👁 Phaco vs. ECCE: When Old School Cataract Surgery is Safer for Complex Cases
ⓘ Executive Summary: Understanding the Safety Trade-Off
Most individuals considering vision correction know Phacoemulsification (Phaco) as the modern, minimally invasive standard for cataract surgery. Conversely, Extracapsular Cataract Extraction (ECCE) is often viewed as outdated. However, this viewpoint is incomplete, particularly in international ophthalmology. Therefore, this article explains why Phaco vs. ECCE is not a simple “new versus old” debate. Instead, it is a nuanced choice based on patient safety.
Indeed, ECCE maintains a critical, life-saving role for specific high-risk patients. These patients primarily have either an extremely dense cataract (a “rock-hard” nucleus) or pre-existing compromised corneal health. Consequently, using Phaco in these scenarios introduces an unacceptable risk of corneal failure due to excessive ultrasonic energy. Thus, a skilled surgeon who can expertly perform both Phaco and ECCE ensures the patient receives the safest, most effective technique, even if it involves a slower recovery. Ultimately, the best choice is the safest choice, and for complex cases, ECCE is safer.
🔬 The Two Surgical Philosophies: Phaco vs. ECCE
Cataract surgery, the world’s most common elective operation, involves replacing the cloudy natural lens with a clear artificial lens. The surgeon’s objective is always clear: achieve excellent vision while minimizing damage to the eye’s delicate internal structures. To achieve this, patients are faced with two main approaches. We must compare the modern, high-tech procedure with its time-tested, manual predecessor to understand the full spectrum of care.
Phacoemulsification: The Gold Standard for Routine Cases
Phaco, short for Phacoemulsification, utilizes ultrasound energy to break up the cataract into small fragments. Consequently, these fragments are then suctioned out through a very small incision, typically only 2.2 mm to 3.0 mm. Therefore, the small wound often requires no stitches and heals rapidly. Furthermore, this minimizes post-operative recovery time and induced astigmatism, making it highly desirable for standard, soft-to-medium cataracts. Nevertheless, its dependence on powerful ultrasonic energy is the source of its primary risk in complicated cases.
Extracapsular Cataract Extraction (ECCE): The Safety Net
ECCE, or Extracapsular Cataract Extraction, is different. The surgeon creates a larger incision, typically 10 mm to 12 mm, and manually removes the entire lens nucleus in one or two pieces. Thus, this method completely bypasses the need for ultrasound within the eye. While the larger wound requires sutures and leads to a slower visual recovery, the inherent safety profile for certain complex eyes is vastly superior. For this reason, experienced ophthalmologists worldwide consider ECCE an indispensable tool, especially when dealing with advanced pathology. Furthermore, understanding the utility of ECCE is essential for any patient seeking comprehensive ophthalmic care, especially when traveling abroad.
Moreover, the key difference between ECCE and ICCE (Intracapsular Cataract Extraction, which is now obsolete) is that both Phaco and ECCE preserve the posterior lens capsule. This delicate, cellophane-like structure is essential because it supports the new intraocular lens (IOL). Conversely, ICCE removed the entire lens-capsule complex, leading to less stable IOL placement and poorer outcomes. Therefore, the focus remains on the controlled, manual removal method of ECCE versus the energetic, fragmentation method of Phaco.
⚠ The Core Conflict: Why Phaco vs. ECCE Safety is Debatable
The central debate in Phaco vs. ECCE hinges entirely on the health of the patient’s eye and the density of the cataract. It is a matter of minimizing collateral damage. Indeed, when a cataract is soft or moderately dense (Grade 1-3), Phaco’s minimal incision and fast recovery make it the safest choice. However, as the cataract hardens, the equation drastically changes. The two primary risks that necessitate the use of ECCE are corneal damage and capsular instability.

The Risk of High Ultrasonic Energy with Hard Cataracts
An extremely dense, brunescent, or “rock-hard” cataract (Grade 4-5) requires the Phaco machine to deliver significant, prolonged ultrasonic energy to fragment the nucleus. Consequently, this high energy generates heat and turbulence inside the eye’s anterior chamber. The most vulnerable structure to this energy is the corneal endothelium.
