Description
Familiarity with treatment
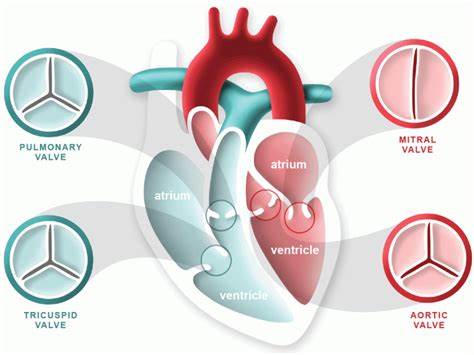
Aortic valve surgery encompasses a range of procedures aimed at addressing conditions affecting the aortic valve, including stenosis, regurgitation, and other structural abnormalities. These procedures may involve either repair or replacement of the aortic valve. Here are some key points about aortic valve surgery:
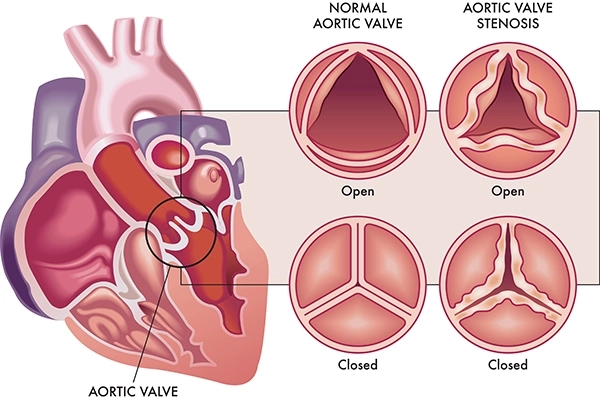
- Aortic Valve Stenosis:
- Aortic valve stenosis refers to the narrowing of the aortic valve, which obstructs the flow of blood from the left ventricle to the aorta. Surgical intervention may involve valve replacement, either with a mechanical or bioprosthetic valve, or in some cases, valve repair.
- Aortic Valve Regurgitation:
