👂 Otoplasty: Your Complete Guide to Ear Pinning and Reshaping
Executive Summary: Key Takeaways
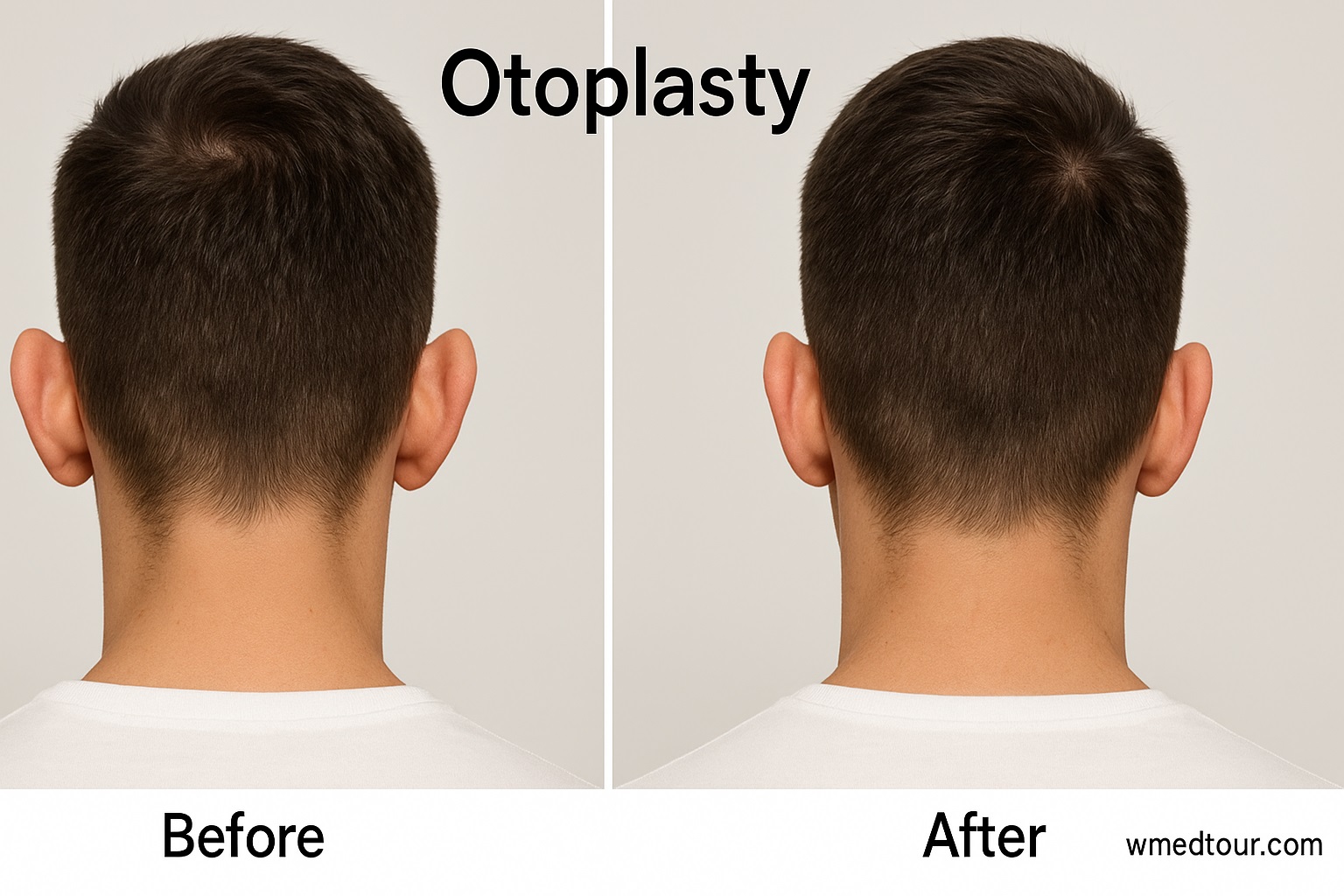
Otoplasty, commonly known as ear pinning or ear reshaping, is a highly effective surgical procedure that corrects prominent, large, or misshapen ears. This surgery offers profound **psychological and social benefits**, particularly for children and adolescents, by significantly improving self-esteem. As a matter of fact, it represents one of the most frequently performed cosmetic procedures for young people. This comprehensive guide details the essential aspects of Otoplasty, including the different techniques surgeons use (Sutures vs. Cartilage Alteration), the ideal candidate, the recovery process, associated costs, and steps for choosing an experienced surgeon. Understandably, you should always consider any surgical procedure carefully; consequently, we break down the pros and cons and offer a detailed patient journey to help inform your decision. If you seek to understand the full scope of Otoplasty, you will certainly find everything you need here.
