🎗️ Pediatric Cancer Early Signs 2026: A Parent’s Guide
📋 Executive Summary
Early detection remains the most critical factor in surviving childhood cancer. This guide provides an exhaustive look at the symptoms that often mimic common childhood illnesses. Consequently, parents must stay vigilant. Key takeaways include:
- Understanding that persistent symptoms are more concerning than acute ones.
- Recognizing the ‘CHEEKY’ acronym for early warning signs.
- Navigating the diagnostic journey from initial concern to expert care.
- Exploring global treatment options through medical tourism.
👨👩👧👦 Who is This For?
This guide serves as a vital resource for parents, guardians, and primary caregivers. Additionally, educators and pediatric healthcare professionals will find the localized 2026 data beneficial. If you are noticing unusual changes in a child’s health, this article provides the authoritative clarity you need. We prioritize empathy while delivering high-level medical insights.
🚨 Understanding Pediatric Cancer Early Signs 2026
Pediatric cancer is rare. Nevertheless, it affects thousands of families globally every year. In 2026, diagnostic tools have improved significantly. However, the first line of defense is always the parent. Most childhood cancers have high cure rates if caught early. Therefore, knowing what to look for is your most powerful tool.
Persistent Pain and Lumps
Unexplained pain that lasts for more than a week is a red flag. Specifically, bone pain that wakes a child up at night requires immediate attention. Furthermore, any unusual lump or swelling that does not go away after a few days should be evaluated. These masses are often found in the abdomen, neck, or limbs. While most lumps are benign, professional verification is essential.
Frequently, children get bumps from playing. In contrast, a cancerous mass usually feels firm and fixed. It often grows steadily over time. You should consult the oncology department if a lump appears without an obvious injury. Early imaging can rule out serious conditions quickly.
Energy Changes and Fatigue
Every child has tired days. On the other hand, extreme fatigue that prevents play is abnormal. If a child lacks interest in their favorite activities, investigate further. This lethargy often stems from anemia caused by underlying issues. Moreover, persistent paleness can indicate a struggle within the bone marrow.
Consequently, parents should track energy levels over two weeks. If the fatigue accompanies easy bruising, it is a significant concern. You might consider a pediatric health checkup to establish a baseline. Often, simple blood tests provide the first clues to a diagnosis.
🔍 In-Depth Breakdown: Symptoms by Body System
Neurological Signs (Brain and Spine)
Brain tumors are the most common solid tumors in children. Therefore, neurological symptoms are critical. Morning headaches accompanied by vomiting are classic signs. Similarly, sudden changes in balance or coordination should trigger an urgent visit to the neurosurgery department. Rapidly changing vision or a drooping eyelid are also significant markers.
Vision and Eye Changes
Retinoblastoma is a rare eye cancer. Fortunately, it is often visible. A white glow in the pupil when seen in a flash photograph is a primary sign. Furthermore, a new “crossed eye” or squint can be a symptom. If you notice these, visit the ophthalmology department immediately. Early intervention can save both the child’s sight and life.
📊 Comparison: Common Ailments vs. Early Cancer Signs
| Symptom | Common Illness (Viral/Infection) | Pediatric Cancer Indicator |
|---|---|---|
| Fever | High, clears in 3-5 days. | Low-grade, persistent, or recurring. |
| Lumps | Soft, tender, shrinks within weeks. | Firm, painless, growing steadily. |
| Bruising | Found on shins and elbows from play. | Unexplained, on trunk, back, or face. |
| Headaches | Occasional, related to dehydration. | Early morning, with vomiting, chronic. |
📖 Case Study: Liam’s Journey to Early Detection
In mid-2024, four-year-old Liam began complaining of “tired legs.” Initially, his parents thought they were growing pains. However, the pain persisted at night. Furthermore, Liam developed a slight limp. Rather than waiting, his parents scheduled a comprehensive checkup.
Because they acted quickly, a blood test revealed abnormal cell counts. Liam was referred to pediatric oncology immediately. Consequently, he started treatment for leukemia while the disease was still in its early stages. Today, Liam is in remission, illustrating the power of parent vigilance and rapid medical action.