💀 Understanding Corneal Endothelial Cell Damage
The corneal endothelium is a single, vital layer of cells lining the back surface of the cornea. Crucially, these cells act as pumps, removing fluid from the cornea to keep it clear. Unlike most cells in the body, endothelial cells do not regenerate. Therefore, any loss is permanent. When a dense cataract forces a surgeon to use excessive Phaco energy, the heat and mechanical stress kill a significant number of these cells. As a result, a critical cell count drop can lead to corneal decompensation, causing the cornea to swell and become permanently opaque, requiring a corneal transplant. In contrast, ECCE avoids this complication entirely by removing the hard nucleus whole, without internal ultrasonic energy.
Authoritative research, such as studies published in the Journal of Cataract and Refractive Surgery, routinely supports the finding that high cumulative dissipated energy (CDE) during Phaco is directly correlated with endothelial cell loss (ECL). Thus, in high-grade cataracts, ECCE’s ability to preserve the cornea outweighs Phaco’s faster recovery time. For instance, one study highlighted the significantly lower endothelial cell loss with manual ECCE over Phaco for dense nuclei.
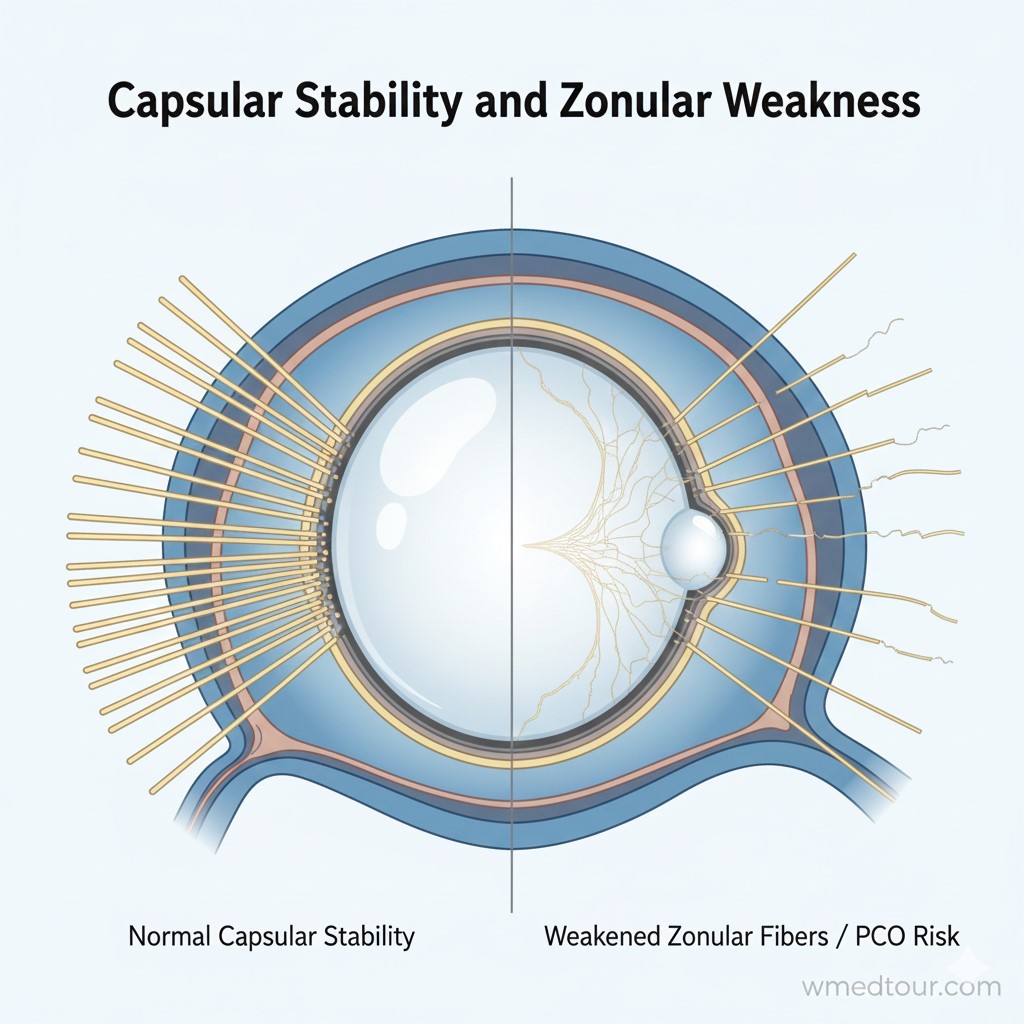
💪 Capsular Stability and Zonular Weakness
The lens is held in place by microscopic fibers called zonules. These fibers can weaken due to trauma, age, or genetic syndromes. Phaco requires the surgeon to manipulate the lens extensively within the capsular bag, putting significant outward stress on these zonules. Conversely, if zonular weakness is present, this manipulation, combined with ultrasonic vibration, can lead to zonular dialysis (tearing) and potential lens subluxation. Consequently, this can lead to the vitreous (the gel inside the eye) prolapsing, which dramatically increases the risk of complications like retinal detachment.