🔍 What is Otoplasty?
The term Otoplasty describes a range of surgical and non-surgical procedures designed to change the shape, position, or size of the ears. Most often, the procedure addresses “protruding ears”—ears that stick out significantly from the side of the head. Furthermore, the primary goal involves creating a natural, aesthetically pleasing appearance that complements the other facial features. Typically, a plastic surgeon or an Otolaryngologist (ENT specialist) performs this surgery. To illustrate, Otoplasty can correct congenital defects, trauma-related damage, or simply a cosmetic concern about ear prominence. Essentially, the procedure requires customization of the ear’s cartilage structure.
While surgeons often perform the procedure on children (usually after age five when ear cartilage is stable), adults also seek Otoplasty to finally address lifelong self-consciousness. Choosing the right specialist for this delicate procedure remains paramount, particularly if you consider cosmetic surgery abroad. Therefore, research thoroughly before proceeding.
👤 Who is This For?
This procedure isn’t universally required; rather, it suits specific groups best. In general, the ideal candidate meets the following criteria:
**Children (Ages 5 and Up):** Since ear development largely completes by age five or six, this represents the prime time for correction. Importantly, early intervention can prevent school-age teasing and **emotional distress**.
**Adolescents and Adults:** Anyone bothered by the appearance of their ears who maintains good general health qualifies. They must also hold realistic expectations about the outcome.
**Individuals with Protruding Ears:** The most common reason for Otoplasty involves correcting ears that project too far from the head (more than 2 cm).
**People with Ear Deformities:** This includes conditions like ‘Lop Ear’ (tip folds forward and down), ‘Shell Ear’ (lacks the natural folds and creases), or ears that are too large (Macrotia). **Thus**, the procedure offers solutions for various issues.
Conversely, non-candidates may include individuals with active ear infections or those with unrealistic expectations. Therefore, a thorough consultation with a surgeon always constitutes the first step.
🛠️ Otoplasty Techniques: Sutures vs. Cartilage Alteration
The surgeon selects the technique based on the patient’s specific anatomy and the desired result. Generally speaking, the approaches fall into two distinct categories:
1. Suture-Only Techniques (The Mustarde or Furnas Method)
Surgeons often classify these techniques as minimally invasive. Specifically, they use permanent internal sutures to reshape the ear cartilage without needing to cut or remove any tissue. Surgeons often utilize these techniques to create or enhance the antihelical fold, which is missing or underdeveloped in protruding ears. **Consequently**, this method proves very popular.
Significantly, patients often experience quicker recovery with less potential for bruising. For example, the Mustarde technique involves placing sutures to flatten the prominent conchal bowl (the deep hollow near the ear canal). In fact, many modern surgeons favor this approach because of its precision and reduced invasiveness. **Moreover**, the results are highly reliable.
2. Cartilage Alteration/Excision Techniques
In cases where the cartilage proves too firm or the protrusion is severe, the surgeon may need to score, cut, or remove cartilage. Consequently, this method allows for a more dramatic change in shape and position. The surgeon typically places the incision in the crease behind the ear (postauricular sulcus), thus making the resulting scar nearly invisible. For instance, when treating Macrotia (oversized ears), the surgeon excises a crescent-shaped piece of cartilage and skin. **Therefore**, this technique provides a powerful solution for complex cases.
