Description
Familiarity with Treatment
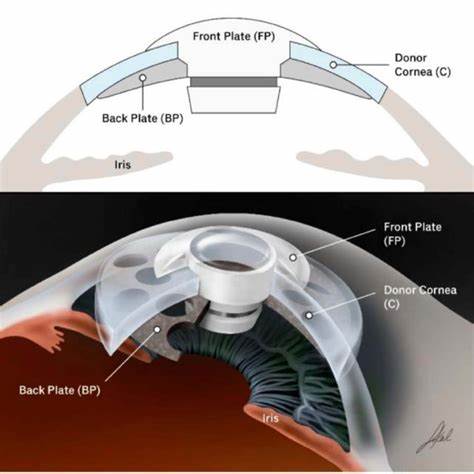
Keratoprosthetics involves the use of an artificial cornea (keratoprosthesis) to replace a damaged or diseased cornea. This procedure is often used when traditional corneal transplants are not viable. The femto-graft technique utilizes a femtosecond laser to prepare both the donor and recipient tissues, allowing for precise and customized cuts.
Procedure Explanation
- Anesthesia:
- Local or general anesthesia is administered to numb the eye.
- Preparation of Donor and Recipient Tissue:
- A femtosecond laser is used to create precise cuts in both the donor corneal tissue and the recipient’s cornea.
- Placement of Keratoprosthesis:
- The artificial cornea is placed into the prepared site on the recipient’s eye.
- The donor tissue is then grafted around the keratoprosthesis to secure it in place.
- Stitching:
- Fine sutures are used to secure the graft and keratoprosthesis in place.
- Post-Surgery:
- The eye is covered with a protective shield to aid healing.
Who is it Suitable For?
- Patients with severe corneal diseases not amenable to traditional corneal transplantation.
- Individuals with conditions such as severe chemical burns, ocular cicatricial pemphigoid, or multiple failed corneal transplants.
- Patients with severe corneal scarring or opacification.
Who is it Not Suitable For?
- Patients with active eye infections or severe inflammation.
- Individuals with conditions that may affect healing, such as uncontrolled diabetes.
- Patients who are not suitable candidates for surgery due to other health conditions.
Advantages
- Vision Restoration: Can significantly improve vision in patients with severe corneal damage.
- Precision: The femtosecond laser allows for highly precise cuts, improving the fit and integration of the graft.
- Durability: The keratoprosthesis provides a long-lasting solution for corneal blindness.
- Reduced Rejection: Lower risk of rejection compared to traditional corneal transplants.
Complications
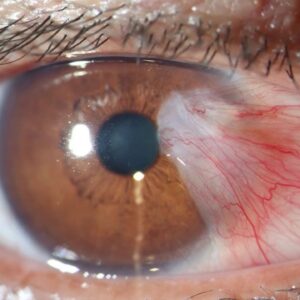
- Rejection: Although reduced, there is still a risk of the body rejecting the graft.
- Infection: Risk of postoperative infection.
- Glaucoma: Increased intraocular pressure.
- Graft Failure: The transplanted tissue may fail over time.
- Vision Changes: Possible temporary or permanent changes in vision.
Previous Care
- Preoperative Assessment: Comprehensive eye examination and measurements.
- Medication Review: Adjustments to current medications, especially those affecting healing.
- Health Evaluation: General health check to ensure suitability for surgery.
Aftercare
- Medications: Use prescribed eye drops to prevent infection and control inflammation.
- Follow-Up Visits: Regular check-ups to monitor healing and detect any complications.
- Activity Restrictions: Avoid strenuous activities and protect the eye from injury.
- Vision Monitoring: Report any changes in vision or discomfort to your ophthalmologist immediately.




Reviews
There are no reviews yet.