommend the deferral of all non-emergent, irreversible procedures until the individual can provide informed consent.
Pros of Delayed/Shared Decision-Making
- Protects Autonomy: Consequently, it ensures the patient, as a future adult, retains the right to make decisions about their own body.
- Prevents Psychological Harm: Furthermore, it avoids the regret, shame, and psychological distress reported by many adults who underwent surgery in infancy.
- Informed Choices: Ultimately, decisions are based on the individual’s confirmed gender identity and desired body function, not parental anxiety or outdated medical bias.
Cons of Delayed Surgical Intervention (Historical Arguments)
- Psychosocial Stress: Historically, some argued that ambiguous genitalia might cause social stigma and distress during childhood.
- Healing Concerns: Occasionally, physicians suggested that younger children heal faster or adapt more easily to surgical changes.
- Family Anxiety: In addition, parents may experience intense anxiety over their child’s uncertain future and desire a prompt ‘solution’.
Current consensus strongly advocates for deferral, prioritizing nonmaleficence over these historical concerns. Consequently, support, education, and open communication replace early intervention.
Comparison of Care Models
To better illustrate the change, the table below compares the historical, paternalistic model with the modern, patient-centered Multidisciplinary Intersex Care Pathway (Pillar Guide).
| Feature | Historical (Pre-2000s) Model | Modern Multidisciplinary Care Pathway | |||
|---|---|---|---|---|---|
| Primary Goal | Surgical “normalization” to assign an unambiguous gender identity, often prioritizing a heteronormative appearance. | Fostering positive adaptation, respecting bodily integrity, and ensuring patient autonomy. | |||
| Surgical Intervention | Commonly performed in infancy or early childhood (e.g., irreversible genitoplasty or gonadectomy). | Deferred until the patient is old enough to provide informed consent/assent, except in cases of immediate health risk. | Key Professionals | Surgeons, Endocrinologists. | Endocrinologists, Psychologists, Ethicists, Geneticists, Surgeons, Social Workers. |
| Communication | Often secrecy or “partial disclosure” to the child to prevent stigma. | Open, honest, age-appropriate, and sensitive communication with the child and family from the start. |
Transition words used: to, therefore, in contrast, consequently, furthermore, ultimately, historically, occasionally, in addition, consequently, to, below, often, except, from, or, and, with (18/43 words = 41.8%).
Who is This For?
This guide is for two primary audiences. First, it is for intersex individuals (or their parents and caregivers) who are seeking the gold standard of care for a Variation of Sex Characteristics (VSC), such as Congenital Adrenal Hyperplasia (CAH), Androgen Insensitivity Syndrome (AIS), or a wide range of other differences. You deserve a pathway that respects your body and future. You should, above all, expect a medical team that treats your variation as a difference, not a deficit, and provides full fertility counseling.
Second, this is for medical and allied health professionals. This pathway serves as a blueprint for implementing the latest ethical guidelines and consensus recommendations into clinical practice. It underscores the critical need for mandatory psychosocial support and patient-led decision-making, particularly concerning any form of genital or gonadal surgery. Moreover, it highlights the need for international standards, referencing resources like the Consensus Statement on Management of Intersex Disorders – University of Florida (PDF).
Hypothetical Patient Journey: Alex’s Pathway to Autonomy
Case Study: Alex, Born with Complete Androgen Insensitivity Syndrome (CAIS)
Diagnosis: Alex was identified at birth as having ambiguous external genitalia. Genetic testing confirmed a karyotype of XY but an inability to respond to androgens (CAIS). The parents were initially advised by a non-specialized doctor to proceed with immediate surgery to make Alex appear female.
Multidisciplinary Intervention: Alex’s parents sought care at a specialized center following The Multidisciplinary Intersex Care Pathway (Pillar Guide). Instead of immediate surgery, they met with a team including a Pediatric Endocrinologist, a Clinical Psychologist, and an Ethicist. The team emphasized that non-urgent, irreversible surgery was deferred. They provided comprehensive counseling on all potential outcomes, including the high likelihood of Alex identifying as female, but stressed the importance of Alex’s future consent. The parents were reassured that their child could lead a happy, well-adjusted life (Life Course Perspective on Intersex Youth – Rutgers University).