- Aortic valve regurgitation, also known as aortic insufficiency, occurs when the valve does not close properly, leading to the backflow of blood into the left ventricle. Surgical options for aortic valve regurgitation include repair or replacement of the valve.
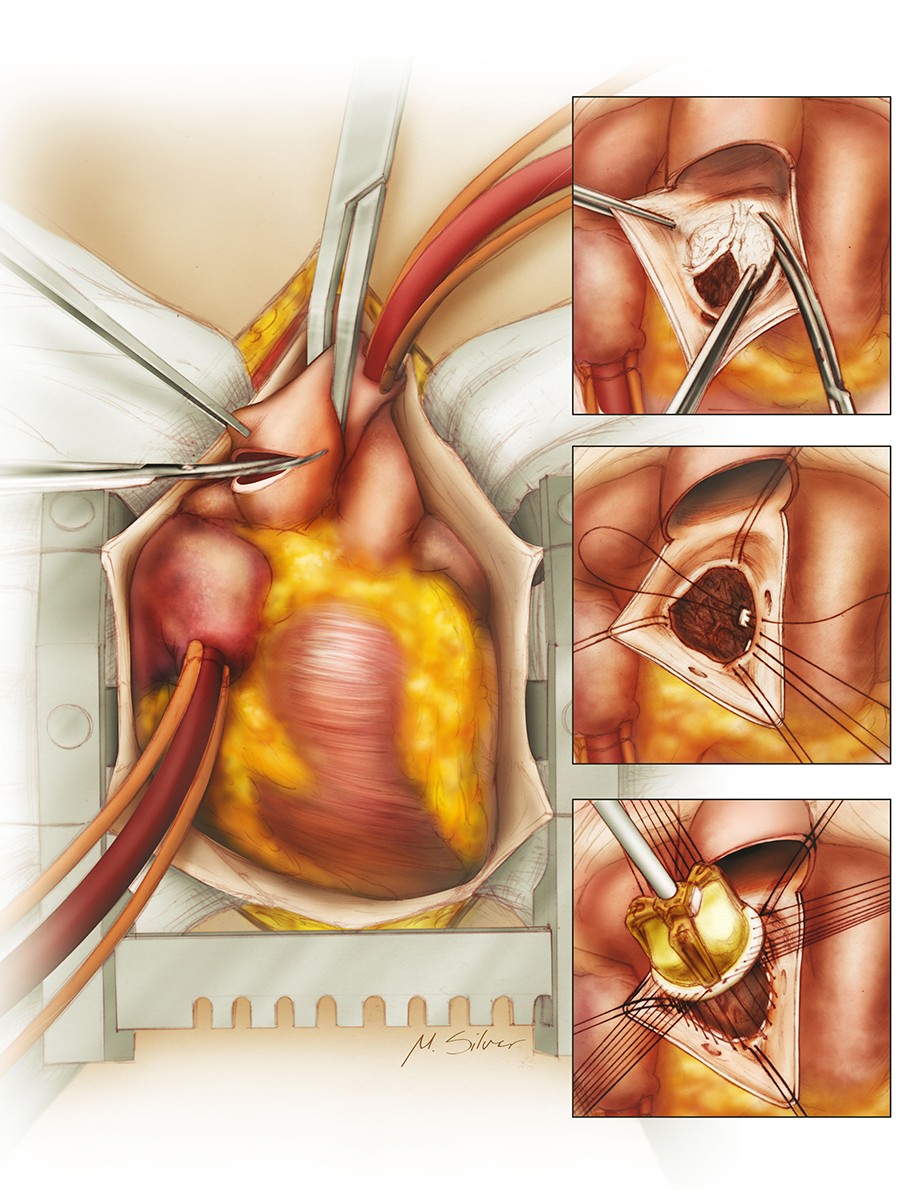
- Surgical Techniques:
- Aortic valve surgery can be performed using traditional open-heart surgical approaches or minimally invasive techniques, which may involve smaller incisions and less extensive surgical exposure.
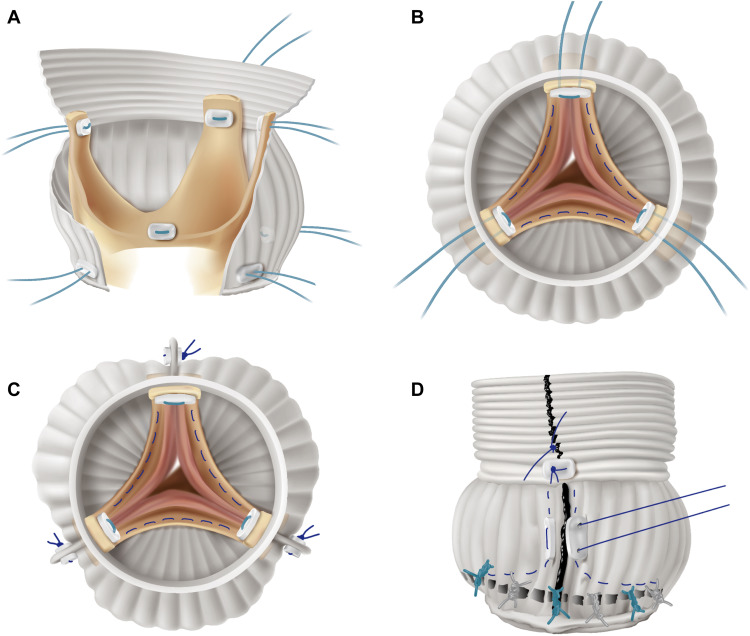
- Valve Repair:
- Aortic valve repair aims to preserve the patient’s natural valve whenever feasible, addressing structural abnormalities and restoring valve function without the need for complete valve replacement.
