Description
Familiarity with treatment
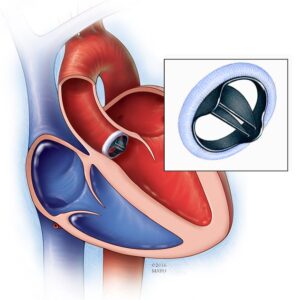
Coronary Artery Bypass Grafting (CABG) is a surgical procedure used to improve blood flow to the heart by bypassing narrowed or blocked coronary arteries. It is also known as heart bypass surgery. Here are some key points about CABG:
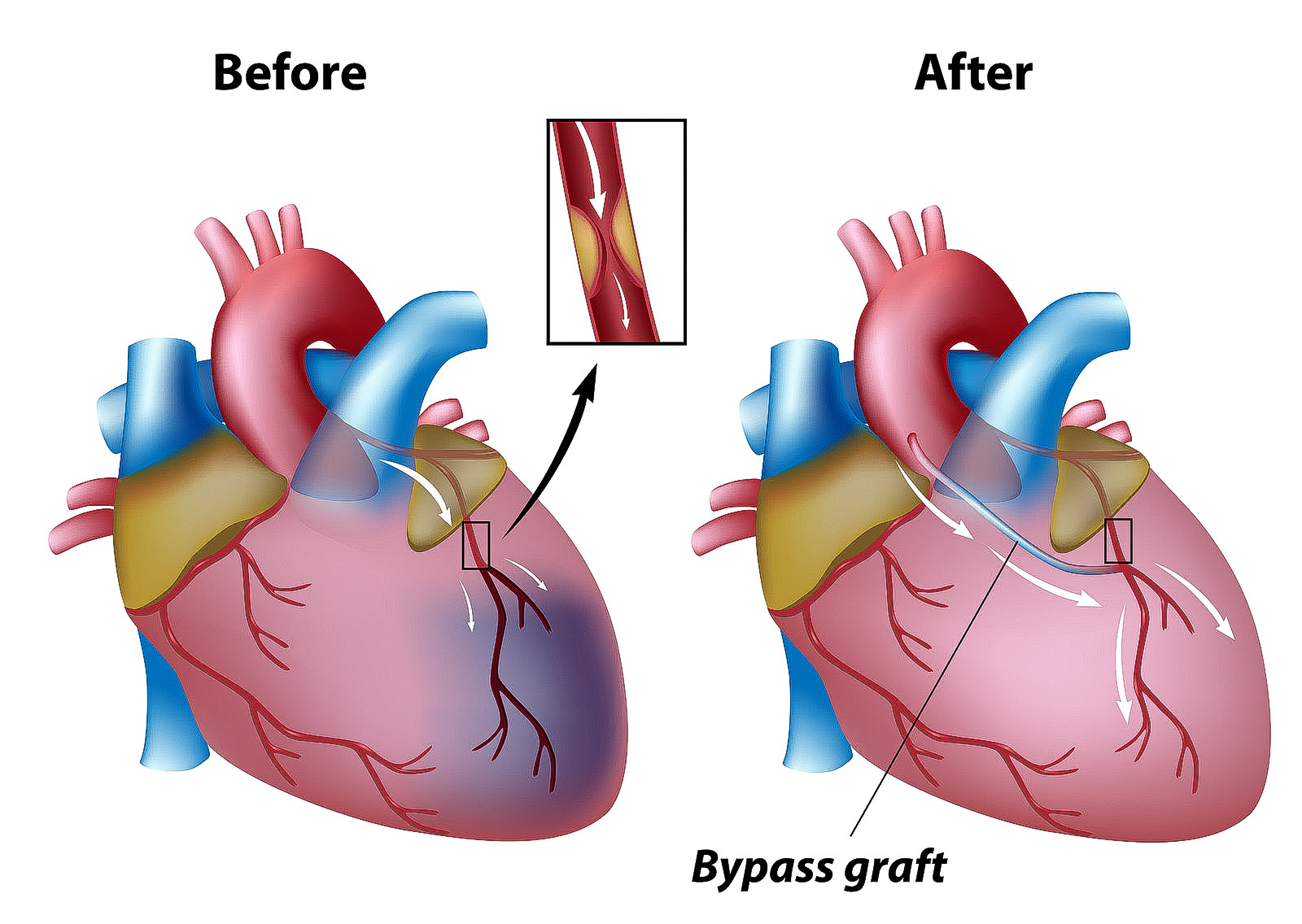
- CABG is typically recommended for individuals with coronary artery disease (CAD) who have blockages or narrowing in their coronary arteries that restrict blood flow to the heart muscle.
