Description
Keratoprosthesis: A Vision of Hope for Eyes with Severe Corneal Damage
Treatment Familiarity:
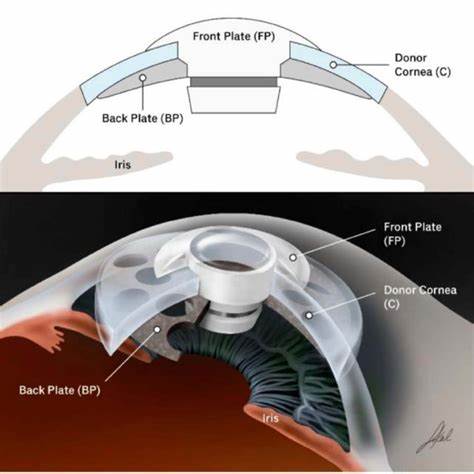
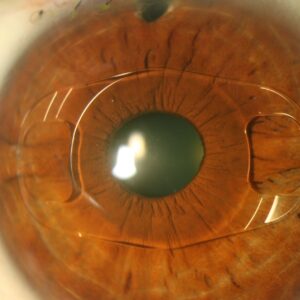
Keratoprosthesis, also known as artificial corneal implant, is a complex surgical procedure reserved for individuals with severe corneal damage where traditional corneal transplantation (keratoplasty) is not a viable option. It involves implanting an artificial cornea made of synthetic materials to restore vision. This is a relatively uncommon procedure compared to traditional corneal transplants.
Procedure Breakdown:
The specific type of keratoprosthesis implant and surgical approach vary depending on the nature and severity of the corneal damage. Here’s a general overview:
- Anesthesia: General anesthesia is typically used to keep the patient unconscious during surgery.
- Recipient Corneal Preparation: The surgeon removes the damaged corneal tissue to create a space for the implant.
- Implant Placement: The chosen keratoprosthesis is carefully positioned and secured to the surrounding eye structures.
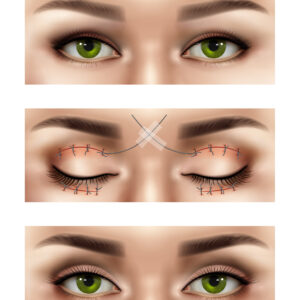
- Closure: The surgical site is meticulously sutured (stitched) closed.
Suitable Candidates:
Keratoprosthesis is considered a last-resort option for individuals with:
- Failed Corneal Transplants: Multiple rejections of donor corneas in traditional transplant surgeries.
- Severe Corneal Scarring: Extensive scarring that makes a traditional corneal transplant technically difficult or unlikely to succeed.
- Corneal Deformities: Significant abnormalities in the corneal shape that traditional transplants cannot address.
Who Might Not Be a Candidate?
Keratoprosthesis is not suitable for everyone. It’s generally not recommended for:
- Individuals with active eye infections: Infection increases surgical risk and can lead to implant failure.
- People with uncontrolled medical conditions: Severe health problems that could increase surgical risk may make someone a poor candidate.
- Patients with unrealistic expectations: Keratoprosthesis has a higher complication rate than traditional transplants, and vision restoration may not be complete.
Advantages of Keratoprosthesis:
- Potential for Vision Restoration: In successful cases, keratoprosthesis can offer sight restoration for individuals with severely damaged corneas who cannot benefit from traditional transplants.
- Advanced Technology: Newer keratoprosthesis designs offer improved biocompatibility and potentially better long-term outcomes.
Potential Complications:
- Rejection: The body’s immune system may react to the artificial implant, leading to rejection and implant failure.
- Infection: Although uncommon, infection is a serious complication requiring prompt antibiotic treatment and potentially removal of the implant.
- Glaucoma: Increased pressure within the eye can develop after surgery and require medication or additional surgery.
- Endophthalmitis: Infection within the inner eye can be a devastating complication.
- Vision Changes: Temporary blurred vision or fluctuations in vision are common after surgery. Vision restoration may not be complete.
Preoperative Care:
- Comprehensive eye exam to assess the severity of corneal damage and overall eye health.
- Detailed discussion of risks and benefits of keratoprosthesis with your ophthalmologist. This will involve a realistic discussion of potential outcomes and the higher complication rate compared to traditional transplants.
- Medical evaluation to ensure you can undergo surgery safely.
- Extensive testing to assess the risk of implant rejection.
Postoperative Care:
- Intensive eye drop regimen to prevent infection and inflammation.
- Wearing an eye patch or shield for a prolonged period to protect the surgical site and the implant.
- Anti-rejection medications may be used to suppress the immune system’s response to the implant.
- Regular follow-up appointments with your ophthalmologist are crucial to monitor healing, vision improvement, address any concerns, and detect potential complications early.




Reviews
There are no reviews yet.