Description
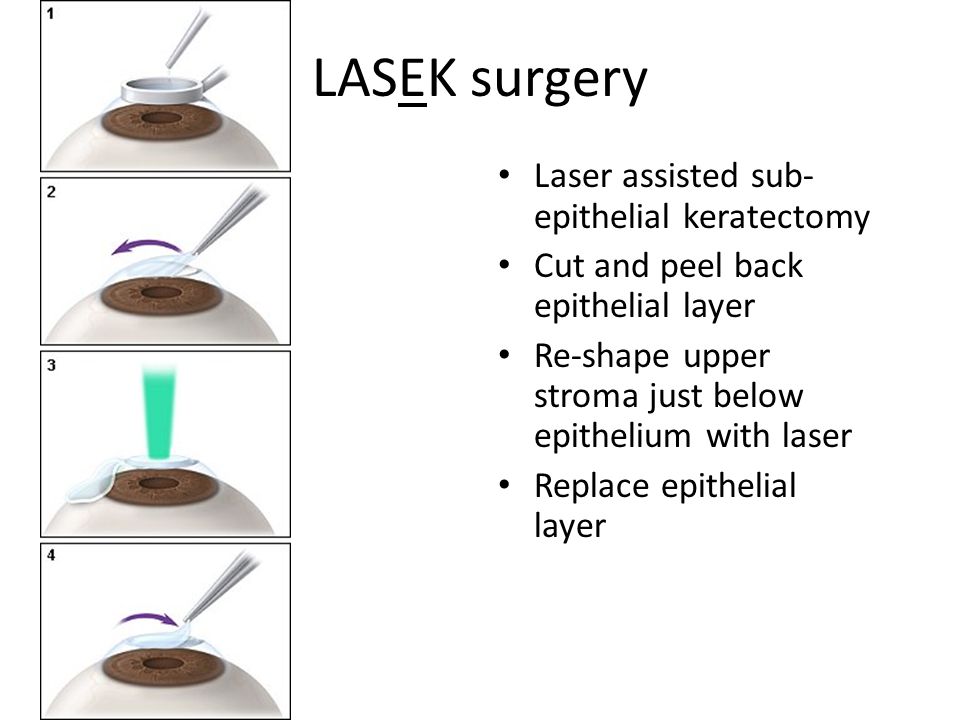
LASEK (Laser Epithelial Keratomileusis): A Hybrid Approach to Corneal Reshaping
Treatment Familiarity:
LASEK (Laser Epithelial Keratomileusis) is a type of laser vision correction surgery that combines elements of PRK (photorefractive keratectomy) and LASIK (laser-assisted in situ keratomileusis). It utilizes a laser to reshape the cornea, the clear dome at the front of the eye, to correct refractive errors like nearsightedness (myopia), farsightedness (hyperopia), and astigmatism. However, unlike LASIK, LASEK avoids creating a permanent corneal flap.
Procedure Breakdown:
LASEK is typically performed on an outpatient basis:
- Anesthesia: Numbing eye drops are used to anesthetize the eye.
- Epithelial Loosening: A diluted alcohol solution is applied to loosen the surface layer of the cornea (epithelium).
- Epithelial Removal: The loosened epithelium is gently lifted and folded back like a hinge, similar to creating a thin flap.
- Laser Ablation: An excimer laser reshapes the underlying corneal tissue based on pre-measured corneal topography to correct the refractive error.
- Epithelial Repositioning: The loosened epithelium is carefully repositioned back onto the cornea and allowed to heal naturally.
- Bandage Contact Lens: A protective bandage contact lens is placed over the cornea to promote healing and reduce discomfort.
Suitable Candidates:
LASEK might be considered for individuals with:
- Stable Vision Prescription: Similar to LASIK and PRK, your eyeglass prescription should be stable for at least a year.
- Mild to Moderate Refractive Errors: LASEK is effective for correcting mild to moderate degrees of nearsightedness, farsightedness, and astigmatism.
- Concerns About LASIK Flaps: Individuals who hesitate about the creation of a permanent corneal flap in LASIK may find LASEK appealing.
- Corneas Thin for LASIK: While not ideal for everyone with thin corneas, LASEK may be a possibility in some cases where LASIK is not recommended due to insufficient corneal thickness.
Who Might Not Be a Candidate?
LASEK is not suitable for everyone. It’s generally not recommended for:
- People with Dry Eyes: LASEK can worsen pre-existing dry eye symptoms.
- Pregnant or Nursing Women: Hormonal changes can affect vision stability.
- Patients with Certain Medical Conditions: Autoimmune diseases or uncontrolled chronic conditions may increase surgical risks.
- Individuals with Active Eye Infections: Infections need to be resolved before LASEK can be considered.
Advantages of LASEK:
- Potential for Faster Healing: Compared to PRK, LASEK may offer slightly faster healing due to the preservation of the epithelial basement membrane.
- Reduced Risk of Flap Complications: LASEK avoids the creation of a permanent corneal flap, potentially reducing the risk of flap-related complications seen in LASIK.
- Possible Option for Thinner Corneas: In some cases, LASEK may be a viable alternative for individuals with corneas that are too thin for LASIK.
Potential Complications:
- Epithelial Ingrowth: There’s a small chance that some epithelial cells may migrate beneath the corneal surface after surgery, requiring additional treatment.
- Slower Recovery than LASIK: While potentially faster than PRK, LASEK recovery may be slightly slower than LASIK due to the manipulation of the epithelium.
- Dry Eyes: Temporary or chronic dry eye symptoms can develop after LASEK.
- Undercorrection or Overcorrection: There’s a slight chance that the laser treatment may not fully correct the refractive error, requiring an enhancement procedure.
- Infection: Although rare, infection is a serious complication requiring prompt antibiotic treatment.
Preoperative Care:
- Comprehensive eye exam to assess your corneal health, measure your refractive error, and determine your candidacy for LASEK.
- Detailed discussion of risks and benefits of LASEK with your ophthalmologist.
- Mapping of the corneal surface (topography) to guide the laser treatment.
- Stopping certain medications that may affect corneal healing (consult your ophthalmologist).
Postoperative Care:
- Eye drops or ointment to prevent infection and inflammation.
- Wearing a bandage contact lens for a few days to protect the healing epithelium.
- Avoiding strenuous activity or rubbing your eyes for a certain period.
- Pain medication may be prescribed for initial discomfort.
- Regular follow-up appointments with your ophthalmologist to monitor healing, vision improvement, and address any concerns.


Reviews
There are no reviews yet.