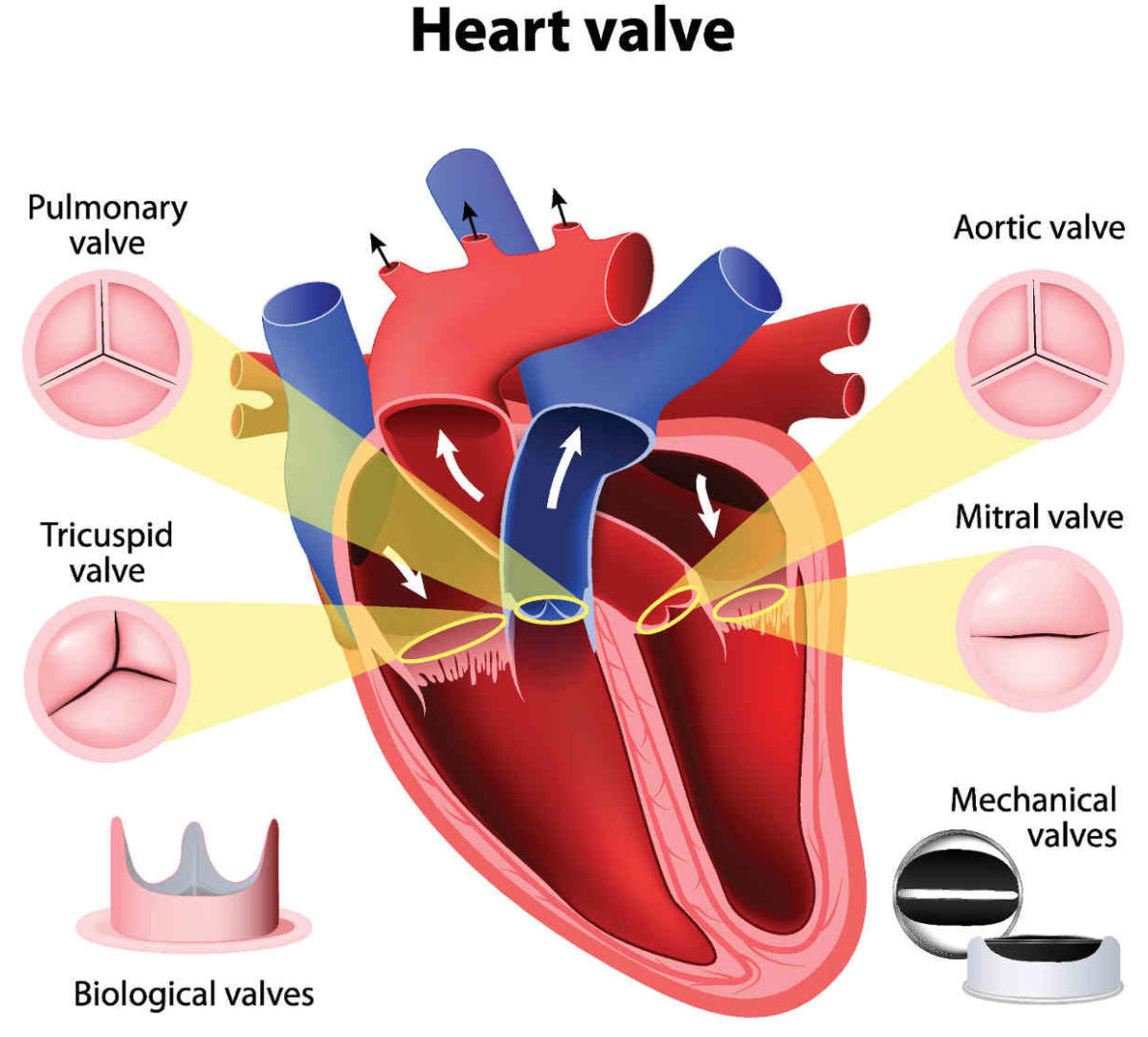
- Valve Replacement:
- When repair is not feasible or the valve is severely damaged, aortic valve replacement may be necessary. This can involve the implantation of a mechanical valve or a bioprosthetic (tissue) valve.
