Description
Familiarity with Treatment
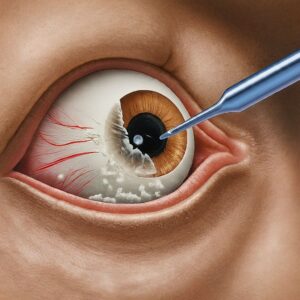
A cystectomy is a surgical procedure to remove all or part of the bladder. It is primarily used to treat bladder cancer but can also be indicated for other conditions such as severe bladder dysfunction or trauma.
Procedure
- Preparation: The patient undergoes preoperative assessments, including imaging studies and lab tests.
- Anesthesia: General anesthesia is administered to ensure the patient is unconscious and pain-free.
- Surgery:
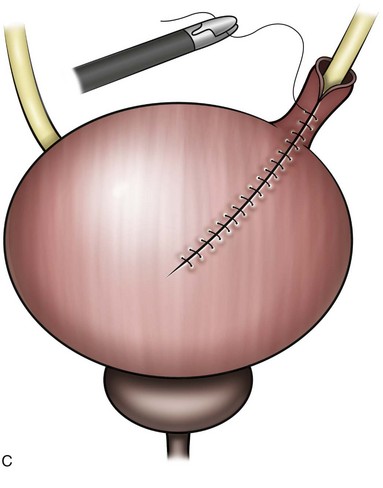
- Partial Cystectomy: Only a portion of the bladder is removed.
- Radical Cystectomy: The entire bladder is removed, often along with nearby lymph nodes and organs that may contain cancer cells (e.g., prostate in men, uterus in women).
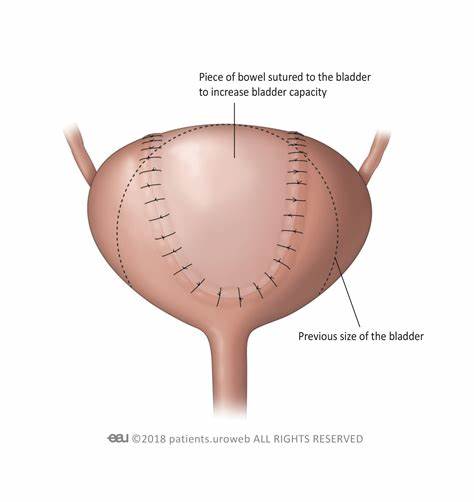
- Reconstruction: After bladder removal, the surgeon creates a new way for urine to exit the body, such as a urostomy or a neobladder.
Who is it Suitable For?
- Patients with muscle-invasive bladder cancer.
- Individuals with high-grade non-muscle-invasive bladder cancer that has not responded to other treatments.
- Patients with severe bladder dysfunction or trauma.
Who is it Not Suitable For?
- Patients with poor overall health or significant comorbidities that increase surgical risk.
- Individuals with non-invasive bladder cancer that can be managed with less invasive treatments.
Advantages
- Effective Cancer Control: Removes the primary site of cancer, reducing the risk of spread.
- Symptom Relief: Alleviates symptoms caused by bladder dysfunction or trauma.
- Potential for Cure: Offers a chance for long-term survival in patients with localized bladder cancer.
Complications
- Infection: Risk of postoperative infections.
- Bleeding: Potential for significant blood loss during surgery.
- Urinary Issues: Problems with urine flow or incontinence.
- Sexual Dysfunction: Possible impact on sexual function, especially in radical cystectomy.
- Bowel Issues: Potential for bowel obstruction or other gastrointestinal problems.
Previous Care
- Preoperative Evaluation: Comprehensive assessment including imaging, lab tests, and consultations with specialists.
- Patient Education: Informing the patient about the procedure, risks, benefits, and postoperative care.
- Nutritional Support: Ensuring the patient is in optimal nutritional status before surgery.
Aftercare
- Hospital Stay: Typically involves a hospital stay of several days to a week.
- Pain Management: Use of medications to control postoperative pain.
- Monitoring: Regular monitoring for signs of infection, bleeding, or other complications.
- Rehabilitation: Physical therapy and exercises to aid recovery.
- Follow-Up: Regular follow-up appointments to monitor recovery and address any issues.




Reviews
There are no reviews yet.