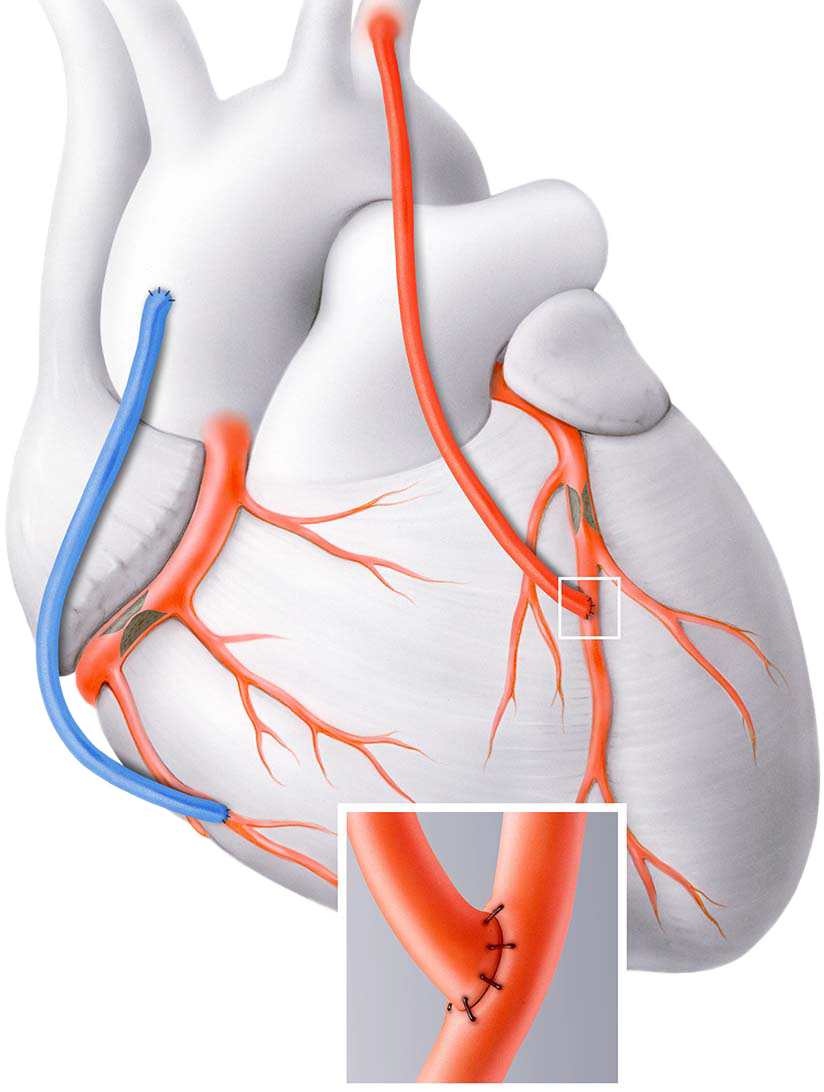
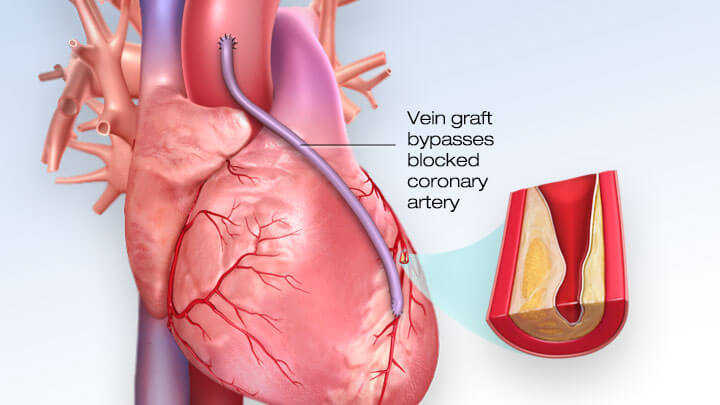
- The procedure involves taking a healthy blood vessel, usually from the chest, leg, or arm, and using it to create a new pathway for blood to flow around the blocked or narrowed coronary artery.