In contrast, ECCE’s larger opening allows for more controlled and direct removal of the lens nucleus. The surgeon can stabilize the lens more effectively and insert the IOL with greater ease, even when the zonules are compromised. Therefore, for eyes with known or suspected zonular weakness, ECCE is often the safer, more manageable procedure, confirming that Phaco vs. ECCE is a debate won by adaptability.
📊 Detailed Breakdown: Pros, Cons, and Comparison
Making an informed decision, especially for medical travelers, requires a clear, objective comparison of the benefits and drawbacks of each method. Therefore, patients must weigh the faster recovery of Phaco against the long-term structural safety offered by ECCE in specific cases. Ultimately, the optimal technique must align with the patient’s ocular health profile.
Phacoemulsification: Key Advantages and Risks
Phaco is widely adopted globally for excellent reasons, as its benefits are significant for the majority of patients.
▲ Pros of Phaco
- Rapid Visual Recovery: Patients often see clearly within a day or two, minimizing disruption to daily life.
- Minimal Astigmatism: The small, self-sealing incision (2.2 mm) induces almost no change to the cornea’s curvature, reducing post-operative focusing issues.
- No Sutures: Avoiding sutures simplifies post-operative care and eliminates the risk of suture-related complications.
▼ Cons of Phaco
- Corneal Endothelial Risk: High ultrasonic energy necessary for dense cataracts can cause irreversible cell loss and corneal decompensation.
- Increased Surgical Complexity in Difficult Cases: Managing complications like capsular tears or zonular weakness through a small incision is significantly harder.
- High Equipment Cost: Reliance on expensive, complex machinery (the phaco machine) increases overhead costs.
Extracapsular Cataract Extraction (ECCE): Key Advantages and Risks
ECCE offers a high margin of safety when a controlled, manual approach is necessary. Consequently, it is a vital option for surgical excellence.
▲ Pros of ECCE
- Corneal Preservation: Uses virtually no ultrasonic energy inside the eye, making it the safest option for patients with hard cataracts or pre-existing corneal disease (like Fuchs’ Dystrophy).
- Superior Control for Complex Lenses: The large incision allows for better visualization and controlled removal of dense, dislocated, or subluxated lenses.
- Manages Capsular/Zonular Tears: Provides ample room to manage vitreous prolapse or securely fixate the IOL if the capsule is compromised.
▼ Cons of ECCE
- Slower Recovery: Healing is slower due to the large, sutured incision; visual stabilization can take several weeks or months.
- Higher Astigmatism Risk: The larger incision can induce greater post-operative astigmatism, requiring careful suture management and removal.
- Longer Operating Time: The manual technique typically requires more surgical time than the automated Phaco procedure.