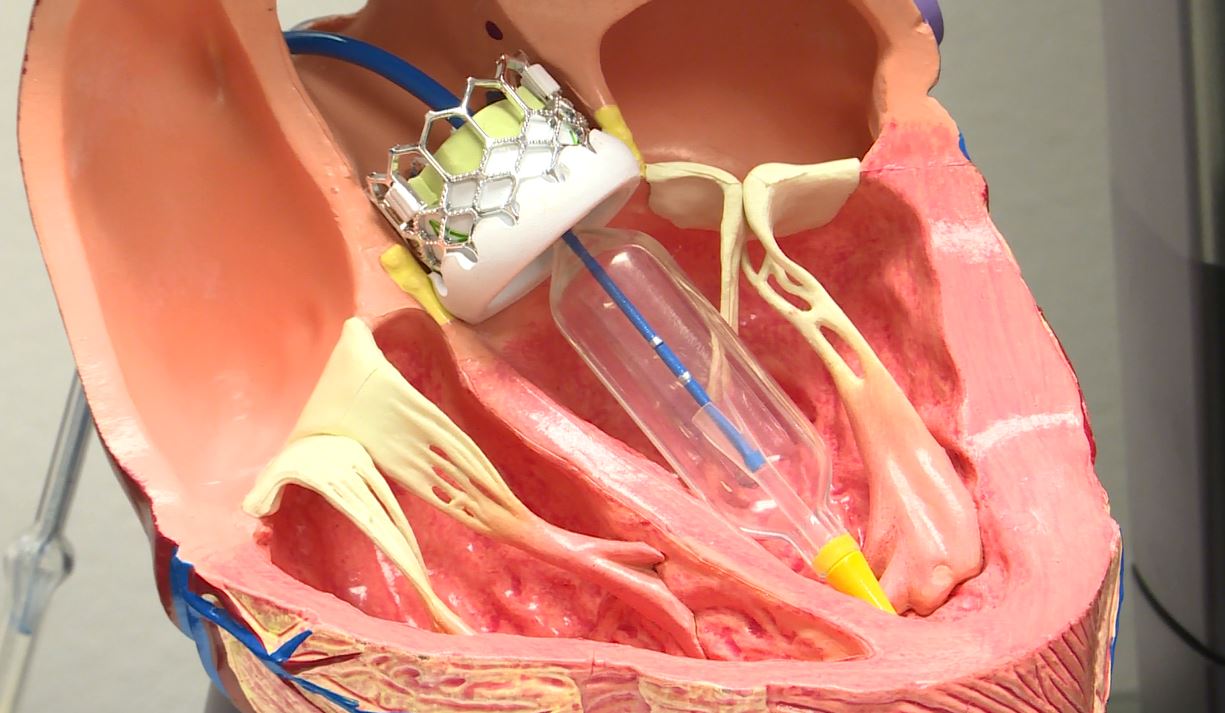
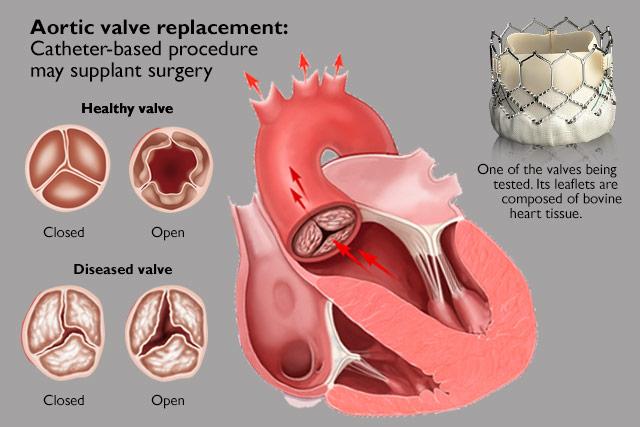
- Transcatheter Aortic Valve Replacement (TAVR):
- TAVR is a minimally invasive procedure that allows for the replacement of the aortic valve without open-heart surgery. This approach is typically used for individuals at higher risk for traditional surgical intervention.