Furthermore, an excellent example of a combined approach involves the use of the anterior scoring technique (cartilage alteration) along with Mustarde sutures (suture-only) to achieve a multi-faceted correction. Learning about these different face and neck procedures is vital when planning your medical journey.
👍👎 Pros and Cons of Otoplasty
Like any surgical procedure, Otoplasty comes with a distinct set of benefits and potential drawbacks. You must maintain a balanced view before you move forward. Therefore, we present a clear breakdown:
| ✅ Advantages (Pros) | ❌ Disadvantages (Cons) |
|---|---|
| Permanent Results: The results are typically lifelong once surgeons reshape the ears. | Surgical Risks: Risks include general anesthesia risks, bleeding, infection, and adverse reactions. |
| Significant Psychological Boost: Vastly improves self-esteem and reduces anxiety, especially in children facing bullying. | Potential Asymmetry: Although rare, minor differences between the two ears can persist or occur post-surgery. |
| Hidden Scars: Surgeons almost always place the incisions behind the ear, which makes scars virtually undetectable. | Recurrence/Correction Failure: In some cases, the ears may slowly revert to their original position, requiring revision surgery. |
| Relatively Quick Recovery: Most patients return to non-strenuous activities within a week. **Generally**, this speed minimizes disruption. | Temporary Discomfort: Patients commonly experience swelling, bruising, and mild to moderate pain in the first few days. |
| Correction of Deformities: The procedure can fix complex congenital or traumatic ear deformities. | Numbness or Tingling: Changes in ear sensation are possible, though often temporary, due to nerve manipulation. |
🗺️ The Otoplasty Patient Journey: A Case Study
To better illustrate the process, let’s walk through a hypothetical patient’s experience. This case study will help you visualize the steps from initial consultation to full recovery. **Hence**, pay close attention to the timeline.
Case Study: Amelia’s Journey (Age 8)
**Initial Concern:** Amelia’s parents noticed her ears were becoming a source of distress; consequently, she started wearing her hair down constantly and was the subject of teasing at school. Her ears protruded about 2.5 cm from her head.
**Consultation:** The surgeon, after examining Amelia and discussing her and her parents’ goals, confirmed her as an excellent candidate for Otoplasty. Because Amelia’s primary issue was a lack of the antihelical fold, the surgeon recommended a modified Mustarde technique using permanent internal sutures. They scheduled the surgery for her school’s summer break. **Therefore**, timing worked perfectly.
**Pre-Op and Surgery:** Amelia underwent a standard pre-op checkup, including blood tests, and stopped taking certain supplements. The surgery itself took approximately 90 minutes under general anesthesia. The surgeon made an incision in the crease behind her ear, placed the sutures to reshape the cartilage, and closed the incisions. She woke up wearing a bulky head dressing.
**Recovery (Weeks 1-6):**
**Day 1-7:** Amelia experienced mild pain, which prescribed medication managed effectively. She wore the bulky dressing for the first 5 days. After removal, her ears looked swollen, but the improvement was instantly noticeable. She had to wear a soft headband constantly to protect the ears and maintain their new shape. Her parents ensured she avoided activities that could injure her ears. Similar recovery care and timelines apply to many other head procedures. **In essence**, diligent care was necessary.
**Week 2-6:** Swelling gradually subsided. She only required the protective headband at night or during sports. She returned to school after two weeks and felt significantly happier, reporting no further teasing. **Finally**, her confidence returned.
**Outcome:** By the three-month mark, Amelia’s ears were fully healed, sitting naturally closer to her head. Her self-confidence soared, clearly demonstrating the powerful **mental well-being** impact of a successful Otoplasty.