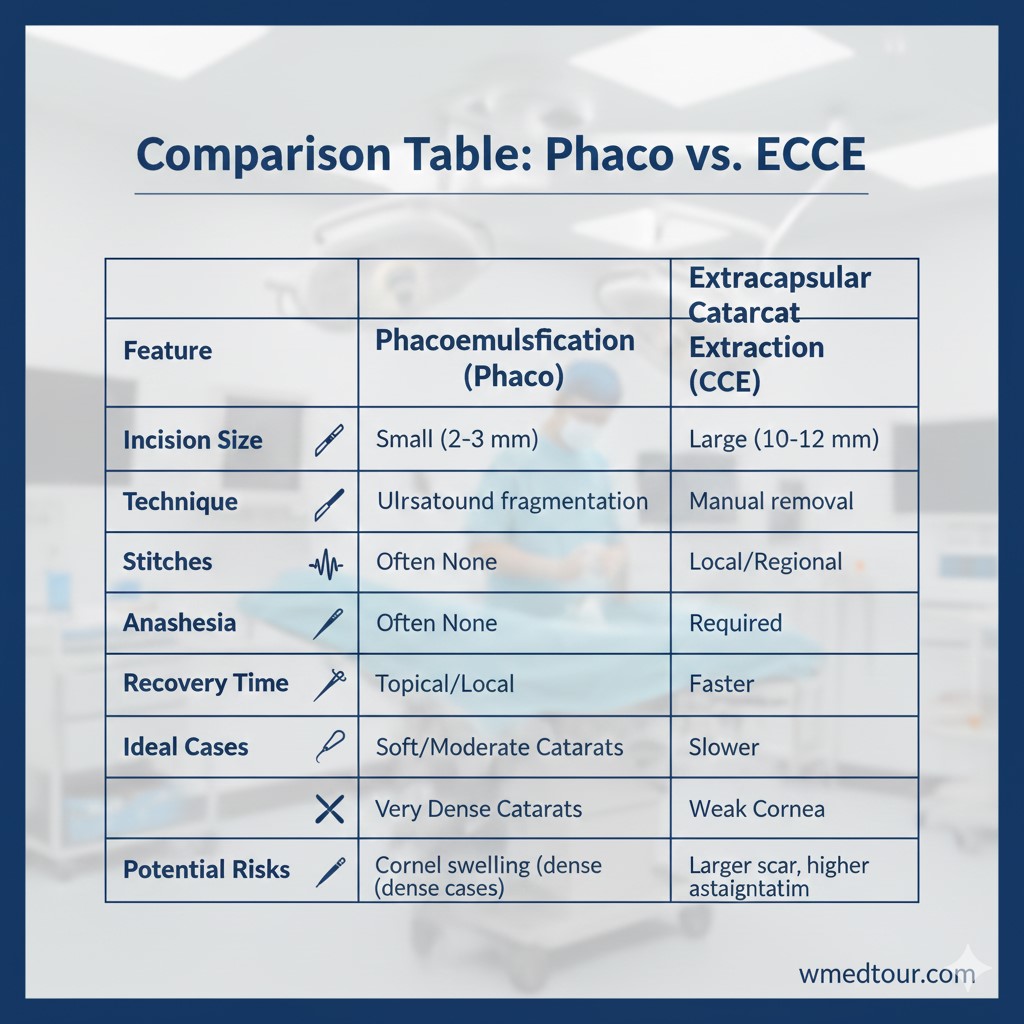
📊 Technique Comparison Table: Phaco vs. ECCE
| Feature | Phacoemulsification (Phaco) | Extracapsular Cataract Extraction (ECCE) |
|---|---|---|
| Incision Size | Small (2.2 mm – 3.0 mm) | Large (10 mm – 12 mm) |
| Energy Use | High ultrasonic energy | Minimal/None (Manual Expression) |
| Recovery Speed | Fast (Days) | Slow (Weeks to Months) |
| Safety for Hard Cataracts | High Risk of Corneal Damage | Safest Option (Protects the Cornea) |
| Sutures Required | Rarely | Always |
| Risk of Conversion | Can require conversion to ECCE | Not applicable (primary manual technique) |
👪 Who is This For? Matching Technique to Patient
The decision for Phaco vs. ECCE should rest squarely on the ophthalmologist’s clinical judgment. Therefore, patients must trust their surgeon to choose the technique that guarantees the best long-term outcome, regardless of the recovery speed. Consequently, high-quality international centers, like the ones we partner with, ensure surgeons are skilled in both methods.