- The new blood vessel, known as a graft, is attached above and below the blocked area, allowing blood to bypass the blockage and reach the heart muscle.
- CABG is performed under general anesthesia, and the surgeon may use a heart-lung bypass machine to temporarily take over the heart’s pumping function during the procedure.
- The internal mammary artery (IMA) from the chest and the saphenous vein from the leg are commonly used as grafts in CABG surgery.
- The goals of CABG include improving blood flow to the heart, relieving symptoms such as chest pain (angina), reducing the risk of heart attack, and improving overall heart function.
- Risks associated with CABG include bleeding, infection, irregular heartbeat, stroke, kidney failure, and graft failure. However, serious complications are rare.
- Recovery after CABG typically involves a hospital stay of about 7 days, during which time the patient’s condition is closely monitored.
- After discharge, patients will need to follow a comprehensive cardiac rehabilitation program, which may include lifestyle modifications, medication management, and regular follow-up appointments with their healthcare team.
Who is it suitable for?
Coronary Artery Bypass Grafting (CABG) surgery is suitable for individuals with coronary artery disease (CAD) who meet certain criteria. CABG surgery may be recommended for the following groups of patients:
- Severe Coronary Artery Disease: CABG surgery is typically considered for individuals with severe CAD, which involves significant blockages or narrowing in the coronary arteries. The decision to undergo CABG is based on the extent and severity of the blockages, as well as the symptoms and overall health of the patient.
- Angina Symptoms: CABG surgery may be recommended for individuals with angina (chest pain) that is not adequately controlled with medications or other interventions. CABG can improve blood flow to the heart muscle, relieving angina symptoms and improving quality of life.
- Left Main Coronary Artery Disease: CABG surgery is often recommended for individuals with significant blockages in the left main coronary artery, which supplies a large portion of the heart. This condition is considered high-risk, and CABG surgery can provide better outcomes compared to other treatment options.
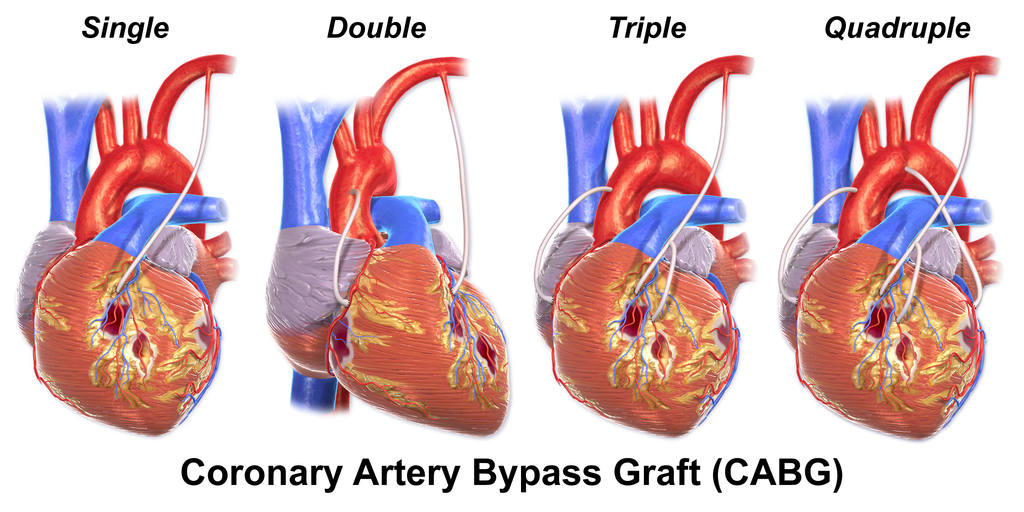
- Triple-Vessel Disease: CABG surgery may be suitable for individuals with blockages in three major coronary arteries. In such cases, CABG can provide comprehensive revascularization by bypassing all three blocked arteries, improving blood flow to the heart.
