Description
Familiarity with treatment
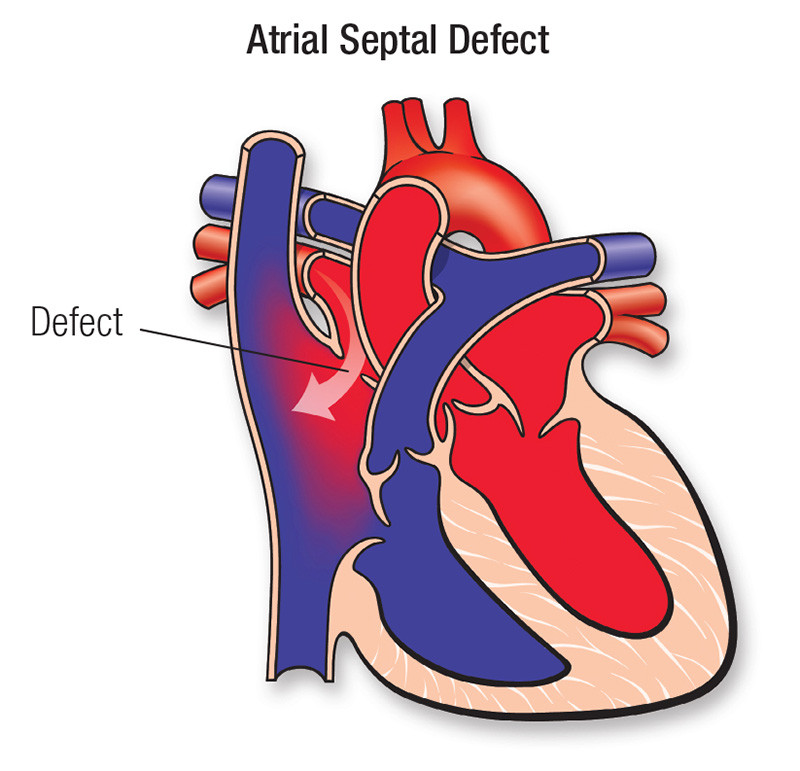
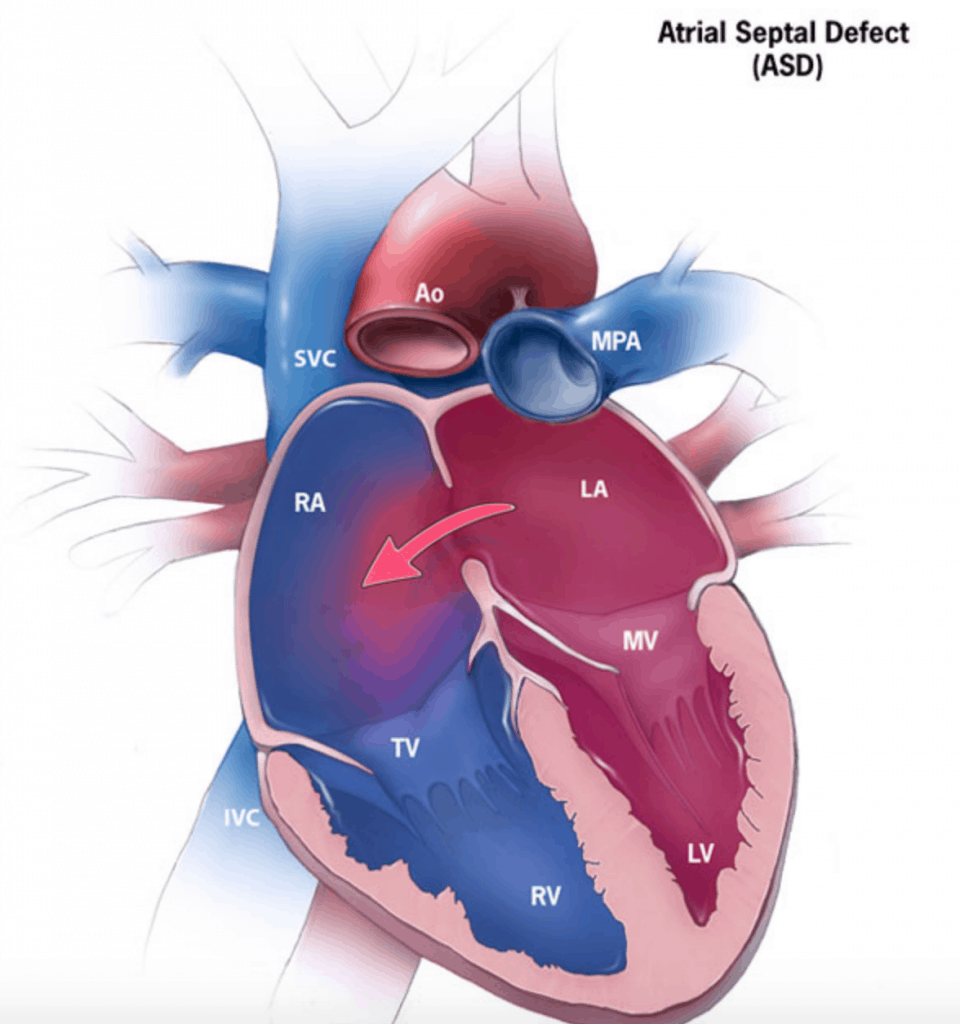
Atrial Septal Defect (ASD) repair surgery is a procedure performed to close an opening in the wall (septum) separating the left and right upper chambers (atria) of the heart. The surgery can be performed using different techniques, including open-heart surgery and minimally invasive catheter-based closure.
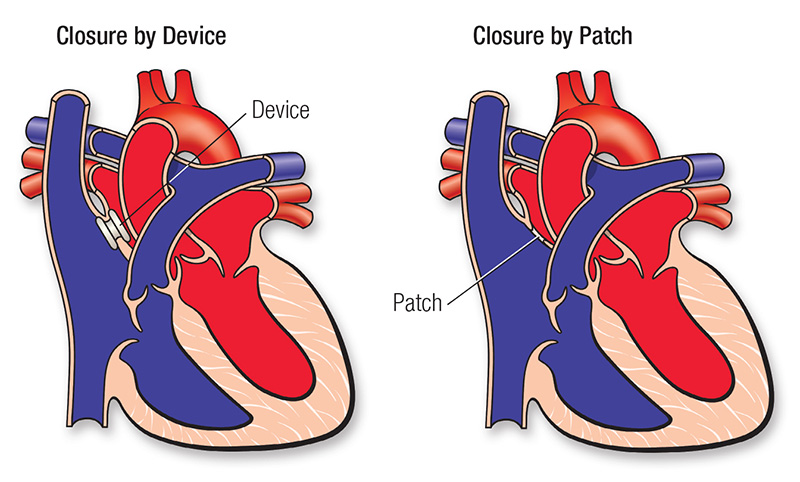
Open-heart surgery: In open-heart surgery, an incision is made in the chest to access the heart. The heart is temporarily stopped, and the patient is connected to a heart-lung machine. The surgeon then closes the ASD using stitches or a patch. This approach is typically used for larger defects or when the ASD is in a complex location. 1
Catheter-based closure: Minimally invasive catheter-based closure is an alternative to open-heart surgery for certain types of ASDs. A catheter is inserted through a small incision in the leg and guided to the heart using imaging techniques. A device, such as a mesh patch or umbrella-like occluder, is then deployed to close the ASD. This approach avoids the need for a large incision and can result in a faster recovery time. 1
The choice of surgical technique depends on various factors, including the size and location of the ASD, the patient’s age, and the presence of other heart conditions. The decision is made by the cardiac surgeon based on a thorough evaluation of the individual case.
Who is it suitable for?