- Preoperative Evaluation:
- Prior to aortic valve surgery, patients undergo comprehensive preoperative evaluation, including imaging studies, cardiac assessments, and risk stratification to determine the most suitable treatment approach.
- Recovery and Rehabilitation:
- Following aortic valve surgery, patients undergo postoperative care, including monitoring in the intensive care unit, rehabilitation, and long-term follow-up to ensure optimal recovery and management of the repaired or replaced valve.
- Risk and Benefits:
- Aortic valve surgery carries potential risks, such as bleeding, infection, and adverse reactions to anesthesia, but it also offers the potential for improved quality of life, symptom relief, and enhanced cardiovascular function.
- Long-Term Management:
- Individuals who undergo aortic valve surgery require long-term management, including surveillance for potential complications, adherence to medication regimens, and lifestyle modifications to support cardiovascular health.
Who is it suitable for?
Aortic valve surgery is suitable for individuals with aortic valve pathologies such as severe stenosis, regurgitation, or other structural abnormalities that significantly impair valve function and overall cardiovascular health. The decision to undergo aortic valve surgery is based on a thorough evaluation of the patient’s condition and the consideration of various factors. Here are some key points regarding who may be suitable for aortic valve surgery:
- Severe Aortic Valve Stenosis:
- Individuals with severe narrowing of the aortic valve, leading to obstruction of blood flow from the left ventricle to the aorta, may be suitable candidates for aortic valve surgery.
- Severe Aortic Valve Regurgitation:
- Patients with severe aortic valve regurgitation, where the valve does not close properly, resulting in the backflow of blood into the left ventricle, may benefit from aortic valve surgery to correct the structural abnormality.
- Symptomatic Patients:
- Aortic valve surgery is often recommended for symptomatic individuals, such as those experiencing chest pain, shortness of breath, fatigue, or syncope, related to their aortic valve pathology.
- Asymptomatic Patients with Severe Pathology:
- In some cases, even asymptomatic individuals with severe aortic valve pathologies may be considered for surgery based on the severity of the condition and the risk of disease progression.
- High-Risk Patients for Transcatheter Aortic Valve Replacement (TAVR):
- Individuals who are at high risk for traditional open-heart surgery may be suitable candidates for TAVR, a minimally invasive approach for aortic valve replacement.
- Patients with Compromised Quality of Life:
- Aortic valve surgery may be considered for patients whose quality of life is significantly impacted by their aortic valve pathology, despite optimal medical management.
- Patients with Indications for Valve Repair:
- Individuals with specific indications for aortic valve repair, such as certain forms of valve disease amenable to surgical correction, are suitable candidates for this intervention.
- Those with Favorable Risk-Benefit Profile:
- The suitability for aortic valve surgery is determined based on a comprehensive assessment of the patient’s overall health, cardiac function, comorbid conditions, and the anticipated risk-benefit profile of the intervention.
- Patients with Appropriate Anatomy for Intervention:
- Suitability for aortic valve surgery also involves consideration of the patient’s aortic valve anatomy, suitability for potential interventions, and the presence of additional cardiac or vascular pathologies.
Who is it not suitable for?
Aortic valve surgery may not be suitable for certain individuals based on their specific clinical circumstances and overall health. The decision to pursue or forego aortic valve surgery is influenced by various factors, and there are situations where the risks of surgery may outweigh the potential benefits. Here are some scenarios in which aortic valve surgery may not be suitable:
- Poor Surgical Candidate:
- Individuals with significant comorbidities or advanced age may be deemed poor candidates for aortic valve surgery due to the increased risks associated with the procedure and the potential impact on overall health and quality of life.
- Limited Life Expectancy:
- In cases where a patient has a limited life expectancy due to advanced age, frailty, or serious systemic illnesses, the potential benefits of aortic valve surgery may not outweigh the risks, and alternative management options may be considered.