- Diabetes and CAD: Individuals with diabetes and significant CAD may benefit from CABG surgery. Studies have shown that CABG surgery may offer better outcomes and long-term survival compared to other treatments, particularly in individuals with diabetes and multi-vessel disease.
- Failed Non-Surgical Interventions: CABG surgery may be considered for individuals who have previously undergone non-surgical interventions, such as angioplasty and stenting, but have experienced recurrent blockages or complications. In such cases, CABG surgery can provide a more durable and long-lasting solution for restoring blood flow to the heart.
Who is it not suitable for?
Coronary Artery Bypass Grafting (CABG) may not be suitable for everyone with coronary artery disease (CAD) or certain medical conditions. The decision to undergo CABG is typically made on an individual basis, taking into consideration various factors. Here are some situations where CABG may not be recommended:
Minimal or no symptoms: If an individual has minimal or no symptoms of angina (chest pain) despite having significant blockages in the coronary arteries, CABG may not be necessary. In such cases, the risks and benefits of the procedure need to be carefully evaluated.
Advanced age or poor overall health: Advanced age or significant comorbidities may increase the risks associated with CABG. In some cases, alternative treatments or palliative care may be more appropriate.
Limited life expectancy: If an individual has a limited life expectancy due to advanced age, underlying medical conditions, or other factors, the potential benefits of CABG may not outweigh the risks or potential complications.
Unstable or high-risk condition: In certain situations where an individual’s condition is unstable or high-risk, such as severe heart failure or active infection, CABG may be deferred or alternative treatments may be considered.
Unsuitable anatomy: In some cases, the anatomy of the coronary arteries may not be suitable for CABG. For example, if the coronary arteries are too small or have diffuse disease, other treatment options like percutaneous coronary intervention (PCI) may be more appropriate.
Patient preference: Ultimately, the decision to undergo CABG should involve the patient’s preferences, values, and goals of care. If a patient does not wish to undergo surgical intervention, alternative treatments or conservative management may be considered.
Advantages
Coronary Artery Bypass Grafting (CABG) surgery can be beneficial for certain individuals with coronary artery disease (CAD). Here are some advantages of CABG:
Improved blood flow: CABG creates new pathways for blood to flow around blocked or narrowed coronary arteries, improving blood flow to the heart muscle. This can relieve symptoms such as chest pain (angina) and improve overall heart function.
Symptom relief: Many patients experience significant improvement or complete relief of angina symptoms after CABG surgery. This can enhance their quality of life and allow them to engage in activities they were previously limited in due to chest pain.
Long-term benefits: Studies have shown that CABG surgery can provide long-term benefits for patients with coronary artery disease. It has been associated with improved survival rates and reduced risk of future cardiovascular events compared to medical therapy alone.
Durability: The grafts used in CABG, such as the internal mammary artery or saphenous vein, can provide durable and long-lasting results. These grafts can remain open and functional for many years, allowing for sustained improvement in blood flow to the heart.
Potential for complete revascularization: CABG allows for complete revascularization, meaning that multiple blocked or narrowed coronary arteries can be bypassed during the procedure. This comprehensive approach can restore blood flow to multiple areas of the heart, improving overall cardiac function.
Lower risk of repeat procedures: Compared to other treatments such as percutaneous coronary intervention (PCI), CABG has been associated with a lower risk of needing repeat procedures or interventions in the future.
Complications
While Coronary Artery Bypass Grafting (CABG) surgery is generally safe and effective, like any surgical procedure, it carries some risks and potential complications. It’s important to be aware of these potential complications, although they occur infrequently. Some of the possible complications of CABG surgery include:
- Infection: There is a risk of developing an infection at the site of the surgical incision or in the chest cavity. Infections can be treated with antibiotics, but in some cases, additional procedures may be required to drain the infected area.
- Bleeding: During and after CABG surgery, there is a risk of bleeding. The surgical team takes precautions to minimize bleeding, but in some cases, blood transfusions or additional surgical interventions may be necessary to control bleeding.
- Blood Clots: Blood clots can form in the legs (deep vein thrombosis) or lungs (pulmonary embolism) after surgery. Medications and compression devices are used to prevent blood clots, but in some cases, additional treatment may be required.