Atrial Septal Defect (ASD) repair surgery is suitable for individuals who have been diagnosed with an ASD and meet certain criteria. Here are some key points from the search results:
Size and Type of ASD: The suitability for surgery depends on the size and type of ASD. Surgery is often recommended for medium to large ASDs diagnosed during childhood or adulthood to prevent future complications 1.
Persistent ASD: Many persistent ASDs eventually require surgery. Closure of the defect is recommended to prevent complications such as enlargement of the heart chambers and damage to lung blood vessels 1.
Severe Pulmonary Hypertension: Closure of the ASD may not be recommended if severe pulmonary hypertension is present.
Minimally Invasive Options: Minimally invasive catheter-based closure procedures, such as transcatheter repair, may be suitable for certain types of ASDs. These procedures offer less invasive approaches and shorter recovery times compared to open-heart surgery.
Children and Adults: ASD repair surgery can be performed in both children and adults. The decision for surgery is based on factors such as the size and location of the defect, the patient’s age, and the presence of other heart conditions 2.
Who is it not suitable for?
Atrial Septal Defect (ASD) repair surgery may not be suitable for certain individuals based on specific factors and conditions. Here are some instances where surgery may not be recommended, as mentioned in the search results:
Small ASDs: Small ASDs, especially those that are asymptomatic and not causing significant complications, may not require surgical intervention. In such cases, the healthcare provider may opt for a conservative approach and monitor the condition over time.
Severe Pulmonary Hypertension: If an individual has severe pulmonary hypertension (high blood pressure in the lungs), surgical closure of the ASD may not be recommended. The presence of severe pulmonary hypertension can increase the risk of complications during surgery.
Multiple or Complex Heart Defects: In cases where an individual has multiple or complex congenital heart defects in addition to the ASD, the suitability for surgery will depend on the overall condition and the potential risks and benefits associated with the procedure. A multidisciplinary team of healthcare professionals, including cardiac surgeons, will assess the situation and make recommendations based on the individual’s specific condition.
Poor General Health: Individuals with significant comorbidities or poor overall health may not be suitable candidates for ASD repair surgery. The risks associated with the surgical procedure may outweigh the potential benefits in such cases.
Individual Preference: In some instances, an individual may choose not to undergo surgery, even if it is recommended by healthcare professionals. This decision is made after thorough discussions between the patient and their healthcare provider, taking into consideration the risks, benefits, and personal circumstances.
Advantages
When it comes to the advantages of Atrial Septal Defect (ASD) repair surgery, the search results highlight several key points:
Prevention of Complications: Closing the ASD through surgery helps prevent potential complications associated with the defect. These complications can include enlargement of the heart chambers, abnormal heart rhythms, and damage to the lung blood vessels.
Improved Quality of Life: Repairing the ASD can lead to an improved quality of life for individuals. Closure of the defect allows the heart to function more efficiently, reducing symptoms such as fatigue, shortness of breath, and exercise intolerance.
Reduced Risk of Infections: ASD closure surgery eliminates the opening in the heart, reducing the risk of infections, such as endocarditis, which can occur when bacteria enter the bloodstream and attach to the heart’s inner lining.
Prevention of Right Heart Strain: Large ASDs can cause increased blood flow and strain on the right side of the heart. Surgical closure of the defect helps alleviate this strain, allowing the heart to work more effectively.
Minimally Invasive Options: For suitable candidates, minimally invasive catheter-based closure procedures offer advantages such as smaller incisions, shorter recovery times, and potentially less postoperative pain compared to traditional open-heart surgery.
Complications
The search results provide insights into the potential complications associated with Atrial Septal Defect (ASD) repair surgery. Here are some key points based on the information:
Morbidity and Mortality: While ASD repair surgery is generally considered safe and effective with little to no morbidity and mortality, as mentioned in a study, it’s important to note that all surgical procedures carry some level of risk, and complications can occur in rare cases.