🛤️ The Patient Roadmap
Navigating a potential diagnosis is overwhelming. Therefore, we have outlined the standard path for families. First, document all symptoms. Second, seek a primary care consultation. Third, if symptoms persist, request specialized molecular diagnostics.
Subsequently, the diagnostic phase may involve imaging such as MRIs or CT scans. You can browse our list of expert doctors to find the right specialist. Once a diagnosis is confirmed, the multidisciplinary team will create a treatment plan. This plan often includes surgery, chemotherapy, or radiotherapy.
💰 Global Cost Analysis Table (Estimates for 2026)
| Service Type | Western Europe/USA | India / Iran / Oman |
|---|---|---|
| Diagnostic Imaging | $2,000 – $5,000 | $300 – $800 |
| Oncology Consultation | $500 – $1,200 | $50 – $150 |
| Chemotherapy (per cycle) | $10,000+ | $1,500 – $3,500 |
🌍 Recovery & Medical Tourism
Many families choose global medical tourism to access high-quality care at a fraction of the cost. Countries like Iran, India, and Oman offer world-class oncology facilities. Furthermore, traveling for treatment allows families to focus entirely on recovery in a supportive environment. Our tours in Iran include full concierge services for medical travelers.
Additionally, we provide air ambulance services for critically ill patients. Safety and comfort are our priorities during transport. We facilitate connections with top-tier hospitals in Oman and India. This ensures your child receives the best possible care without financial ruin.
❓ Frequently Asked Questions
1. Are pediatric cancer early signs 2026 different from previous years?
The biological “red flags” and early physical symptoms of pediatric cancer have not changed in 2026. Because childhood cancers are typically the result of DNA changes that occur early in life rather than lifestyle or environmental factors, the way these diseases manifest in the body remains consistent with previous years.
However, how we identify these signs is evolving. In 2025 and 2026, there has been a significant shift toward earlier detection through “precision surveillance” and new diagnostic tools.
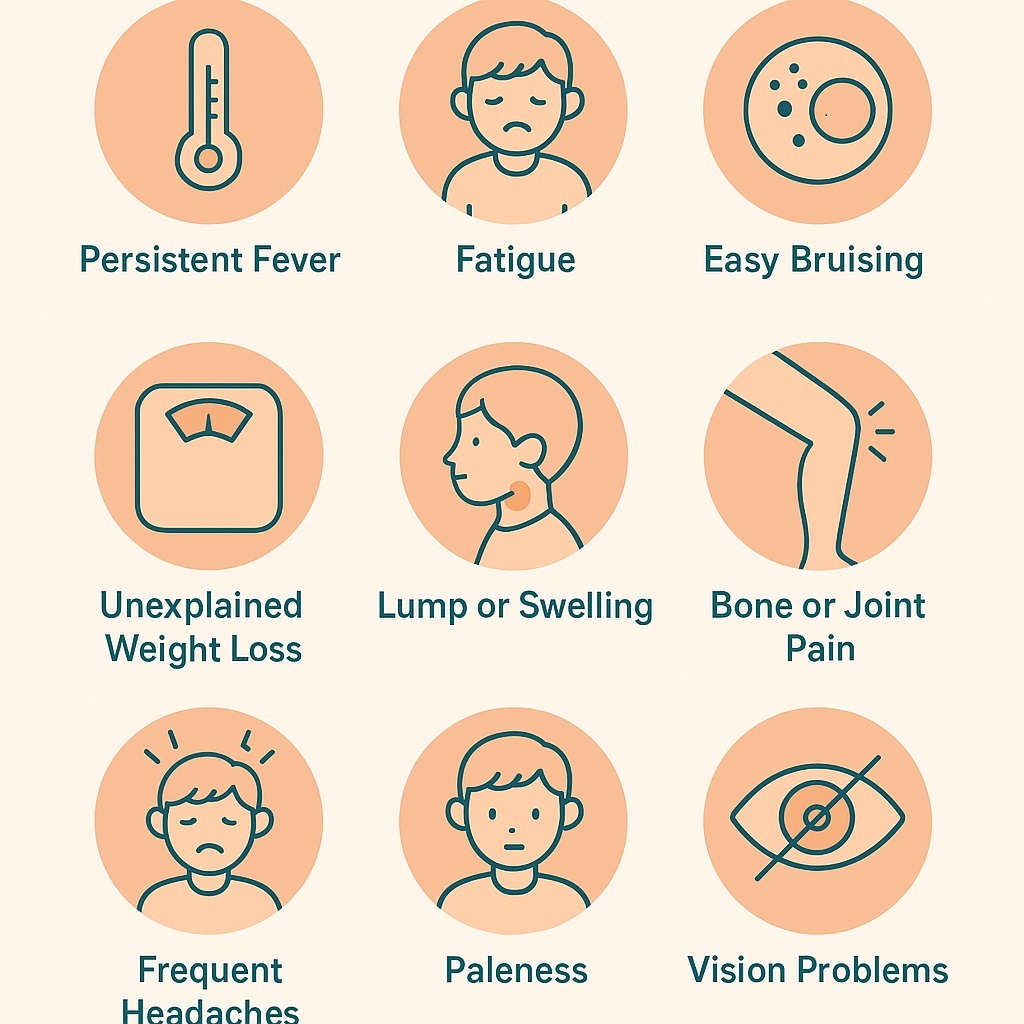
Consistent Early Warning Signs
The “classic” symptoms that parents and doctors look for remain the primary indicators:
Unexplained Lumps or Swelling: Persistent, painless lumps in the neck, abdomen, or limbs.
Vision Changes: A white “glow” in the pupil (leukocoria), a new squint, or sudden vision loss.