This path showcases how a smooth patient journey, careful planning (especially regarding the timing of surgery), and adherence to post-operative instructions lead directly to a positive result. This kind of success is what you should look for when vetting potential specialists. You might want to refer to a comprehensive checklist when choosing a surgeon or clinic abroad. **Ultimately**, preparation ensures safety.
🩹 Recovery and Aftercare: Ensuring the Best Results
The post-operative phase is arguably as crucial as the surgery itself. In order to guarantee the ears heal in their new position, you must adhere strictly to the surgeon’s guidelines. Crucially, you will have the initial dressing removed after a few days, revealing the new ear contour, which will still show some swelling. **Immediately** after removal, you must begin wearing the protective band.
Key Recovery Steps:
**Protective Headband:** You must wear a compression headband or ear band consistently for the first week, and then only at night for several more weeks. This measure prevents accidental trauma and helps the ears maintain their shape. Failure to wear this is a common reason for recurrence, so be diligent. Wearing protective gear is crucial in many post-surgical scenarios. **Furthermore**, it safeguards the delicate structures.
**Sleeping Position:** Absolutely avoid sleeping on the sides. Instead, use several pillows to keep your head elevated and sleep on your back to prevent pressure on the ears. **Otherwise**, you risk displacing the cartilage.
**Activity Restriction:** Avoid strenuous exercise, heavy lifting, and contact sports for at least six to eight weeks. Basically, you must restrict anything that could cause a direct blow to the ear. **In fact**, light walking is the only recommended activity initially.
**Medication:** The surgeon will prescribe pain medication and antibiotics to prevent infection. You must use them exactly as directed. Importantly, avoid aspirin and other blood-thinners unless your doctor advises otherwise. **Thus**, you manage both pain and infection risk effectively.
Generally, most patients feel comfortable enough to return to work or school within 5 to 7 days, even though some residual swelling may persist for several weeks. Surgeons usually see the final result of the Otoplasty after about six months, once all swelling has completely resolved. **Therefore**, patience during recovery is key.
💰 Otoplasty Cost Comparison: Global Perspective
The cost of Otoplasty varies dramatically depending on the surgical technique, the surgeon’s experience, the clinic’s location, and whether the surgery involves both ears (bilateral) or one ear (unilateral). Consequently, many international patients choose countries like Turkey or Iran, finding highly affordable, yet high-quality, cosmetic procedures there.
| Location | Average Price Range (USD) | Notes |
|---|---|---|
| United Arab Emirates (Dubai) | $4,500 – $8,000+ | High-end, luxurious facilities, premium pricing. **However**, quality remains excellent. |
| Turkey | $2,000 – $4,500 | Extremely popular for medical tourism; high volume, competitive pricing. **Indeed**, it’s a global hub. |
| United States/Western Europe | $5,000 – $9,500+ | Highest cost, but often includes comprehensive follow-up care. |
| Iran | $1,500 – $3,000 | Very affordable with specialized surgical expertise, often combined with travel packages. |
| India | $2,500 – $4,000 | Competitive pricing and experienced surgeons, especially in large metropolitan areas. |
Ultimately, a lower price shouldn’t be the only determining factor. Instead, you must prioritize quality and surgeon reputation. Before making a decision, research the surgeon’s qualifications and the facility’s accreditation, as outlined in guides like Global Medical Treatment Regulations Guide. **Therefore**, always perform due diligence.
👨⚕️ Choosing Your Otoplasty Surgeon
Selecting the right surgeon is absolutely critical for achieving a successful outcome. Because ear shape is complex and highly individualized, the surgeon needs an artistic eye combined with technical skill. Here are essential factors to consider:
Certification and Expertise
Look for a surgeon who holds board-certification in plastic surgery or Otolaryngology-Head and Neck Surgery. Consequently, this certification ensures they have met rigorous training and ethical standards. Specifically, ask how many Otoplasty procedures they perform annually. A high-volume surgeon typically possesses more refined techniques. **However**, also check patient reviews.