- Severe End-Stage Organ Dysfunction:
- Patients with severe, end-stage organ dysfunction, such as advanced renal failure, liver disease, or respiratory insufficiency, may not be suitable candidates for aortic valve surgery due to the high risk of perioperative complications and limited expected benefits.
- Unacceptable Surgical Risk:
- Individuals with an unacceptably high surgical risk, such as those with severe pulmonary hypertension, extensive coronary artery disease, or other complex cardiac conditions, may not be considered suitable candidates for aortic valve surgery.
- Limited Functional Status:
- Patients with severely limited functional status and poor baseline functional capacity may face challenges in tolerating the stress of surgery and the potential postoperative recovery, leading to a determination that aortic valve surgery is not suitable.
- Patient Preference:
- In some cases, a patient’s personal preferences and values may lead them to decline aortic valve surgery, even if they meet clinical criteria, based on their individual perspectives on quality of life, treatment goals, and potential risks.
- Unfavorable Valve Anatomy for Intervention:
- Individuals with unfavorable aortic valve anatomy, such as complex valve pathology or anatomy not amenable to surgical or transcatheter interventions, may not be suitable candidates for aortic valve surgery.
- Rapid Decline or Poor Prognosis:
- Patients with rapidly declining health, a poor overall prognosis, or advanced stages of terminal illness may not be considered suitable for aortic valve surgery, as the potential benefits may be limited in the context of their clinical trajectory.
- Clear Contradictions to Surgery:
- Patients with clear contradictions to undergoing surgery, such as those with active infections, uncontrolled bleeding disorders, or other conditions that preclude safe surgical intervention, may not be suitable candidates for aortic valve surgery.
Advantages
Aortic valve surgery offers several potential advantages for individuals with significant aortic valve pathologies, such as stenosis, regurgitation, or other structural abnormalities. The decision to undergo aortic valve surgery is based on a comprehensive assessment of the patient’s clinical condition and the potential benefits of the intervention. Here are some of the advantages of aortic valve surgery:
- Symptom Relief:
- Aortic valve surgery can provide significant relief from symptoms associated with aortic valve pathologies, such as chest pain, shortness of breath, fatigue, dizziness, and syncope, leading to improved quality of life and functional capacity.
- Prolonged Life Expectancy:
- Addressing severe aortic valve pathologies through surgery can contribute to improved long-term survival and may reduce the risk of adverse cardiovascular events associated with untreated or poorly managed valvular disease.
- Improved Cardiac Function:
- Aortic valve surgery can help restore normal hemodynamics, reduce left ventricular hypertrophy, and improve cardiac function, contributing to enhanced cardiovascular performance and overall well-being.
- Prevention of Disease Progression:
- Surgery for aortic valve pathologies can halt the progression of the disease, preventing further deterioration of valve function and potential complications associated with advanced valvular disease.
- Enhanced Exercise Tolerance:
- Addressing severe aortic valve pathologies through surgery may lead to improved exercise tolerance, reduced exertional symptoms, and the ability to engage in physical activities with greater comfort and capacity.
- Reduction of Heart Failure Risk:
- Aortic valve surgery can reduce the risk of developing heart failure or slow the progression of existing heart failure by addressing the underlying valve pathology and optimizing cardiac function.
- Treatment of Severe Symptoms:
- For individuals with severe aortic valve stenosis or regurgitation, aortic valve surgery can effectively alleviate debilitating symptoms and improve the patient’s overall well-being.
- Opportunity for Valve Repair:
- In cases where aortic valve repair is feasible, surgery can preserve the patient’s natural valve, potentially avoiding the long-term anticoagulation requirements associated with mechanical valve replacement.
- Potential for Transcatheter Aortic Valve Replacement (TAVR):
- For individuals at high surgical risk, TAVR offers a minimally invasive alternative to traditional open-heart surgery, providing the benefits of aortic valve replacement with reduced procedural morbidity.
