Description
Treatment Familiarity:
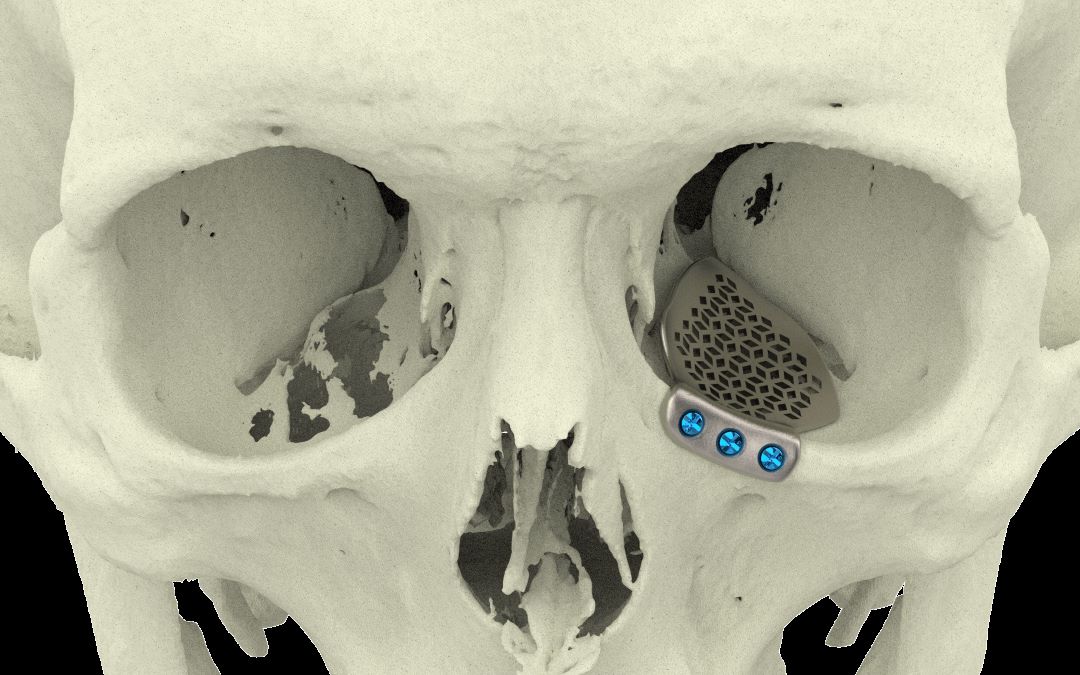
Orbital reconstruction is a specialized surgical procedure performed by ophthalmic plastic surgeons (ophthalmologists with additional training in eyelid, tear duct, and orbital surgery). It aims to restore the shape and function of the bony socket surrounding the eye (orbit) after trauma, tumors, or congenital malformations.
Procedure Breakdown:
The specific approach for orbital reconstruction depends on the extent and nature of the damage. Here’s a general overview:
- Anesthesia: General anesthesia is typically used to keep the patient unconscious during surgery.
- Access: The surgeon creates an incision based on the location and type of reconstruction needed. This might involve accessing the orbit through the eyelid, conjunctiva (white part of the eye), or a facial incision.
- Repair or Reconstruction: Several techniques may be employed:
- Bone Grafting: If bone is missing, grafts from other parts of the skull or synthetic materials can be used to rebuild the orbital walls. Plates and screws may be used for additional support.
- Orbital Implants: Pre-fabricated implants made of plastic or biocompatible materials can be used to replace missing orbital structures.
- Fat Grafting: In some cases, fat grafting can be used to improve the contour and support of the eye.
- Muscle Reattachment: Eye muscles that have been detached or damaged may be reattached to their proper positions to restore eye movement.
- Closure: The surgical site is meticulously sutured (stitched) closed.
Suitable Candidates:
Orbital reconstruction can benefit individuals with:
- Fractures of the orbital bones: Trauma to the face can cause fractures to the bones surrounding the eye. Reconstruction can restore the shape of the orbit and prevent complications like vision problems or eye movement limitations.
- Orbital Tumors: Surgery to remove an orbital tumor may require reconstruction to restore the orbital anatomy and support the eye.
- Congenital Malformations: Individuals born with underdeveloped or misshapen orbital bones can benefit from reconstruction for both functional and cosmetic reasons.
- Graves’ Ophthalmopathy: This autoimmune disease can cause enlargement and bulging of the eyes (proptosis). Orbital reconstruction can help reposition the eye and improve vision.
Who Might Not Be a Candidate?
Orbital reconstruction may not be suitable for everyone. It’s generally not recommended for:
- Individuals with severe medical conditions that could increase surgical risk.
- Patients with uncontrolled eye infections: Infection increases surgical risk.
- People with unrealistic expectations about the outcome of surgery.
Advantages of Orbital Reconstruction:
- Functional Restoration: Can restore vision, eye movement, and improve eye lubrication.
- Cosmetic Improvement: Rebuilds the shape of the orbit for a more symmetrical and aesthetically pleasing appearance.
- Preventing Complications: Reduces the risk of vision loss or other problems associated with orbital defects.
- Improved Quality of Life: Overall functional and cosmetic improvements can significantly enhance quality of life.
Potential Complications:
- Bleeding: Minor bleeding can occur during or after surgery.
- Infection: Although uncommon, infection is a potential complication requiring prompt antibiotic treatment.
- Vision Loss: In rare cases, vision loss can occur as a complication of surgery.
- Double Vision: Eye muscle dysfunction can lead to double vision, which may require additional surgery for correction.
- Numbness: Temporary numbness around the surgical site can occur.
- Asymmetry: Achieving perfect symmetry can be challenging, and some degree of asymmetry may remain.
Preoperative Care:
- Comprehensive examination by an ophthalmologist and potentially other specialists depending on the cause of the orbital defect.
- Imaging tests like CT scan or MRI scan to assess the extent of the damage to the orbit.
- Discussion of risks and benefits of orbital reconstruction with your ophthalmic plastic surgeon.
- Medical evaluation to ensure you can undergo surgery safely.
- Stopping certain medications that could increase bleeding risk.
Postoperative Care:
- Eye drops or ointment to prevent infection and inflammation.
- Wearing an eye patch or shield for a short period to protect the surgical site.
- Pain medication to manage discomfort.
- Careful monitoring of vision and eye movement.
- Regular follow-up appointments with your ophthalmic plastic surgeon to monitor healing and address any concerns.



Reviews
There are no reviews yet.