Description
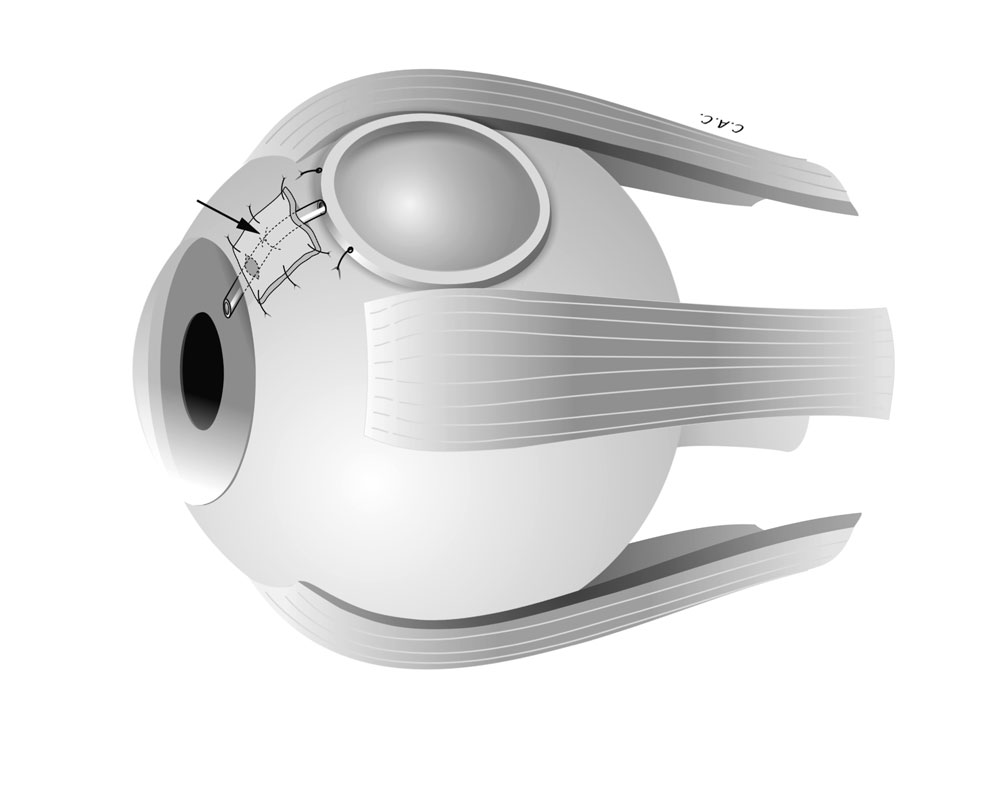
What are Glaucoma Drainage Implants?
Glaucoma drainage implants are tiny prosthetic devices implanted in the eye to regulate intraocular pressure (IOP) in glaucoma patients. Glaucoma occurs when aqueous humor, a fluid in the front of the eye, doesn’t drain properly, causing pressure buildup that damages the optic nerve. Drainage implants create a new pathway for fluid to exit the eye, lowering IOP and potentially preventing further nerve damage.
Procedure:
Glaucoma drainage implant surgery is typically performed on an outpatient basis. Anesthesia numbs the eye area, and medication relaxes the patient. A small tube is inserted into the eye, often between the cornea and iris. The tube acts as an artificial drain, channeling fluid to a plate positioned on the eye’s surface. This plate acts as a reservoir, allowing fluid to seep through and be absorbed by the body.
Suitable Candidates:
- Patients whose glaucoma is uncontrolled with eye drops or laser treatments.
- Individuals with certain glaucoma types where traditional surgery (trabeculectomy) is less effective, such as aphakic glaucoma (no lens in the eye), neovascular glaucoma (abnormal blood vessel growth), or uveitic glaucoma (inflammation).
Unsuitable Candidates:
- Patients with uncontrolled active eye infections.
- Individuals with severe anatomical abnormalities in the eye.
- People with a high risk of bleeding or scarring.
Advantages:
- Effective IOP control in some patients where other treatments fail.
- May offer a longer-term solution compared to medications.
Complications:
- Infection: The bleb (fluid collection area under the skin) is an entry point for infection, requiring prompt medical attention if redness, pain, or vision changes occur.
- Tube blockage: The drainage tube can become blocked, requiring further surgery.
- Corneal problems: The implant may irritate the cornea, causing discomfort or vision issues.
- Bleeding: Bleeding can occur during or after surgery.
- Loss of vision: While rare, there’s a slight risk of vision loss associated with any eye surgery.
Preoperative Care:
- A comprehensive eye exam to assess suitability.
- Discussion of risks and benefits with your ophthalmologist.
- Medications to prevent infection may be prescribed.
- Stopping certain medications that could increase bleeding risk.
Postoperative Care:
- Eye drops to prevent infection and inflammation.
- Regular follow-up appointments to monitor IOP and check for complications.
- Avoiding strenuous activities that could strain the eye.


Reviews
There are no reviews yet.