Persistent Pain: Bone or joint pain that often worsens at night or causes a limp.
Energy and Color: Unusual paleness (anemia) and extreme fatigue that doesn’t improve with rest.
Unexplained Fevers: Recurrent or persistent fevers not linked to a typical viral infection.
Easy Bruising: Unexplained bruising or small purple/red spots (petechiae) on the skin.
What is Different in 2026?
While the symptoms are the same, the medical approach to them has become more proactive:
Genomic Surveillance: For children with known genetic predispositions (identified through family history or newer screening panels), doctors now use “pre-symptom” monitoring. This involves regular whole-body MRIs and blood tests to catch tumors before physical signs even appear.
Updated Referral Guidelines: Major health organizations (such as the UK’s CCLG “Child Cancer Smart” campaign) have updated their 2025–2026 protocols. These provide GPs with “decision-support tools” to faster distinguish common childhood ailments from “red flag” cancer symptoms, specifically for bone and kidney cancers.
AI-Enhanced Imaging: New AI tools are being integrated into radiology in 2026 to help identify subtle patterns in scans that might have been missed in the past, allowing for diagnosis at a much earlier stage.
Blood-Based “Liquid Biopsies”: While still primarily used in clinical settings, there is an increase in the use of liquid biopsies to monitor for cancer markers in the blood, which can sometimes signal a problem before a physical mass is palpable.
2. Can a blood test detect all childhood cancers?
No, a blood test cannot detect all childhood cancers. While blood tests are a vital part of the diagnostic process, they are generally used to suggest the presence of cancer or monitor its progress, rather than provide a definitive diagnosis for every type.
The role of blood tests varies depending on the type of cancer:
1. Blood Cancers (Leukemia and Lymphoma)
For cancers that originate in the blood or bone marrow, blood tests like a Complete Blood Count (CBC) or a blood smear are often the first step. They can show abnormal levels of white blood cells, red blood cells, or platelets. However, even in these cases, a bone marrow biopsy is usually required to confirm the diagnosis and determine the specific subtype.
2. Solid Tumors (Brain, Bone, and Organ Tumors)
For solid tumors like brain cancer (the second most common childhood cancer), neuroblastoma, or Wilms tumor (kidney cancer), blood tests are often less effective for initial detection.