When Phaco is the Optimal Choice
- Soft to Moderate Cataracts: For routine cases classified as Grade 1, 2, or 3, Phaco is undeniably faster and safer.
- Younger Patients: Generally have softer cataracts and excellent corneal health, maximizing Phaco’s recovery benefits.
- Professionals with Time Constraints: Individuals requiring the absolute fastest return to work or travel.
When ECCE is the Safer, Medically Required Choice
- Rock-Hard/Brunescent Cataracts: Grade 4 and 5 nuclei where Phaco energy would destroy the corneal endothelium. For this reason, ECCE is medically mandated.
- Compromised Cornea: Patients with pre-existing conditions like Fuchs’ Dystrophy or very low Endothelial Cell Count (ECC). Phaco is simply too aggressive here. Furthermore, the protection of the cornea must be the priority.
- Subluxated or Dislocated Lenses: When the zonules are weak or broken, the controlled removal offered by ECCE is crucial to prevent vitreous loss and retinal complications.
- Post-Traumatic Cataracts: Often associated with compromised capsules, necessitating the large, controlled access of ECCE.
For patients exploring medical tourism options, it is vital to vet the surgical team. You must ensure they are proficient in both Phaco and ECCE. Indeed, their ability to pivot from one technique to another if complications arise (a ‘Phaco to ECCE conversion’) is a hallmark of an expert surgeon. You can use our checklist for choosing a surgeon to guide your consultation.
🌍 ECCE in Global Ophthalmic Centers
While Phaco dominates routine procedures in Western nations, the mastery of manual techniques like ECCE is a defining characteristic of world-class ophthalmology departments globally, particularly in leading medical tourism destinations. The reason for this dual expertise is simple: complexity demands adaptability. Centres that only offer Phaco risk suboptimal, or even dangerous, outcomes for 10-15% of their cataract patients.
Iran: A Center for Comprehensive Cataract Mastery
Iran, for example, is recognized as a leader in medical tourism in Iran, boasting specialized ophthalmology hospitals with high-volume, experienced surgeons. Therefore, these surgeons routinely manage complex cases, often referred from neighboring countries. They are not only expert in Phaco but maintain high proficiency in ECCE. Consequently, patients can be assured that the safest method will be chosen, not just the trendiest one. This commitment to patient safety is one reason why patients choose destinations with comprehensive departments, which you can explore further in our Ophthalmology Department Guide. Finding a top ophthalmologist in Iran means finding a surgeon proficient in both techniques.
Other International Hubs
Turkey is another significant hub, where medical travel to Turkey offers access to surgeons with equally versatile skills. Similarly, many established centers worldwide, including those detailed in our guide on the top countries for ECCE ophthalmology, continue to value and teach the manual technique. Indeed, the absence of ECCE expertise in a clinic is a sign that they may not be prepared to handle the full spectrum of cataract pathology. This is a crucial consideration when comparing the cost vs. quality, as highlighted in our discussion on cost-vs-quality in medical procedures.
Ultimately, when seeking treatment abroad, patients should prioritize a clinic’s capability to deliver the safest treatment, which in challenging circumstances, means the option of ECCE. This mirrors the care taken in planning for any major procedure, such as a hip replacement surgery.
Moreover, the skill required for ECCE is foundational, offering surgeons a manual dexterity that is invaluable when complex complications occur during Phaco. The University of Michigan provides strong academic resources detailing the nuances of cataract surgical techniques and outcomes, supporting the need for versatile surgical skills.
📜 Patient Journey: The Safety of ECCE in a High-Risk Case
Case Study: Clara’s Corneal Preservation
Clara, a 68-year-old patient from the UK, had been diagnosed with an extremely advanced, dark brown (Grade 5) cataract. Furthermore, she had a pre-operative corneal assessment showing a low endothelial cell density, putting her at high risk for permanent corneal swelling if Phacoemulsification was performed with high energy. Therefore, her local surgeon advised a very guarded prognosis, highlighting the high risk of needing a follow-up corneal transplant.