- Stroke: There is a small risk of stroke during or after CABG surgery. This can occur due to blood clots, air bubbles, or other factors. The risk is generally low, but it is higher in individuals with pre-existing risk factors for stroke.
- Irregular Heart Rhythms: CABG surgery can sometimes cause irregular heart rhythms, such as atrial fibrillation. In most cases, these irregularities resolve on their own, but medications or other interventions may be needed to manage them.
- Lung Problems: After CABG surgery, some individuals may experience lung-related complications, such as pneumonia or fluid accumulation in the lungs. Breathing exercises, early mobilization, and respiratory support can help prevent and manage these complications.
- Kidney Problems: CABG surgery can occasionally lead to temporary or permanent kidney problems, particularly in individuals with pre-existing kidney disease or other risk factors. Close monitoring and appropriate management are important to minimize the risk of kidney complications.
- Wound Healing Issues: Some individuals may experience delayed wound healing or infection at the surgical incision site. Proper wound care and follow-up with healthcare professionals can help prevent and manage these issues.
- Graft Failure or Blockage: Over time, the bypass grafts used during CABG surgery can develop blockages or fail to function properly. This can lead to recurrent symptoms or the need for additional interventions, such as angioplasty or repeat CABG surgery.
Previous care
Preoperative Evaluation: Before undergoing CABG surgery, a thorough preoperative evaluation is conducted. This includes a review of the patient’s medical history, physical examination, and various tests such as blood tests, electrocardiogram (ECG), echocardiogram, and coronary angiography. These evaluations help assess the severity of coronary artery disease, identify any associated conditions, and determine the suitability for surgery.
Medication Management: Prior to surgery, medications may be prescribed or adjusted to optimize the patient’s condition. This may include medications to control blood pressure, manage cholesterol levels, prevent blood clots, and stabilize heart function.
Preparation for Surgery: In the days leading up to the surgery, patients are given instructions on fasting, medication management, and other preoperative preparations. They may be advised to stop certain medications, refrain from eating or drinking for a specific period of time, and follow specific hygiene protocols.
Anesthesia: CABG surgery is performed under general anesthesia, which means the patient is unconscious and pain-free during the procedure. An anesthesiologist administers the anesthesia and monitors the patient’s vital signs throughout the surgery.
Surgical Procedure: During the surgery, the surgeon makes an incision in the chest to access the heart. The patient is connected to a heart-lung bypass machine, which takes over the function of the heart and lungs during the procedure. The surgeon then takes a healthy blood vessel, often from the chest or leg, and attaches it to the blocked coronary artery, bypassing the blockage and restoring blood flow to the heart muscle. The number of grafts performed depends on the extent of coronary artery disease.
Postoperative Care: After the surgery, the patient is transferred to the intensive care unit (ICU) for close monitoring. They are connected to various monitors to track vital signs, heart function, and oxygen levels. Pain management, wound care, and prevention of complications such as infection and blood clots are important aspects of postoperative care. Gradually, the patient is transitioned to a regular hospital room and then discharged with specific instructions for recovery, medication management, and follow-up appointments.
Aftercare
Aftercare following Coronary Artery Bypass Grafting (CABG) surgery is an essential part of the recovery process. Here are some key aspects of aftercare:
Hospital Stay: After CABG surgery, patients typically stay in the hospital for a few days. The length of the hospital stay may vary depending on individual factors and the specific hospital’s protocols. During this time, medical staff closely monitor the patient’s vital signs, heart function, and overall recovery.
Pain Management: Pain management is an important aspect of aftercare. Medications are prescribed to help manage pain and discomfort following surgery. It’s important for patients to communicate their pain levels to the healthcare team to ensure appropriate pain relief.
Wound Care: Proper care of the surgical incision site is crucial to prevent infection and promote healing. Patients are instructed on how to keep the incision clean and dry, and they may need to change dressings regularly. It’s important to follow the healthcare team’s instructions regarding wound care.
Physical Activity and Rehabilitation: Gradual resumption of physical activity is an important part of aftercare. Patients are encouraged to start with light activities, such as short walks, and gradually increase their activity level as advised by the healthcare team



Reviews
There are no reviews yet.