- Individualized Treatment:
- Aortic valve surgery allows for individualized treatment tailored to the specific characteristics of the patient’s valve pathology, anatomy, and overall cardiovascular health, addressing their unique clinical needs.
Complications
Aortic valve surgery, like any surgical procedure, carries the potential for various complications. While these complications are not guaranteed to occur, it is important for patients to be aware of the potential risks associated with aortic valve surgery. Here are some of the potential complications:
- Bleeding and Hemorrhage:
- Surgical procedures, including aortic valve surgery, carry a risk of bleeding during or after the operation, which may necessitate blood transfusions or additional interventions to control bleeding.
- Infection:
- Infection at the surgical site or within the chest cavity (such as mediastinitis) is a potential complication of aortic valve surgery, which can be serious and may require antibiotic treatment or surgical drainage.
- Arrhythmias:
- Irregular heart rhythms, including atrial fibrillation, can occur after aortic valve surgery, requiring management with medications or, in some cases, electrical cardioversion.
- Stroke:
- There is a risk of stroke associated with aortic valve surgery, particularly during the perioperative period, due to embolization of blood clots or other factors, which can lead to neurological deficits.
- Pulmonary Complications:
- Complications such as pneumonia, atelectasis, or respiratory insufficiency can occur following aortic valve surgery, particularly in patients with underlying lung disease or those with prolonged intubation.
- Acute Kidney Injury:
- Some individuals may experience acute kidney injury following aortic valve surgery, particularly if there are complications related to reduced blood flow or the effects of medications used during the procedure.
- Thromboembolic Events:
- Following aortic valve replacement, there is a risk of thromboembolic events, such as blood clots leading to stroke, transient ischemic attack (TIA), or peripheral embolization, particularly in the context of mechanical valve replacement.
- Valve Dysfunction:
- Complications related to the aortic valve itself, such as prosthetic valve dysfunction (e.g., stenosis, regurgitation, thrombosis), may require reintervention or long-term anticoagulation therapy.
- Cardiac Tamponade:
- Cardiac tamponade, a condition where fluid accumulates around the heart, can occur as a rare but serious complication of aortic valve surgery, requiring urgent intervention to relieve the pressure on the heart.
- Prosthetic Valve Endocarditis:
- Infection of a prosthetic valve, known as prosthetic valve endocarditis, is a potential long-term complication that may require prolonged antibiotic therapy or, in severe cases, surgical intervention.
- Psychological and Emotional Effects:
- Some individuals may experience psychological and emotional effects following aortic valve surgery, including anxiety, depression, or adjustment difficulties related to the surgical experience and recovery process.
Previous care
The preoperative care for aortic valve surgery is a critical component of the overall treatment process and is essential for ensuring the best possible outcomes for the patient. Here are the key aspects of preoperative care for aortic valve surgery:
- Comprehensive Evaluation:
- Patients undergo a comprehensive evaluation, which includes a detailed medical history, physical examination, and assessment of cardiac function. This evaluation helps the healthcare team understand the patient’s overall health and identify any potential risks associated with surgery.
- Diagnostic Testing:
- Diagnostic tests such as echocardiography, electrocardiography, chest X-ray, and cardiac catheterization may be performed to assess the severity of the aortic valve pathology, evaluate cardiac function, and identify any associated cardiovascular conditions.
- Risk Stratification:
- Risk stratification is conducted to assess the patient’s surgical risk, taking into account factors such as age, comorbidities, functional status, and the severity of the aortic valve pathology. This helps in determining the most appropriate treatment approach and setting realistic expectations for the patient.
- Multidisciplinary Consultation:
- Patients may be evaluated by a multidisciplinary team of healthcare providers, including cardiologists, cardiac surgeons, anesthesiologists, and other specialists, to ensure a comprehensive and individualized approach to their care.
- Optimization of Medical Management:
- Preoperative medical management may include the optimization of medications to address cardiovascular conditions, such as heart failure or coronary artery disease, and to minimize the risk of perioperative complications.