Pulmonary Hypertension: Severe pulmonary hypertension can impact the suitability for ASD closure surgery. Closure may not be recommended if severe pulmonary hypertension is present, as mentioned in the Mayo Clinic source.
Arrhythmia Complications: Postoperative management after ASD repair may involve monitoring for arrhythmia complications. Surgery for an ASD may be associated with a long-term risk of atrial fibrillation or flutter, as mentioned in the source discussing postoperative management.
Unusual Position of ASD: If the ASD is in an unusual position within the heart or if there are other heart defects, such as abnormal connections of the veins bringing blood from the lungs back to the heart, the ASD may not be suitable for closure with catheter-based techniques, and surgery may be needed.
Complex Cases: In cases where an individual has multiple or complex congenital heart defects in addition to the ASD, the suitability for surgery will depend on the overall condition and the potential risks and benefits associated with the procedure.
Previous care
Regarding previous care for Atrial Septal Defect (ASD), it’s important to note that the specific care and treatment options can vary depending on the individual’s condition, the size and location of the defect, and other factors. However, here are some common aspects of care that may be involved:
Monitoring and Evaluation: Individuals diagnosed with an ASD may undergo regular monitoring and evaluation by a healthcare professional, typically a cardiologist. This can involve periodic check-ups, echocardiograms, and other diagnostic tests to assess the size and progression of the defect and to monitor any associated complications.
Medication: In some cases, medication may be prescribed to manage symptoms or associated conditions. For example, medications may be used to control high blood pressure or to prevent blood clots in certain situations.
Lifestyle Modifications: Healthcare providers may recommend certain lifestyle modifications to manage the condition. This can include regular exercise, a heart-healthy diet, weight management, and avoiding activities that may strain the heart.
Preventive Measures: Individuals with an ASD may be advised to take preventive measures to reduce the risk of complications. This can include measures such as maintaining good oral hygiene to prevent infections that can affect the heart, and taking antibiotics before certain dental or medical procedures to prevent endocarditis.
Surgical Intervention: In cases where the ASD is large, causing significant symptoms, or associated with complications, surgical intervention may be recommended. The specific type of surgery (open-heart or minimally invasive catheter-based closure) will depend on various factors, as discussed earlier.
Aftercare
Aftercare following Atrial Septal Defect (ASD) repair surgery is an essential part of the recovery process. While the specific aftercare instructions may vary depending on the surgical approach and individual circumstances, here are some general aspects that might be involved:
Hospital Stay: After surgery, the individual will typically spend a few days in the hospital for monitoring and recovery. The healthcare team will closely monitor vital signs, pain management, and wound healing during this time.
Medications: Medications may be prescribed to manage pain, prevent infection, and prevent blood clot formation. It’s important to follow the prescribed medication regimen and report any adverse effects or concerns to the healthcare provider.
Wound Care: Proper care of the surgical incision site is crucial for healing. The healthcare team will provide instructions on how to keep the incision clean and dry, and when to change dressings, if necessary.
Physical Activity and Rest: The healthcare provider will provide guidance on physical activity and rest. Initially, there may be limitations on strenuous activities, and gradually, the individual can increase their activity level as healing progresses. It’s important to follow the recommended activity guidelines to prevent complications.
Follow-up Visits: Regular follow-up visits with the healthcare provider are typically scheduled to monitor the healing process and assess the overall recovery. These visits may include physical examinations, echocardiograms, or other diagnostic tests to ensure optimal healing and assess the success of the procedure.
Lifestyle Modifications: The healthcare provider may recommend certain lifestyle modifications to promote heart health and overall well-being. This can include adopting a heart-healthy diet, maintaining a healthy weight, managing stress, and avoiding tobacco and excessive alcohol consumption.
Educational Support: Education regarding self-care and recognizing signs of potential complications is crucial. The healthcare team will provide information on symptoms to monitor, when to seek medical assistance, and any specific care instructions based on the individual’s circumstances.







Reviews
There are no reviews yet.