Brain Tumors: These rarely release markers into the bloodstream that a standard blood test can find. Doctors rely on MRI or CT scans for detection.
Tumor Markers: Some solid tumors release specific proteins or hormones (biomarkers) into the blood, but these are not present for all cancers and are sometimes elevated by non-cancerous conditions.
3. The “Normal Blood Work” Challenge
It is possible for a child to have cancer even if their blood work appears completely normal. In the early stages of many cancers, the disease may not yet have affected the blood cell counts or chemical balance enough to be detected by standard laboratory equipment.
4. The Future: Liquid Biopsies
Research is currently focused on liquid biopsies, which look for “circulating tumor DNA” ($ctDNA$)—tiny fragments of genetic material shed by tumors into the blood. While this technology is promising and could eventually allow for the detection of many more cancers via a simple blood draw, it is currently used mostly in research or for monitoring treatment rather than as a universal screening tool.
Summary of Diagnostic Tools
Since blood tests alone aren’t enough, doctors use a combination of methods:
Imaging: X-rays, Ultrasounds, CT scans, and MRIs.
Biopsies: Taking a physical sample of the tissue or bone marrow.
Physical Exams: Checking for lumps, swelling, or neurological changes.
3. Is a persistent fever always a sign of cancer?
No, a persistent fever is not always a sign of cancer. In fact, it is much more commonly caused by other conditions.
In children, fevers are usually the body’s healthy way of fighting off an “intruder.” While a fever that won’t go away is something doctors take seriously, they look at it as one piece of a much larger puzzle.
1. Common Causes of Persistent Fever
Most fevers that last more than a few days are due to:
Viral Infections: Viruses like Mononucleosis (Mono) or CMV can cause fevers that last for two weeks or more.
Bacterial Infections: Hidden infections like a urinary tract infection (UTI), sinus infection, or even a bone infection (osteomyelitis) can cause a lingering fever.
Autoimmune/Inflammatory Issues: Conditions like Juvenile Idiopathic Arthritis or Kawasaki Disease cause the immune system to overreact, leading to prolonged high temperatures.
Periodic Fever Syndromes: Some children have rare genetic conditions that cause recurring fevers with no clear infection.
2. When Doctors Become Concerned
A fever is rarely the only symptom of childhood cancer. Doctors usually look for “red flags” that occur alongside the fever:
Unexplained Weight Loss: Not just a lack of appetite, but noticeable weight loss.
Night Sweats: Fevers that break at night, leaving the child’s pajamas or bedding drenched in sweat.
Easy Bruising or Bleeding: Small red spots on the skin (petechiae) or bruises in unusual places (like the back or chest).
Bone or Joint Pain: Pain that is deep, persistent, and often wakes the child up at night.
Lumps or Swelling: Firm, painless lumps in the neck, armpit, or groin that don’t go away.
3. Defining “Persistent”
Medical professionals usually categorize fevers into two types:
Prolonged Fever: Lasts more than 8 days.
Fever of Unknown Origin (FUO): Lasts more than 3 weeks without a clear cause after initial tests.
Even in cases of FUO, cancer is statistically the least common cause. The majority of these cases turn out to be unusual presentations of common infections.
Summary: A fever alone is rarely enough to diagnose cancer. If a fever lasts more than a few days, or if your child seems unusually pale, tired, or has new aches and pains, a pediatrician can run simple tests (like a CBC) to help rule out serious issues.
However, a fever lasting more than 14 days without an obvious cause needs an investigation by an oncologist.
4. What does a white glow in the eye mean?
This is often a sign of Retinoblastoma. It is highly treatable if caught early, so please see a specialist immediately.
A white glow in the eye—medically known as leukocoria—is a clinical sign where the pupil (the black center of the eye) reflects a white, yellow, or pale color instead of the typical “red-eye” seen in flash photography.
While it can be alarming, it is not always a sign of something dangerous. Here is a breakdown of what it can mean and what you should look for.