- Patient Education:
- Patients receive thorough education about the nature of their aortic valve pathology, the rationale for surgery, the potential risks and benefits of the procedure, and the expected postoperative recovery process. Informed consent is obtained from the patient after they have a clear understanding of the procedure.
- Psychosocial Support:
- Psychosocial support, including counseling and support services, may be provided to address the emotional and psychological aspects of undergoing cardiac surgery, helping to alleviate anxiety and promote coping strategies.
- Smoking Cessation and Lifestyle Modifications:
- Patients who smoke are encouraged to quit smoking, and all patients are advised to make lifestyle modifications, such as adopting a heart-healthy diet and engaging in regular exercise, to optimize their overall health and prepare for surgery.
- Preoperative Medications:
- Depending on the patient’s clinical condition, medications such as anticoagulants, antiplatelet agents, or antibiotics may be prescribed in the preoperative period to manage specific cardiovascular or infectious concerns.
- Logistical Planning:
- Logistical aspects of the surgery, such as scheduling, preadmission testing, and coordination with the surgical team and hospital staff, are managed to ensure a smooth transition into the operative phase.
- Advance Directives and Care Planning:
- Discussions about advance directives, care preferences, and potential postoperative care needs are conducted to address the patient’s values and preferences regarding their medical care.
Aftercare
The postoperative or aftercare following aortic valve surgery is crucial for the patient’s recovery and long-term health. It involves a combination of medical management, monitoring, rehabilitation, and patient education. Here are the key components of aftercare following aortic valve surgery:
- Intensive Care Unit (ICU) Monitoring:
- After surgery, patients are typically monitored in the ICU for a period of time to closely track their vital signs, cardiac function, and overall recovery from the procedure.
- Pain Management:
- Adequate pain management is provided to ensure the patient’s comfort during the immediate postoperative period. This may involve the use of pain medications and other pain management techniques.
- Monitoring for Complications:
- Healthcare providers closely monitor for potential complications such as bleeding, infection, arrhythmias, respiratory issues, and other postoperative concerns, intervening as necessary to address any issues that may arise.
- Early Mobilization:
- Patients are encouraged to start moving and engaging in early mobilization as soon as it is safe to do so, with the goal of preventing complications such as deep vein thrombosis and promoting a faster recovery.
- Cardiac Rehabilitation:
- Cardiac rehabilitation programs may be recommended to help patients regain strength, improve cardiovascular fitness, and learn about heart-healthy lifestyle behaviors following aortic valve surgery.
- Medication Management:
- Patients receive instructions regarding their postoperative medication regimen, which may include medications to manage pain, prevent infection, control blood pressure, and address specific cardiac conditions.
- Wound Care:
- Patients and their caregivers receive guidance on caring for the surgical incision site, including instructions on wound dressing changes, signs of infection to watch for, and when to seek medical attention for wound-related concerns.
- Dietary Guidance:
- Patients receive dietary guidance to support their recovery, including recommendations for heart-healthy eating patterns, fluid management, and any specific dietary considerations related to their postoperative condition.
- Activity Restrictions and Gradual Resumption:
- Healthcare providers provide clear instructions regarding activity restrictions, such as lifting restrictions, driving limitations, and guidelines for gradually resuming daily activities and exercise.
- Follow-Up Appointments:
- Patients are scheduled for follow-up appointments with their healthcare providers to monitor their progress, assess their cardiac function, adjust medications as needed, and address any concerns or questions related to their recovery.
- Patient Education and Support:
- Ongoing patient education and support are provided to address the patient’s questions, concerns, and needs related to their recovery, including emotional support and guidance on adapting to lifestyle changes.
- Long-Term Surveillance:
- Long-term surveillance and monitoring are conducted to assess the function of the aortic valve prosthesis, address any potential complications, and optimize the patient’s cardiac health over time.





Reviews
There are no reviews yet.