Description
Familiarity with treatment
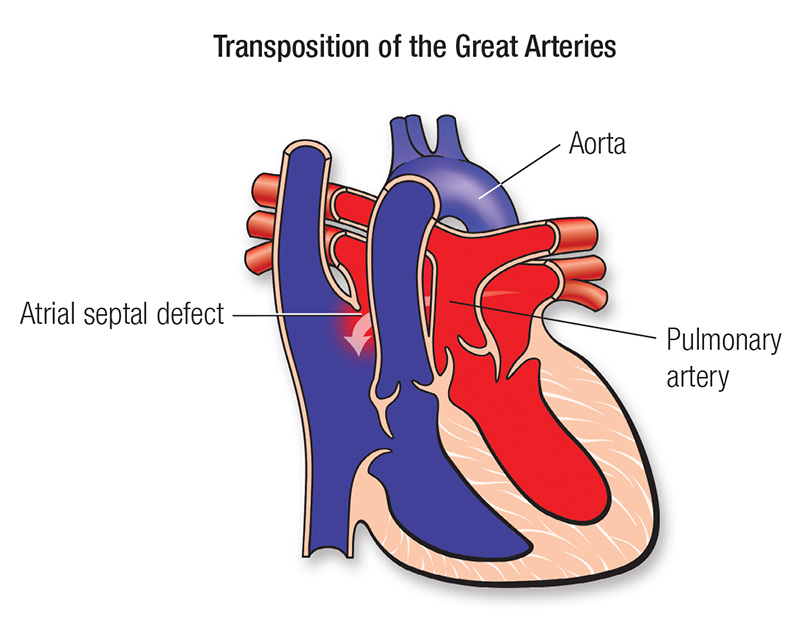
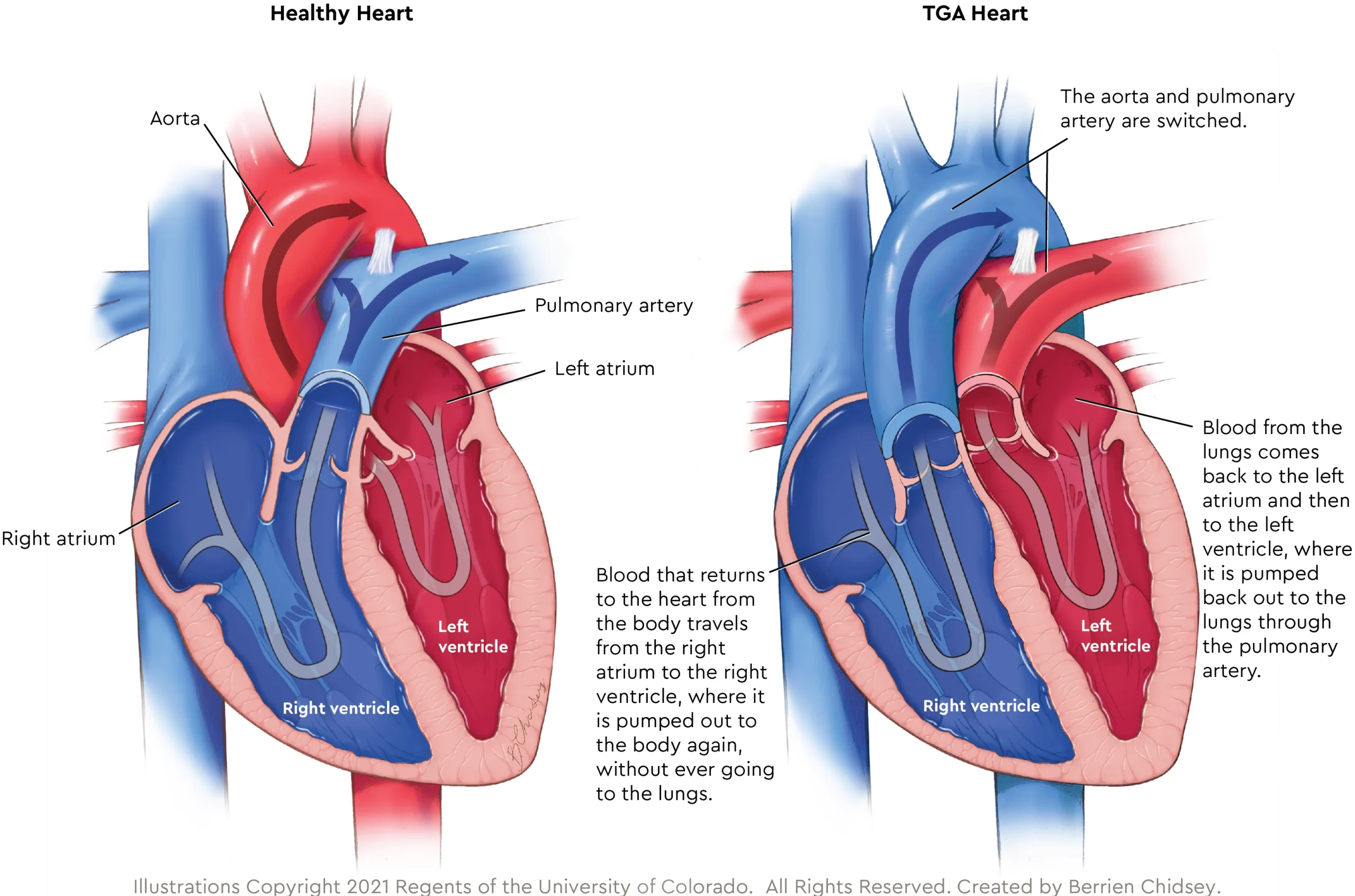
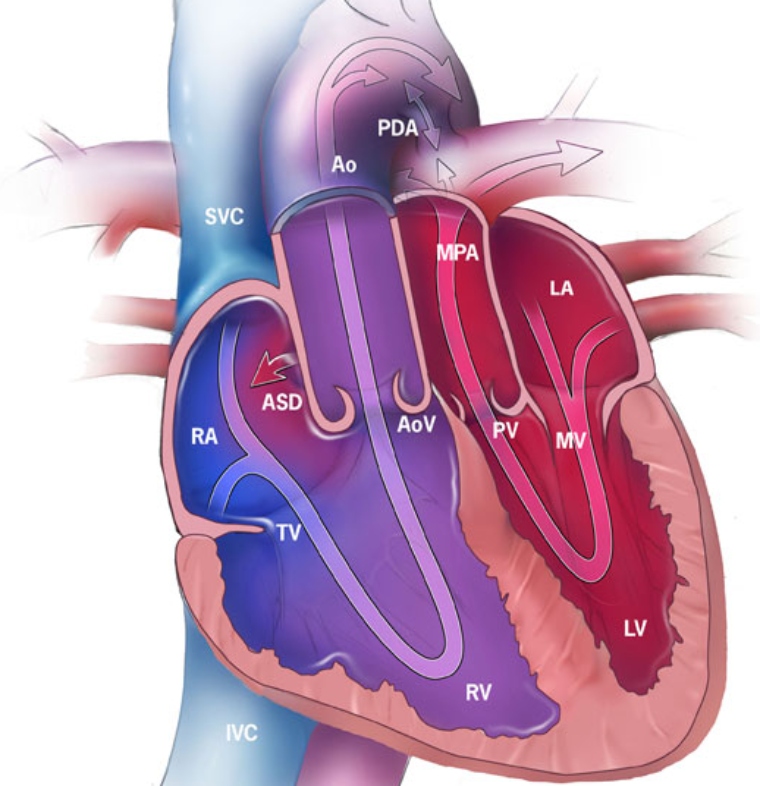
TGA is a congenital heart defect where the positions of the pulmonary artery and the aorta are switched, resulting in abnormal blood circulation. The primary treatment for TGA is surgical repair, which aims to correct the abnormal positioning of the arteries and restore normal blood flow.
