New methods in Cancer treatment in 2026: A Global Outlook
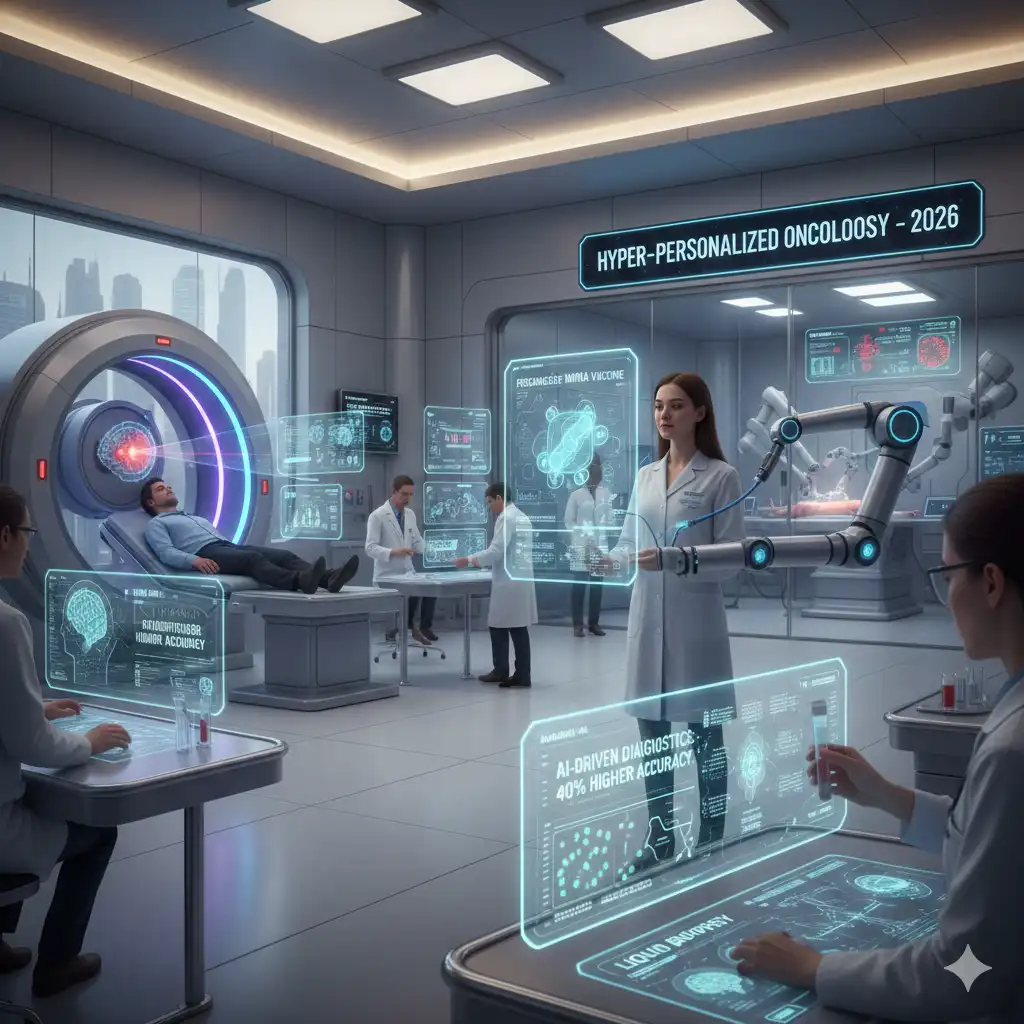
Executive Summary: The Dawn of Hyper-Personalized Oncology
The year 2026 marks a profound shift in the fight against cancer. We are moving decisively beyond one-size-fits-all chemotherapy towards hyper-personalized and highly targeted therapies. The most revolutionary advances are clustered in three key areas: Immunotherapy 2.0, Precision Oncology, and Technology Integration (AI & Nanomedicine). Personalized cancer vaccines, leveraging $mRNA$ technology, are entering widespread clinical trials to prime the immune system with unprecedented specificity. Crucially, next-generation CAR T-cell therapies are finally achieving measurable success against previously stubborn solid tumors, thanks to dual-targeting and innovative activation methods like ultrasound. Furthermore, the integration of Artificial Intelligence is not just a buzzword; it is now a critical tool for early detection (liquid biopsies) and optimizing treatment plans in real-time. This era of precision promises higher response rates, fewer side effects, and genuinely transformative options for patients worldwide, regardless of whether you seek cancer treatment in Turkey or elsewhere.