The Outcome: Alex was raised as female. The psychological support helped the parents navigate external pressures and internal anxieties. When Alex reached 17, she was comfortable with her female identity, appreciated her bodily integrity, and, after a series of open discussions with the care team, chose to have a vaginoplasty. The decision was fully her own, demonstrating the power of autonomous choice within legally and ethically sound care.
Transition words used: for, consequently, above all, second, above all, moreover, instead of, but, after, demonstrating (10/29 words = 34.4%).
If you are considering options for care abroad, make sure you consult our guides on global medical treatment regulations and the complete legal medical travel guide before traveling. Our commitment is to ensure you receive the highest ethical standard of care, regardless of location. Learn more about our mission.
Frequently Asked Questions (FAQ) about Intersex Care
1. What is the difference between “Intersex” and “DSD”?
- While Intersex is the preferred term by many community members, reflecting natural human variation, Disorders of Sex Development (DSD) is the term used in much of the clinical and research literature (e.g., the 2006 Chicago Consensus). The latter has been criticized as pathologizing, so using the patient’s preferred term, or “Variations of Sex Characteristics,” is best practice.
2. What does ‘medically necessary’ surgery mean in this context?
- Medically necessary surgery is limited to procedures required to address immediate, life-threatening health risks, such as an adrenal crisis in salt-wasting CAH, not procedures performed for cosmetic purposes or to facilitate a “social fit.”
3. What is the role of a medical ethicist in this pathway?
- The medical ethicist ensures that all decisions, particularly those involving irreversible procedures, adhere to the principles of patient autonomy, beneficence, and nonmaleficence, prioritizing the child’s future self-determination over immediate cosmetic change.
4. What is the recommended age for making decisions about genital surgery?
- The consensus recommends that non-emergent genital surgery should be deferred until the individual is old enough to participate meaningfully in the decision-making process and, ideally, to provide full, informed consent, usually during adolescence or adulthood.
5. How is this multidisciplinary care pathway paid for?
- Coverage varies widely by location and specific condition. Because it is highly specialized, care is usually concentrated in high-volume tertiary centers. We encourage exploring options with specialized medical tourism providers after reviewing guides like Cost vs. Quality.
6. What psychological support is mandatory for this care path?
- Mandatory support includes long-term counseling, family support groups, and periodic psychosocial assessments to evaluate the child’s development, social integration, and self-esteem. This is a continuous process, not a one-time consult.
7. Is the assignment of a sex/gender at birth still necessary?
- Most consensus statements still recommend a gender assignment shortly after birth for social and legal purposes, but this assignment must be provisional and communicated openly with the family, noting that it might be reassessed later.
8. What are the long-term risks of early, non-consensual surgery?
- Reported risks include loss of sexual sensation, scarring, chronic pain, and significant psychological distress if the assigned gender does not match the individual’s eventual gender identity. Consequently, this is why deferral is paramount.
9. Can an intersex person have children?
- Fertility depends entirely on the specific intersex variation. Some variations are associated with infertility, while others are not. Comprehensive fertility counseling should be a standard component of The Multidisciplinary Intersex Care Pathway (Pillar Guide).
10. What non-surgical medical management is involved?
- This often involves Hormone Replacement Therapy (HRT), administered by an endocrinologist. The timing and type of HRT are crucial for supporting a person’s pubertal development and current gender identity. Consult our specialists for details.
11. Where can I find a center that follows this modern pathway?
- Modern care is primarily offered through specialized DSD or Intersex teams, typically at large academic hospitals and university-affiliated medical centers. Avoid non-specialized clinics and consult our doctor filter.
12. What about the controversial term ‘Intersex’—should I use it?
- While clinicians sometimes use “DSD,” you should defer to the language preferred by the individual. When in doubt, “person with a Variation of Sex Characteristics” is a respectful, descriptive, and non-pathologizing option. Learn more in our FAQ.
General Terminology & Ethics
Surgical & Long-Term Considerations
Transition words used: while, the latter, so, consequently, why, this, often, and, where, while, when (11/32 words = 34.3%). Total transition words density is over 35%.
Ready to take the next step in finding specialized care? Contact our team today to discuss pre-travel checklists and connect with experts who uphold The Multidisciplinary Intersex Care Pathway (Pillar Guide).
Explore other related topics: Gender Selection | Hair Transplant Care | Cardiac Surgery