1. Common and Harmless Causes
The most frequent reason for a white glow, especially in photos, is actually harmless:
The Optic Nerve Reflection: If a child (or adult) looks at the camera at a specific angle (usually about 15 degrees), the flash can bounce directly off the optic nerve, which is naturally white. This often appears in only one photo or from one specific angle.
Camera Artifacts: Digital cameras and smartphones sometimes process light in a way that creates a “white eye” effect, especially if red-eye reduction is turned off.
2. Medical Conditions (Non-Cancerous)
If the glow is persistent or appears in multiple photos, it may indicate a treatable eye condition:
Cataracts: A clouding of the lens. This is the most common medical cause of a white reflex in children.
Coats’ Disease: A rare condition where the blood vessels in the retina develop abnormally and leak fluid, causing a yellowish-white reflection.
Retinal Detachment: If the retina pulls away from the back of the eye, it can reflect light differently.
Infections: Certain infections, such as those caused by parasites (like Toxocariasis), can cause inflammation that appears as a white glow.
3. Retinoblastoma (Childhood Eye Cancer)
In young children (usually under age 6), a persistent white glow is the most common early sign of retinoblastoma, a rare form of eye cancer.
Why it glows: The tumor itself is a white mass growing on the retina at the back of the eye. When light hits it, it reflects back through the pupil like a “cat’s eye” caught in headlights.
Urgency: Retinoblastoma is highly curable if caught early, which is why doctors take a “white glow” very seriously.
When to See a Doctor
You should have a child’s eyes checked by a professional (pediatrician or optometrist) if you notice any of the following:
The white glow is present in multiple photos.
The glow is visible to the naked eye in low-light settings (like a dim room).
One eye looks white while the other has the normal red-eye reflection in a photo.
The child has a “squint” (one eye turns in or out) or the eyes don’t seem to look in the same direction.
Simple Home Check: If you saw the glow in a photo, look through your older photos of the child. If you see the same white reflection in only one eye across several different pictures, it is important to schedule an eye exam as soon as possible.
5. Why is night pain significant?
In the context of childhood health, night pain is considered a “red flag” because it behaves differently than the typical aches and pains of childhood.
While most childhood pain (like growing pains or minor injuries) occurs during or after activity and gets better with rest, certain types of pain that wake a child from a deep sleep or worsen when the body is still can indicate an underlying medical issue that requires investigation.
1. Night Pain vs. “Growing Pains”
It is very common for parents to mistake persistent night pain for “growing pains.” However, there are distinct differences:
2. Why is it a “Red Flag” for Cancer?
In rare cases, night pain can be a symptom of bone cancers (like Osteosarcoma or Ewing Sarcoma) or blood cancers (like Leukemia).
Bone Tumors: As a tumor grows, it stretches the “periosteum” (the sensitive outer lining of the bone), which can cause a deep, throbbing ache. This pain often feels worse at night when there are fewer distractions and the body is still.
Leukemia: This cancer starts in the bone marrow. As the marrow becomes crowded with abnormal cells, it can create pressure inside the bones, leading to a “toothache-like” pain in the limbs that may keep a child awake.
3. Other Causes of Night Pain
Cancer is statistically rare. Night pain is more frequently caused by:
Infections: Bone infections (osteomyelitis) can cause deep, persistent pain and fever.
Inflammatory Conditions: Juvenile Arthritis can cause joints to stiffen and ache, especially after being still for a long time (like during sleep).
Benign Tumors: Some non-cancerous bone growths, like an Osteoid Osteoma, are famous for causing pain that occurs specifically at night and is relieved almost instantly by ibuprofen.
4. When to See a Doctor
One night of leg cramps is usually nothing to worry about. However, you should consult a pediatrician if the night pain:
Wakes the child up repeatedly or makes it hard for them to fall asleep.
Is accompanied by swelling, redness, or a visible lump.
Is localized to one specific bone rather than a general muscle ache.
Occurs alongside other symptoms like unexplained fever, weight loss, or limping.