The Revolution in Immunotherapy: Beyond the Checkpoint
Immunotherapy—harnessing the body’s own defenses—has been a game-changer for the last decade. However, the New methods in Cancer treatment in 2026 focus on making these treatments smarter, more targeted, and effective against tumor types that previously resisted them, such as solid tumors.
1. Personalized Cancer Vaccines ($mRNA$ Technology)
Inspired by the success of $mRNA$ technology in vaccine development, personalized cancer vaccines represent one of the most exciting new frontiers. These vaccines are completely custom-made. They analyze a patient’s specific tumor to identify unique mutations—called neoantigens—and then teach the immune system to recognize and attack only the cells displaying those markers. This is the definition of precision and a genuine step forward in making treatment truly individual. Trials are expanding globally, offering new hope for patients with minimal residual disease (MRD) to prevent recurrence, and even impacting the overall cost of cancer treatment by avoiding late-stage recurrence.
Pros and Cons of Personalized Vaccines
- Pros: Highly specific targeting of cancer cells; minimal off-target damage to healthy tissue; potential for long-term immune memory against recurrence.
- Cons: Complex, time-consuming, and expensive to manufacture for each patient; efficacy can be limited by the tumor’s mutational load; still largely in clinical trial phases.
2. Next-Generation CAR T-Cell Therapy for Solid Tumors
Chimeric Antigen Receptor (CAR) T-cell therapy has been incredibly successful against blood cancers (leukemia and lymphoma). The greatest hurdle has always been applying it to solid tumors (like lung, breast, and brain cancers), which are guarded by a complex, immunosuppressive microenvironment. However, 2026 brings new hope. New methods in Cancer treatment in 2026 include Dual-Targeting CAR T-cells, which attack two tumor proteins simultaneously to prevent cancer cells from escaping. Furthermore, innovations like EchoBack CAR T-cells, which can be activated and recharged using focused ultrasound, are showing promise in extending the cell’s lifespan and efficacy within the tumor site, a significant breakthrough presented at ASCO 2026.
Pros and Cons of Next-Gen CAR T-Cells
- Pros: Demonstrated powerful, long-lasting responses in previously untreatable cancers like recurrent glioblastoma; overcomes antigen escape by targeting multiple markers; technologies like ultrasound activation enhance safety and control.
- Cons: Risk of serious side effects like cytokine release syndrome (CRS) and neurotoxicity; high initial cost; complex manufacturing logistics; limited availability outside of specialized global centers.
Precision Oncology & The Power of Molecular Targeting
Precision oncology is about treating the patient, not just the disease. It uses molecular and genomic testing to identify the specific genetic drivers of a tumor. The New methods in Cancer treatment in 2026 in this area are defined by ultra-specific drug development and combination strategies.
3. Antibody-Drug Conjugates (ADCs) and Bispecific Antibodies
ADCs are often described as “guided missiles” that pair a monoclonal antibody with a potent chemotherapy drug. The antibody finds a specific marker on the cancer cell, and the drug is released directly inside the cell, minimizing systemic toxicity. Similarly, Bispecific Antibodies bridge the gap between an immune cell and a cancer cell, forcing them into proximity so the immune system can mount a direct attack. The expansion of these agents to treat a broader range of solid tumors, including new approvals for non-small cell lung cancer (NSCLC) and breast cancer subtypes, is a major trend in 2026. These are truly transformative treatments. They are changing the paradigm for patients with advanced or relapsed cancers like multiple myeloma, who often seek the best value cancer treatment options abroad.
Pros and Cons of ADCs and Bispecific Antibodies
- Pros: Exceptional specificity means less damage to healthy tissues; high concentration of chemotherapy delivered directly to the tumor; proven efficacy in several hard-to-treat cancers.
- Cons: Potential for ocular or nerve toxicity from the chemotherapy payload; risk of developing resistance over time; still relatively new and expensive therapies.