Before & After Photos
Always review the surgeon’s portfolio of previous Otoplasty cases. Look for results that appear natural and symmetrical. If you look for specialists, our directory can help you vet qualified doctors.
Facility Accreditation
Confirm that the surgery will take place in an accredited hospital or surgical center. For instance, reputable centers adhere to strict safety protocols, reducing the risk of complications. **Moreover**, accreditation provides peace of mind.
It’s important to remember that clear communication is key. The surgeon should listen attentively to your aesthetic goals and clearly explain the limitations and potential risks of the procedure. For more on this, consider reading our advice on vetting surgeons, which applies across all surgical specialties. **Finally**, ensure you feel comfortable with the professional.
🧠 The Profound Mental Well-being Impact of Ear Surgery
The most significant, and often underestimated, benefit of Otoplasty is the **psychological** transformation it brings. Protruding ears can lead to serious self-consciousness, social anxiety, and, especially in children, become a target for bullying. Research consistently shows that ear pinning can dramatically improve a patient’s quality of life. The Journal of Craniofacial Surgery confirms that patients report higher levels of self-satisfaction and reduced social inhibition following the procedure. Correspondingly, this benefit explains why many parents choose to have the surgery done before their child starts school. **Indeed**, preventing long-term emotional damage is paramount.
Because the ears are almost fully grown early in life, correcting them at a young age allows children to develop a positive self-image before long-term emotional scars set in. Therefore, this empathetic approach to cosmetic surgery—improving **mental well-being**—remains central to the practice. Further research from Cureus Journal highlights that the procedure is highly effective in achieving patient satisfaction for aesthetic concerns. Furthermore, the emotional relief this provides often far outweighs the physical change. **Ultimately**, the procedure changes lives.
🚀 Emerging Trends in Otoplasty
While traditional Otoplasty remains the gold standard, new techniques are constantly emerging to improve results and minimize invasiveness. Consequently, the procedure becomes safer and more accessible. **For example**, consider these alternatives:
Non-Surgical and Minimally Invasive Options
For newborns with ear deformities, a non-surgical method called **ear molding** can be highly effective. Because the cartilage remains very soft due to maternal estrogens, surgeons can reshape the ears using specialized splints, thereby avoiding surgery entirely. However, practitioners must initiate this within the first few weeks of life to achieve success. **Otherwise**, the window of opportunity closes quickly.
Another emerging method for adults is the **Earfold** system, a minimally invasive alternative that involves implanting a small clip under the skin to hold the ear cartilage in the desired position. This offers a quicker, local-anesthesia option, although experts still evaluate its longevity compared to traditional surgery. This innovation illustrates how the field of plastic surgery is always advancing. Likewise, you can see similar advances in areas like new methods in fat removal or AI-driven medical precision. **In summary**, the options expand constantly.
A recent study from JAMA Otolaryngology–Head & Neck Surgery indicates high long-term satisfaction and low complication rates for traditional techniques, thus validating their continued use in most cases. **Significantly**, the safety profile is strong.
🛑 Risks and Potential Complications
While surgeons generally consider Otoplasty a safe procedure, you must remember it involves surgery, and risks exist. Being fully aware of these complications helps you make an informed decision. **Therefore**, review the list below carefully:
**Infection:** Rare, but possible. Doctors typically treat this with antibiotics. **Specifically**, look for redness or pus.
**Hematoma:** This is a collection of blood under the skin. It can sometimes require drainage by the surgeon. **If it occurs**, contact your clinic immediately.
**Suture Extrusion:** The internal sutures can sometimes surface through the skin, requiring removal or replacement. This is more common with non-dissolvable materials. **Consequently**, some surgeons prefer newer materials.
**Unsatisfactory Results:** This includes asymmetry, over-correction (ears pinned too flat), or under-correction (recurrence). Revision surgery may be necessary in about 5-10% of cases. Consulting with a specialist is the best way to mitigate these risks. For more on managing unexpected surgical results, see our guide on revisions for failed procedures. **Despite the low risk**, be prepared for this possibility.