The Decision to Choose ECCE Abroad
After researching comprehensive ophthalmic centers, Clara chose to travel to a specialty hospital renowned for its versatility in cataract surgery. Indeed, the consulting surgeon, an expert in both Phaco vs. ECCE, confirmed the high risk. Consequently, the surgeon recommended ECCE as the safest approach to preserve her already compromised cornea. Clara readily agreed, prioritizing long-term safety over fast recovery. She followed all the pre-travel guidance, including the pre-travel resources checklist.
The Outcome
The surgeon performed ECCE, removing the dense nucleus manually through the large, sutured incision. Thus, there was no internal ultrasonic energy exposure to the corneal endothelium. The initial visual recovery was slow, as expected, taking several weeks for the sutures to be removed and the cornea to stabilize. Nevertheless, Clara’s cornea remained clear, and her vision stabilized at a healthy 20/40, a successful and safer outcome than her guarded prognosis at home.
Clara’s experience is a powerful testament to the fact that ECCE is safer than Phaco in specific, high-risk conditions. Furthermore, it highlights the importance of choosing a doctor and clinic that can perform the full range of surgical options, reflecting a commitment to patient-centric care. Preparing for her medical travel also involved reviewing the country-specific information, such as the visa guide for Iran.
📩 Essential Questions for Your Surgeon
When consulting with an ophthalmologist, particularly in a medical tourism setting, your dialogue should focus on their adaptability. Therefore, ask probing questions to ascertain their comfort level and experience with the manual method. Consequently, a good surgeon will always be honest about the risks and the best plan for your unique eyes. Knowing the difference between Phaco vs. ECCE is your first line of defense.
Vetting Your Surgeon’s Dual Proficiency
- “Based on my cataract density, what is my risk of corneal endothelial cell loss with Phaco?”
- “How many ECCE procedures do you perform annually?”
- “What is your plan if a complication requires you to convert from Phaco to the ECCE technique?”
- “Given my corneal health, why do you recommend Phaco over ECCE, or vice-versa?”
- “If I have zonular weakness, what measures will you take to stabilize the IOL, and which procedure is safer?”
This line of questioning ensures your surgeon prioritizes safety. You can find experienced surgeons in our doctors directory. Furthermore, you should familiarize yourself with all preparation steps, similar to the pre-travel organization needed for gynecological surgery. The principles of safe medical travel remain consistent across specialties.
Moreover, the same due diligence should be applied when comparing complex treatments like bone marrow transplant or specialized departmental care. The ultimate goal is quality.
❓ Frequently Asked Questions (FAQ) about Phaco vs. ECCE Safety
No, the Intraocular Lens (IOL) options are generally the same. Both Phaco and ECCE aim to place the IOL securely within the posterior lens capsule. Modern, foldable IOLs can be inserted through the smaller Phaco incision, but they can also be placed through the larger ECCE incision just as effectively. The choice of IOL (monofocal, toric, or multifocal) is based on the patient’s vision needs, not the removal technique.
Phaco is often attempted due to patient expectation of a small incision and rapid recovery. Surgeons are trained to use techniques that minimize energy, but in many clinical settings, Phaco is the primary, or only, technique they are comfortable with. Furthermore, the modern trend sometimes pressures less experienced surgeons to avoid the “old school” ECCE, even when clinically indicated.
The primary factor is the density and color of the nucleus, often classified as Grade 4 (brown) or Grade 5 (black, or “brunescent”). This hardness indicates significant sclerosis and calcification, requiring much higher ultrasonic energy and longer Phaco time, directly increasing the risk to the corneal endothelium.
For a routine, soft cataract, Phaco can be completed in 10-15 minutes. A complex ECCE procedure takes longer, typically 25-45 minutes, due to the need for a larger incision, careful manual nucleus delivery, and meticulous suturing. However, attempting a high-energy Phaco on a hard cataract can also push the Phaco time well past 30 minutes, increasing risk without improving speed.
ECCE has a higher potential to induce post-operative astigmatism because the large incision changes the curvature of the cornea. However, modern ECCE utilizes specific surgical techniques, such as corneal or limbal incisions and precise, adjustable sutures, to minimize and correct this induced astigmatism, leading to excellent long-term visual outcomes.