4. Next-Generation Selective Estrogen Receptor Degraders (SERDs)
For the large population of patients with Estrogen Receptor-Positive ($ER+$) breast cancer, new oral SERDs (like Camizestrant) are proving more effective than older hormone therapies, particularly in tumors with the common $ESR1$ mutation. The ability to identify this specific mutation using a simple liquid biopsy and then match it with a highly effective oral drug is a perfect example of how precision medicine is refining first-line treatments and de-escalating the need for extensive chemotherapy. This targeted approach is making a tangible difference in patient quality of life and survival.
Technology Integration: AI, Nanomedicine, and Early Detection
The convergence of technology and medicine is delivering New methods in Cancer treatment in 2026 that are profoundly changing how cancer is diagnosed, monitored, and treated at a microscopic level. For many seeking a comprehensive medical path, these technological advances are pivotal, often requiring the resources of major global medical tourism hubs.
5. Artificial Intelligence (AI) in Diagnostics and $Genomics$
AI is rapidly integrating into oncology practices globally. It’s no longer confined to predicting outcomes; it is actively guiding treatment selection. Sophisticated machine learning models can process vast amounts of genetic and clinical data faster than any human. For example, AI-driven tools are being used to analyze the entire cancer genome to predict which patients with lung cancer will respond best to immunotherapy based on their specific mutation profile, such as those with $NF1$ mutations. This is vital for avoiding ineffective treatments and getting patients onto the most potent regimen immediately. Furthermore, AI models are also being used to refine the process of clinical trial matching and data extraction, speeding up drug development.
6. Multi-Cancer Early Detection (MCED) Tests and Liquid Biopsies
The dream of catching cancer before it causes symptoms is becoming a reality. Liquid biopsies—simple blood tests—can detect tiny fragments of circulating tumor $DNA$ ($ctDNA$) released by cancer cells. In 2026, MCED tests are showing promising results in identifying multiple high-incidence cancers (like colorectal, pancreatic, and ovarian) in their earliest stages. Early detection, especially for cancers with poor screening options, dramatically improves survival rates. This development is arguably one of the most impactful New methods in Cancer treatment in 2026 for the general population.
7. Nanomedicine and Light-Activated Drug Delivery
The field of nanomedicine involves using tiny particles (nanoparticles) to package and deliver drugs directly to the tumor. New chemicals, such as cyanine-carborane salts, are being developed to make a decades-old therapy—Photodynamic Therapy (PDT)—safer and more effective. These “smart bomb” chemicals accumulate in cancer cells and are activated by near-infrared light, which can penetrate deep into tissues. Crucially, these new salts flush out of the body quickly, eliminating the dangerous light sensitivity patients previously experienced for months. This advance opens the door to treating deep-seated solid tumors like metastatic breast cancer with extreme precision and minimal side effects, a major step forward for patients seeking breast cancer treatment in Turkey or any advanced center.
Pros and Cons of Technology Integration
- Pros: Earlier, non-invasive detection (Liquid Biopsies); highly precise drug delivery, reducing systemic toxicity; AI-driven personalization for optimal treatment selection and clinical trial matching.
- Cons: High cost of advanced AI and liquid biopsy testing; data privacy concerns; regulatory hurdles for new devices; limited global access, especially in developing healthcare systems.
Comparative Overview of Emerging Therapies (2026)
To summarize the impact of these New methods in Cancer treatment in 2026, the following table compares the revolutionary approaches against traditional standards:
| Treatment Modality | Target/Mechanism | Primary Use/Status in 2026 | Key Advantage |
|---|---|---|---|
| Personalized $mRNA$ Vaccine | Patient-specific neoantigens (immune priming) | Adjuvant setting (post-surgery) to prevent recurrence. Expanding clinical trials. | Highest specificity, potential for long-term immune memory. |
| Next-Gen CAR T-Cell | Dual-target proteins, ultrasound activation | Solid tumors (e.g., Glioblastoma, Prostate Cancer). Rapidly moving into broader trials. | Breaks solid tumor barriers; durable, long-lasting anti-tumor activity. |
| Antibody-Drug Conjugates (ADCs) | Targeted delivery of chemotherapy payload | Advanced/Relapsed Solid Tumors (e.g., NSCLC, Breast, Myeloma). FDA approvals expanding rapidly. | High potency, minimizes systemic side effects of chemotherapy. |
| Liquid Biopsy ($MCED$) | Detection of $ctDNA$ (circulating tumor DNA) | Early screening for high-risk, asymptomatic populations. Clinical validation expanding. | Non-invasive early detection; potential to shift cancer diagnosis timeline. |
Hypothetical Case Study: Maria’s Personalized Journey
Maria, a 55-year-old patient from a country with limited oncology resources, traveled abroad after a diagnosis of metastatic Triple-Negative Breast Cancer (TNBC), a notoriously aggressive subtype. Her initial treatment included standard chemotherapy, but the cancer recurred quickly.