**Keloid/Hypertrophic Scars:** Raised scars, though rare since the surgeon places the incision behind the ear. Individuals with a predisposition to keloids must inform their surgeon beforehand. **Likewise**, disclose all relevant medical history.
To reduce these risks, ensure you follow all pre-operative instructions precisely, particularly those concerning smoking cessation and medication avoidance. The Mayo Clinic provides clear guidance on these general surgical precautions. Additionally, proper wound care minimizes the chance of infection. **Ultimately**, your compliance determines much of the success.
✈️ Important Considerations for Medical Tourism
Patients increasingly travel for Otoplasty, drawn by cost savings and the high expertise available in global hubs like Turkey, Iran, and India. However, going abroad demands additional planning and due diligence. For instance, you should consider the total cost, including flights and accommodation, against the price of surgery alone. **Moreover**, factor in currency fluctuations.
**Post-operative Stay:** Crucially, you must plan to stay in the destination country for at least 7-10 days for your initial follow-up appointment and removal of the main dressing. This ensures the operating surgeon can manage any immediate complication. **Therefore**, never rush your departure.
**Communication:** Ensure the surgeon and clinical staff communicate effectively in your native language or that a reliable medical translator is available. This prevents misunderstandings, particularly regarding critical aftercare instructions. **Indeed**, clear instructions prevent errors.
**Accreditation:** Look for international accreditations such as JCI (Joint Commission International). You can learn more about international accreditation and its importance in our Pre-Travel Resources and Checklists. **Hence**, prioritize accredited facilities.
Ultimately, a successful medical trip depends on meticulous planning. While the cost of aesthetic surgeries in Turkey or Rhinoplasty prices in Iran often drive the initial decision, safety and quality should always remain the priority. MedlinePlus stresses the importance of understanding the entire scope of the procedure and recovery. **Thus**, you travel with confidence.
✨ Non-Surgical Otoplasty: Is it an Option?
While most adult corrections require surgery, a few non-surgical avenues exist, primarily for infants. **Specifically**, consider the early intervention methods.
Infant Ear Molding (Splinting)
As mentioned, this technique is incredibly successful when started early. Within the first 6-8 weeks of life, a soft, custom-made splint is worn to gradually reshape the malleable cartilage. **Therefore**, organizations like Healthy Children (AAP) highly recommend this as a first line of defense against future Otoplasty needs. The key is timing: the window closes quickly as the baby’s estrogen levels drop. **Consequently**, parents must act quickly.
Fillers and Sutures (Temporary Fixes)
Occasionally, surgeons use injectable fillers to build up deficient parts of the ear or temporarily pin back the helix with a non-permanent suture. However, these methods are not a substitute for permanent surgical Otoplasty, which addresses the underlying cartilage structure. Consequently, they offer only temporary relief. **In contrast**, surgery provides permanent results.
For other aesthetic non-surgical options, you might be interested in treatments like CO2 Laser Skin Resurfacing or Skin Tightening Procedures. **Additionally**, explore options for hair loss.
❓ Frequently Asked Questions (FAQ) About Otoplasty
We compile answers to the most common questions our patients have regarding Otoplasty. **Specifically**, we cover topics not addressed above:
Can Otoplasty Improve Hearing?
No, Otoplasty is a cosmetic and reconstructive procedure that focuses solely on the shape and position of the outer ear (pinna). It does not affect the middle or inner ear structures; therefore, it will not improve or worsen your hearing. If you are concerned about hearing, consult an ENT specialist immediately.
Is Otoplasty covered by insurance?
In most cases, Otoplasty is considered a cosmetic procedure, so health insurance does not cover it. However, if the surgeon performs the surgery for reconstructive reasons (e.g., following trauma or to correct a significant congenital abnormality like Microtia) or if a doctor deems it medically necessary to address significant **emotional distress**, coverage may be possible. Always check with your insurance provider directly; **furthermore**, ask for pre-authorization.