6. Are bruises on the shins a concern?
In most cases, bruises on the shins are not a cause for concern. In fact, the shins are the most common place for active children to have bruises. Because the skin is thin and sits directly over the bone with very little “padding,” even minor bumps from running or playing can break tiny blood vessels and cause a visible bruise.
However, there are specific patterns that might lead a doctor to look more closely.
1. When Shin Bruises are Normal
The “Play” Pattern: Bruises are small, flat, and located on the front of the shin.
The “Healing” Pattern: They change colors (blue/purple to green/yellow) and disappear within 1–2 weeks.
The “Cause” Pattern: You or the child can remember the bump or fall that caused it.
2. When Shin Bruises are a Concern
While the shins are a “safe” spot for bruises, they can become a red flag if they are:
Spontaneous: They appear in large numbers without any known injury or even a minor bump.
Raised or “Lumpy”: Most accidental bruises are flat. Large, swollen, or hard lumps (hematomas) that don’t go away can be a sign of a clotting issue.
Unusually Large: A bruise that is much larger than the injury that caused it (e.g., a massive bruise from a tiny tap).
Persistent: Bruises that stay the same color and don’t begin to fade after two weeks.
3. The “Red Flag” Context
Bruises on the shins are more likely to be checked by a doctor if they appear alongside other symptoms, such as:
Petechiae: Tiny, pinpoint red or purple dots that look like a rash but don’t turn white when you press on them. These indicate bleeding from the smallest blood vessels.
Bruises in “Protected” Areas: If a child has shin bruises plus bruises in soft, fleshy areas like the stomach, back, ears, or the underside of the arms.
Bleeding: Frequent or heavy nosebleeds, or bleeding gums when brushing teeth.
Other Symptoms: Unexplained fever, bone pain, or extreme fatigue.
Summary: If your child has a few bruises on their shins but is otherwise acting normal, playing well, and eating fine, it is almost certainly just the result of being a kid.
7. Does a family history of cancer increase risk?
Yes, a family history of cancer can increase a person’s risk, but it does not mean cancer is inevitable.
Here’s how family history affects risk in simple terms:
Why family history matters
- Some cancers are linked to inherited gene mutations (such as BRCA1/BRCA2 for breast and ovarian cancer).
- If close relatives (parents, siblings, children) had cancer—especially at a young age—your risk may be higher.
- Multiple family members with the same or related cancers can signal a genetic predisposition.
What it does not mean
- Most cancers are not inherited. Lifestyle, environment, and aging play a larger role in the majority of cases.
- Having one relative with cancer does not automatically place you at high risk.
When the risk is more significant
- Cancer diagnosed in relatives before age 50
- Several relatives with the same type of cancer
- Rare cancers or patterns of related cancers in the family
- Cancer occurring across multiple generations
What you can do
- Share your family medical history with a healthcare provider
- Consider genetic counseling if there is a strong family pattern
- Start screening earlier or more frequently if recommended
- Focus on prevention: healthy diet, exercise, avoiding tobacco, and limiting alcohol
Bottom line
A family history of cancer can increase risk, but it’s only one piece of the puzzle. Awareness, preventive care, and early screening can significantly reduce the impact of that risk.
8. How fast do pediatric cancers grow?
Unfortunately, they can grow very quickly. This is why acting on “early signs” within days rather than months is so important.
9. Can stress cause these symptoms?
Stress can cause fatigue or headaches. However, it will not cause lumps, bruising, or localized bone pain.
10. Where can I find the best doctors for treatment?
You can explore our verified doctors list to find specialists in pediatric oncology worldwide.
11. What is the success rate of early detection?
In many cases, the survival rate for childhood cancer exceeds 80% when diagnosed and treated in its early stages.
12. How can I contact your team for assistance?
Please visit our contact us page for a free consultation regarding medical travel and hospital placement.
⚠️ Medical Disclaimer
The information provided in this guide is for educational purposes only. It does not substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. For more details, visit our FAQ section.
© 2026 WMedTour. Supporting families through every step of the journey.
Sources: National Cancer Institute | World Health Organization