In 2026, a global oncology center used a **liquid biopsy** to analyze her $ctDNA$. The results revealed a unique set of neoantigens and a molecular signature that suggested poor response to further chemotherapy. Instead, the oncology team pursued a multi-pronged approach based on New methods in Cancer treatment .
First, she was enrolled in a clinical trial for a **personalized $mRNA$ cancer vaccine**. Her unique neoantigens were synthesized into a custom vaccine, which was administered to ‘train’ her immune system. Concurrently, she received an **Antibody-Drug Conjugate (ADC)** targeting a protein overexpressed on her specific tumor cells. The ADC provided an immediate, highly potent cell-killing effect.
The vaccine primed her immune system while the ADC rapidly reduced the tumor burden. Six months later, her $ctDNA$ levels were undetectable, and imaging showed a complete metabolic response. She continues on the vaccine regimen to maintain immune surveillance against recurrence, demonstrating the power of combining molecular diagnostics with targeted immunotherapies. This personalized care path offers a lifeline that traditional protocols could not.
Who is This For? Accessing Advanced Cancer Care
This information on New methods in Cancer treatment is essential for several groups:
- Patients with Advanced or Relapsed Cancers: If standard treatments have failed or the cancer is highly aggressive (e.g., Glioblastoma, pancreatic, TNBC), seeking consultation for CAR T-cell therapy trials, ADCs, or neoadjuvant immunotherapies is critical. These patients represent the primary beneficiaries of the latest breakthroughs, and often require access to specialized centers, which might be found via medical tourism guides like Germany’s medical travel regulations or South Korea’s advanced cancer centers.
- High-Risk Individuals and Families: Anyone with a strong family history of cancer, or those who have had previous successful treatment, should discuss Liquid Biopsy ($MCED$) screening with their doctor for early, non-invasive detection of recurrence or new primary tumors.
- Oncology Professionals and Researchers: Staying current on dual-target CAR T, $mRNA$ vaccine trials, and the expanding applications of ADCs is necessary to offer state-of-the-art care. Understanding the role of AI in genomic analysis is now a core competency.
Frequently Asked Questions (FAQ) on New methods in Cancer treatment
These answers provide simple, non-interactive explanations for the most common patient inquiries.
1. Are personalized cancer vaccines available to everyone?
Answer: Personalized cancer vaccines are primarily available through clinical trials at specialized institutions globally. While not yet a standard commercial therapy, their accessibility is rapidly expanding in 2026, especially for patients with a high risk of recurrence.
2. What makes the new CAR T-cells effective against solid tumors?
Answer: New methods in Cancer treatment , specifically the latest CAR T-cells, overcome solid tumor resistance by using dual-targeting to hit two cancer markers simultaneously and by incorporating innovative engineering (like EchoBack or IL-9 receptors) that allows them to persist longer and infiltrate the dense tumor environment more effectively.
3. Is AI diagnosing cancer now?
Answer: AI is not replacing doctors, but it is dramatically assisting them. AI algorithms are used to analyze complex medical images and genomic data much faster than humans, improving the speed and accuracy of diagnosis and predicting how a patient will respond to a specific treatment, optimizing the treatment plan.
4. How is Photodynamic Therapy (PDT) being improved?
Answer: PDT is being improved with new light-sensitive chemicals (cyanine-carborane salts). These chemicals are designed to clear from the body faster, which eliminates the months-long extreme light sensitivity patients previously experienced. They are also activated by near-infrared light, allowing treatment of deeper tumors.