How long do the results of Otoplasty last?
Surgeons consider the results of surgical Otoplasty permanent. Once the cartilage is successfully reshaped and healed, the ears will maintain their new position for life. There is a small risk of partial recurrence (the ear moving slightly back toward its original position), which is why strict adherence to post-operative headwear is essential. **Otherwise**, recurrence becomes more likely.
What type of anesthesia is used for Otoplasty?
For children, surgeons almost always use general anesthesia to ensure they remain still and comfortable throughout the procedure. For adults, Otoplasty can often be performed under local anesthesia with sedation, meaning the patient is awake but completely relaxed and the surgical area is numb. **Thus**, the procedure suits many patient preferences.
How soon after the procedure can I wash my hair?
You should avoid washing your hair for the first few days while the initial surgical dressing remains in place. After the surgeon removes the dressing (usually around day 5-7), you can gently wash your hair, taking great care not to bend or rub the ears. Use mild shampoo and lukewarm water; furthermore, have someone help you initially. **Consequently**, cleanliness is maintained safely.
Will I need to miss work or school?
Most adults can return to desk work or light activity within 5 to 7 days. Children typically need about a week off school. The key consideration is the visibility of the protective headband, which you may need to wear full-time for the first week. **In short**, plan for about one week away.
Are there any age limits for Otoplasty?
The procedure can be performed safely on children as young as four or five, since the ears are almost fully developed by then. There is no upper age limit, provided the patient is in good overall health. **Therefore**, age rarely prevents the procedure.
How visible are the scars after Otoplasty?
Scars are very well concealed, as the surgeon almost exclusively makes the incision in the natural crease (sulcus) behind the ear. Over time, these scars typically fade to thin, fine lines that become virtually unnoticeable. **Indeed**, scar visibility is minimal.
Can non-protruding ears be reshaped (e.g., for size reduction)?
Yes, Otoplasty encompasses more than just pinning. Surgeons can perform techniques like Macrotia reduction to reduce the size of overly large ears. However, ear size reduction surgery is technically more complex than simple ear pinning. **Nevertheless**, a skilled surgeon can address it.
What should I look out for during the recovery process?
Contact your surgeon immediately if you notice severe, sudden pain, excessive bleeding, high fever, or any foul-smelling discharge from the incision sites. These could be signs of an infection or hematoma, which require immediate medical attention. **Furthermore**, swelling that increases after the first three days is a concern.
Can Otoplasty correct ears damaged by piercings or stretching?
Yes, specialized reconstructive Otoplasty (often called **earlobe repair**) can address tears from heavy earrings or correct stretched earlobes from gauges. This is usually a simpler, in-office procedure, often performed under local anesthesia. **Additionally**, earlobe reconstruction is common.
Does the surgeon remove any cartilage during Otoplasty?
It depends on the technique used. Suture-only methods only use stitches to reshape the cartilage. Conversely, for more severe protrusion or overly prominent cartilage (conchal hypertrophy), the surgeon may carefully trim away a small amount of cartilage to achieve the desired contour and position. **Therefore**, the approach depends on the patient’s anatomy.
🌟 Final Thoughts and Next Steps
Otoplasty is a straightforward procedure with a high satisfaction rate, offering dramatic cosmetic and, more importantly, **emotional** benefits. By now, you’ve learned about the techniques, the recovery process, and the critical importance of selecting a qualified surgeon. Whether you choose to have the procedure locally or as part of global medical tourism, you must prioritize expertise and clear communication. If you explore the option of having face surgery, including Otoplasty, abroad, remember to start with a comprehensive consultation to outline your expectations and confirm your candidacy. **Consequently**, you maximize your chances for success.
Ready to explore your options or consult with a top-tier Otoplasty specialist? Contact us today to begin your journey toward greater confidence.