Femtosecond Laser-Assisted Cataract Surgery (FLACS) can automate initial steps and pre-fragment the nucleus. This pre-fragmentation can reduce the total ultrasonic energy needed during the Phaco portion of the surgery. Therefore, FLACS can potentially make Phaco safer for moderately dense cataracts, but ECCE often remains the safest primary option for the most extreme, rock-hard cases.
A Phaco to ECCE conversion is the necessary switch to the manual technique mid-procedure when Phaco encounters a complication that cannot be safely managed through the small incision, such as a large posterior capsular tear or zonular failure. The ability to perform this conversion expertly is a vital measure of a surgeon’s overall skill and is crucial for patient safety.
No. ECCE (Extracapsular Cataract Extraction) is a modern, relevant technique that leaves the posterior lens capsule intact. ICCE (Intracapsular Cataract Extraction) is the obsolete method where the entire lens, including the capsule, was removed, leading to unstable IOL placement. ECCE is a safe alternative; ICCE is not.
Phaco restrictions are typically minimal and last only a few days to a week. ECCE restrictions are much stricter and longer, lasting 6 to 8 weeks. Patients must avoid heavy lifting, bending, or straining to ensure the large, sutured incision heals securely and does not lead to wound dehiscence or a pressure spike.
You should explicitly ask the clinic or medical tourism provider if their ophthalmic surgeons are proficient and routinely perform both Phaco and ECCE, especially for Grade 4 or 5 cataracts. Look for facilities listed in our doctors directory or those with a comprehensive ophthalmology department, as these are more likely to have the necessary dual capability.
Yes, ECCE is generally more cost-effective because it does not require the expensive, complex ultrasonic Phaco machine or its associated disposable parts. This cost differential is significant in many international medical tourism markets and contributes to the overall affordability of high-quality care. This is a common factor in comparing complex treatments, as seen when comparing PGT-A testing or fertility treatments abroad.
Yes. A skilled surgeon can correct pre-existing astigmatism by carefully placing the ECCE incision on the steepest corneal axis or by implanting a Toric IOL. While the large incision must be managed, modern techniques allow for excellent post-operative outcomes, and the primary benefit of corneal protection still outweighs the minor risk of induced astigmatism.
ECCE remains a vital part of surgical training globally for two main reasons. First, it is the safest technique for complex and advanced cataracts, ensuring residents are equipped to handle high-risk cases. Second, it is the necessary “bailout” procedure when a routine Phaco case encounters severe complications, making it a critical skill for all ophthalmologists. This dedication to foundational skills is the hallmark of quality education. You can learn more about general travel requirements in the definitive patient handbook.
The risk of severe post-operative infection (endophthalmitis) is low for both procedures in a modern, sterile operating room environment. While the larger wound of ECCE is theoretically a slightly greater portal for infection, meticulous surgical technique, careful wound closure, and the use of post-operative antibiotics effectively manage and mitigate this risk, ensuring safety remains high.
MSICS is a modern, suture-less, manual technique that is a refinement of ECCE, using a slightly smaller incision (6-8 mm) and a self-sealing scleral tunnel to avoid sutures and reduce astigmatism. MSICS is highly effective and safe for hard cataracts, particularly in high-volume settings, and can be seen as the ultimate safe middle ground between Phaco and traditional ECCE. Both MSICS and ECCE demonstrate that a manual approach is superior for hard nuclei.
Expert surgeons who maintain dual proficiency are commonly found in high-volume teaching hospitals and specialized centers in countries with strong medical tourism infrastructure, such as Iran, Turkey, and India. You should look for surgeons who explicitly list experience with complex cataracts and manual techniques on their profile. Utilizing our all locations page or the medical tourism Turkey guide can help you start your search for the right specialist.
Common visual restrictions include blurred vision for the first few weeks, especially due to the sutures, and a period of reliance on thick glasses until the cornea heals and sutures are removed. The visual recovery is gradual, with significant improvement often noticed only after the first month.
No. The cataract density and corneal health can differ significantly between eyes. If your first eye was a routine case for Phaco but the second eye developed a rock-hard cataract or you had an unexpected complication in the first, the surgeon may safely recommend ECCE for the second eye. The decision of Phaco vs. ECCE is made individually for each eye.