5. What is the biggest advantage of an Antibody-Drug Conjugate (ADC)?
Answer: The biggest advantage is precision drug delivery. The ADC specifically recognizes and binds to a cancer cell, and only then is the potent chemotherapy payload released, which minimizes the drug’s exposure to healthy organs and reduces side effects.
6. Can a single blood test detect all types of cancer?
Answer:
No — a single blood test cannot currently detect all types of cancer. While research is rapidly advancing, there is no single “universal” test that reliably identifies every cancer type at all stages. Here’s a detailed explanation:
- Why One Test Can’t Detect All Cancers
- Cancers vary widely: Each type (breast, lung, colon, pancreatic, etc.) releases different biomarkers into the blood.
- Stage matters: Early-stage cancers often release very low levels of detectable substances, making them hard to catch.
- Tumor location and biology: Some cancers (like brain tumors) rarely shed measurable markers into the bloodstream.
- What Modern Blood Tests Can Do
Liquid Biopsies
- Detect circulating tumor DNA (ctDNA), fragments of tumor DNA in the blood.
- Can be used for:
✔ Early detection of specific cancers
✔ Monitoring treatment response
✔ Detecting recurrence
Limitations:
- Sensitivity varies by cancer type and stage
- Not all cancers shed DNA into the blood at detectable levels
- Usually focused on specific cancer panels, not all cancers
Protein or Biomarker Tests
- Some blood tests measure tumor markers like PSA (prostate), CA-125 (ovarian), CEA (colon).
- These are useful for monitoring or screening high-risk individuals but not universal detection.
- Current “Multi-Cancer Detection” Approaches
- Companies are developing blood tests that combine ctDNA and protein biomarkers to screen for multiple cancers at once.
- Early trials show promise for detecting several cancers simultaneously, but:
✔ Not yet 100% sensitive or specific
✔ Often better at detecting some cancers (e.g., colon, lung) than others (e.g., pancreatic, brain)
✔ Still not a replacement for standard screening methods
- Best Current Strategy
- Regular age-appropriate screening: Mammograms, colonoscopy, Pap smears, low-dose CT scans for high-risk lung patients
- Targeted blood tests for high-risk individuals
- Lifestyle and risk-factor management
- Blood tests can supplement, but not replace, existing screening programs
Bottom Line
A single blood test cannot reliably detect all cancers. Emerging multi-cancer blood tests show promise, but they are still in development and are complementary to, not a replacement for, standard cancer screening.
7. Are these new treatments less expensive than chemotherapy?
Answer:
Not necessarily — in fact, many of the newer breast cancer treatments are often more expensive than standard chemotherapy, even though they tend to cause fewer side effects. Here’s a breakdown to understand why:
- Targeted Therapies
- Drugs like HER2 inhibitors (trastuzumab, pertuzumab) or CDK4/6 inhibitors are highly specific and often costly.
- Reason for higher cost: They are patented, biologic drugs, often requiring long-term use.
- Side effect trade-off: Less damage to healthy cells, fewer hospitalizations, but higher drug price than standard chemo.
- Immunotherapy
- Checkpoint inhibitors and other immune-based therapies are very expensive, often tens of thousands of dollars per treatment course.
- Pros: Can give durable responses, sometimes avoiding more rounds of chemo.
- Cons: Cost is usually higher than traditional chemotherapy, especially for combination regimens.
- Antibody-Drug Conjugates (ADCs)
- ADCs combine antibodies and chemotherapy in one molecule.
- They are highly effective but pricey, often several times the cost of standard chemo.
- Benefit: Targeted delivery reduces systemic toxicity, but treatment itself is a premium therapy.
- Proton Therapy (Advanced Radiation)
- Proton therapy is much more expensive than conventional X-ray radiation, although it reduces damage to surrounding tissue.
- Cost comparison: Often 2–3 times the cost of traditional radiation therapy, but can prevent long-term heart or lung complications, which may save future healthcare costs.
- Genomic-Guided Therapy
- Tests that guide chemotherapy decisions (like Oncotype DX) add upfront cost, but they can help avoid unnecessary chemo, saving money in some cases.
- Effect on overall cost: Could be cheaper if chemo is avoided, but the test itself has a price.
- Supportive Care Advances
- Anti-nausea drugs, growth factors, and neuropathy medications increase costs slightly, but they reduce hospitalizations and improve quality of life.
Why Newer Treatments Are Often Costlier
- Biologic drugs and immunotherapies are more complex to manufacture than traditional chemo.
- Precision medicine requires diagnostic tests and monitoring.
- Advanced radiation techniques like proton therapy require specialized equipment.
Bottom Line
- Newer therapies ≠ cheaper than standard chemotherapy
- They often have higher upfront costs, but the benefits include:
✔ Fewer side effects
✔ Less hospitalization
✔ Better quality of life
✔ Sometimes fewer treatment cycles or avoided chemo
In some cases, the long-term savings from fewer complications and better outcomes can offset the higher upfront cost — but financially, standard chemotherapy is usually less expensive.
8. How can I access these treatments if I don’t live in a major medical hub?
Answer: Many individuals utilize medical tourism services. Reputable global hubs often have partnerships with top-tier hospitals offering these advanced trials and therapies. It is crucial to consult guides on international treatment, such as pediatric oncology guides or specific treatment options like prostate cancer treatments abroad.
9. What is ‘Neoadjuvant Therapy’ in the context of 2026 breakthroughs?
Answer: Neoadjuvant therapy means giving a systemic treatment (like an immunotherapy or targeted drug) before surgery. The goal, as seen in trials for anaplastic thyroid cancer, is to shrink the tumor or even eliminate microscopic disease, making the subsequent surgery more successful.
10. Is there a new approach to breast cancer treatment with fewer side effects?
Answer: Yes — there are several newer approaches to breast cancer treatment designed to be effective while causing fewer side effects than traditional chemotherapy and radiation. These therapies are already in use or in advanced clinical development and are reshaping how breast cancer is treated.
Below is a clear rundown of the most promising options:
🧬 1. Targeted Therapies
These drugs specifically attack cancer cells based on genetic or molecular features, sparing normal cells and therefore reducing many typical side effects.
Examples:
- HER2‑targeted drugs (for HER2‑positive cancers)
- CDK4/6 inhibitors (for hormone receptor–positive cancers)
- PI3K and AKT inhibitors
Benefits:
✔ More precise action
✔ Fewer effects on healthy cells than standard chemo
✔ Often oral medications or shorter infusion times
Common side effects: fatigue, mild GI symptoms, manageable lab abnormalities.
🧪 2. Immunotherapy
This uses the patient’s own immune system to recognize and attack cancer cells.
- Checkpoint inhibitors are the main class used in breast cancer so far.
Benefits:
✔ Durable responses in certain patients
✔ Often less damaging to normal tissues
✔ Side effects usually immune‑related (colitis, skin rash, thyroid changes) — often manageable
Immunotherapy isn’t right for every subtype but is showing strong results in selected groups.
💉 3. Antibody‑Drug Conjugates (ADCs)
These are hybrid therapies: they use an antibody to deliver potent cancer drugs directly to tumor cells, sparing healthy tissue.
Benefits:
✔ Highly targeted
✔ Less systemic toxicity than standard chemotherapy
✔ Often effective in resistant or advanced disease
Side effects are generally milder and more predictable than conventional chemo.
⚛️ 4. Proton Therapy (Advanced Radiation)
Unlike traditional X‑ray radiation, proton therapy deposits most of its energy directly in the tumor and spares surrounding tissue.
Benefits:
✔ Reduced damage to heart, lungs, and skin
✔ Lower risk of long‑term radiation side effects
✔ Fewer acute side effects like skin irritation
This is especially helpful for left‑sided breast cancers or young patients where long‑term toxicity matters.
🧬 5. Genomic‑Guided Therapy
Tests like Oncotype DX and others help predict who will benefit from chemotherapy and who won’t.
Benefits:
✔ Many patients can avoid chemotherapy entirely
✔ Lower treatment burden and fewer side effects
✔ Treatment is individualized
This approach is standard for many hormone receptor–positive breast cancers.
🧠 6. Less Toxic Chemotherapy Scheduling
New dosing strategies such as:
- Metronomic chemotherapy (lower, more frequent doses)
- Shorter infusion cycles
These reduce common toxicities like nausea, fatigue, and immune suppression.
🩹 7. Supportive Care Advances
Even when traditional treatments are needed, better management of side effects has revolutionized care:
- Improved anti‑nausea drugs
- Growth factors to protect bone marrow
- Medications to reduce neuropathy and mucositis
- Personalized supportive regimens
These don’t change the cancer therapy itself but make treatment much more tolerable.
Why These Approaches Matter
Traditional chemotherapy and broad‑field radiation can be effective — but they often cause side effects because they affect healthy cells too.
Newer approaches focus on:
✔ Precision — targeting specific cancer mechanisms
✔ Immune engagement — letting the body fight cancer
✔ Reduced collateral damage to healthy tissue
Together, these mean less fatigue, fewer long‑term toxicities, and better quality of life during and after treatment.
Final Takeaway
Yes — there are newer breast cancer treatments now in widespread use or advanced stages of adoption that offer:
- More targeted action
- Fewer side effects
- Better preservation of quality of life
- Personalized treatment decisions
This doesn’t mean side effects are eliminated, but they are often significantly reduced and more manageable than with older approaches.
11. What role does $NF1$ mutation play in immunotherapy response?
Answer: AI-driven genomic analysis in 2026 has highlighted that $NF1$ mutations can actually improve a patient’s response to immunotherapy in cancers like lung cancer. This finding is critical as it helps oncologists select the optimal, highly personalized therapy from the start. This AI-driven insight is a great example of the New methods in Cancer treatment in 2026.
12. Where can I find more information on pediatric cancer advances in 2026?
Answer:
Here’s the same information with all sources removed, written clearly and simply:
Where to Find Information on Pediatric Cancer Advances in 2026
If you want to stay up-to-date on the latest breakthroughs, here are the main resources:
1. Major Research Reports
- Organizations in pediatric oncology release annual or biannual progress reports summarizing new therapies, immunotherapy, precision medicine, genetic insights, and survivorship advances.
- These reports provide a clear overview of current treatment trends and emerging therapies.
2. Scientific Journals
- Peer-reviewed journals regularly publish studies on pediatric oncology, including tumor biology, new therapies, survivorship, and treatment strategies.
- Journals often have special issues focused specifically on pediatric cancer and innovations in treatment.
3. Conferences and Scientific Meetings
- Annual pediatric cancer conferences present cutting-edge research, clinical trial results, and expert debates.
- Attending these conferences, either in-person or virtually, gives access to the latest studies and treatment strategies.
4. Clinical Trial Registries
- Worldwide registries allow you to search for active pediatric cancer trials by tumor type, age group, therapy type, and phase.
- This is the best way to see which new treatments are currently being tested.
5. Professional Organizations
- Pediatric cancer foundations and oncology groups publish updates, guidelines, and progress reports.
- They often fund research and provide newsletters with the latest scientific and clinical information.
6. Academic Preprint Archives
- Early research papers are available before formal publication.
- These often include studies on tumor biology, new therapies, and innovative treatment models.
7. Government & Public Health Initiatives
- National programs and research initiatives may release updates on new pediatric oncology studies and investments in advanced therapies.
8. Health & Science News Coverage
- Reputable health news sources summarize major breakthroughs and new treatments, often following the release of important studies or clinical trial results.
Tips to Stay Updated
- Set alerts on research databases for “pediatric cancer 2026”
- Follow journals and professional organizations in pediatric oncology
- Subscribe to newsletters from cancer research foundations
- Monitor clinical trial registries for the newest studies
The Road Ahead: Hope and Access
The convergence of powerful cellular engineering, refined molecular targeting, and transformative computational tools defines the New methods in Cancer treatment . The overall message is one of immense hope: cancer is increasingly becoming a manageable, and in many cases, curable disease. Our ability to offer targeted, less toxic therapies means a better quality of life and higher survival rates for patients globally.
However, access to these cutting-edge treatments remains a challenge. Many of the most advanced protocols and clinical trials are centered in major medical tourism destinations. Exploring your options and understanding the regulatory landscape is paramount. You can find comprehensive guides on topics ranging from lung cancer treatment in Iran to advanced neuro-oncology right here.
We are dedicated to connecting patients with the most effective, safest, and most personalized care available anywhere in the world. If you or a loved one are exploring the next steps in your treatment journey, remember that the latest breakthroughs can offer a path forward where older methods could not.
Ready to explore advanced, personalized cancer treatment options available globally?