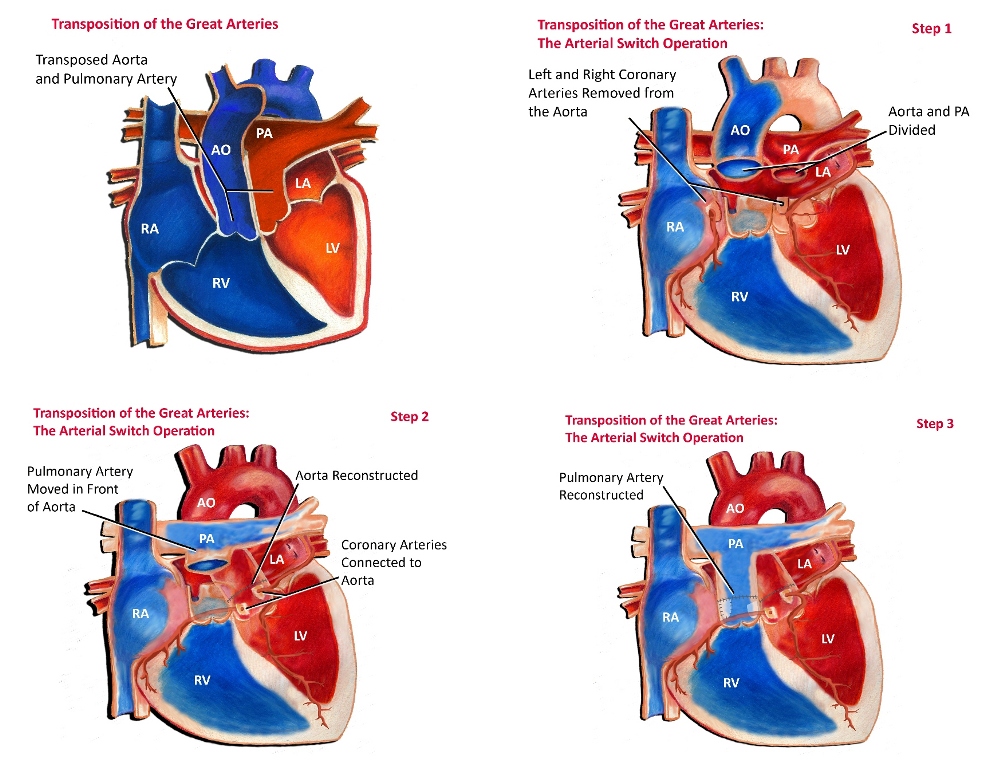
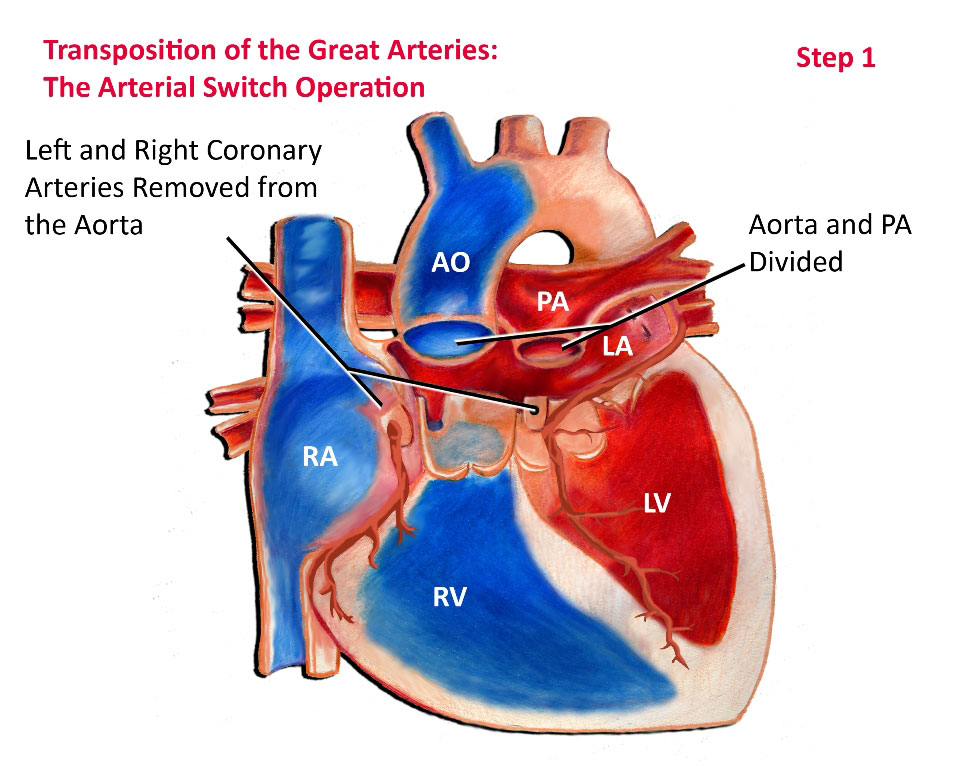
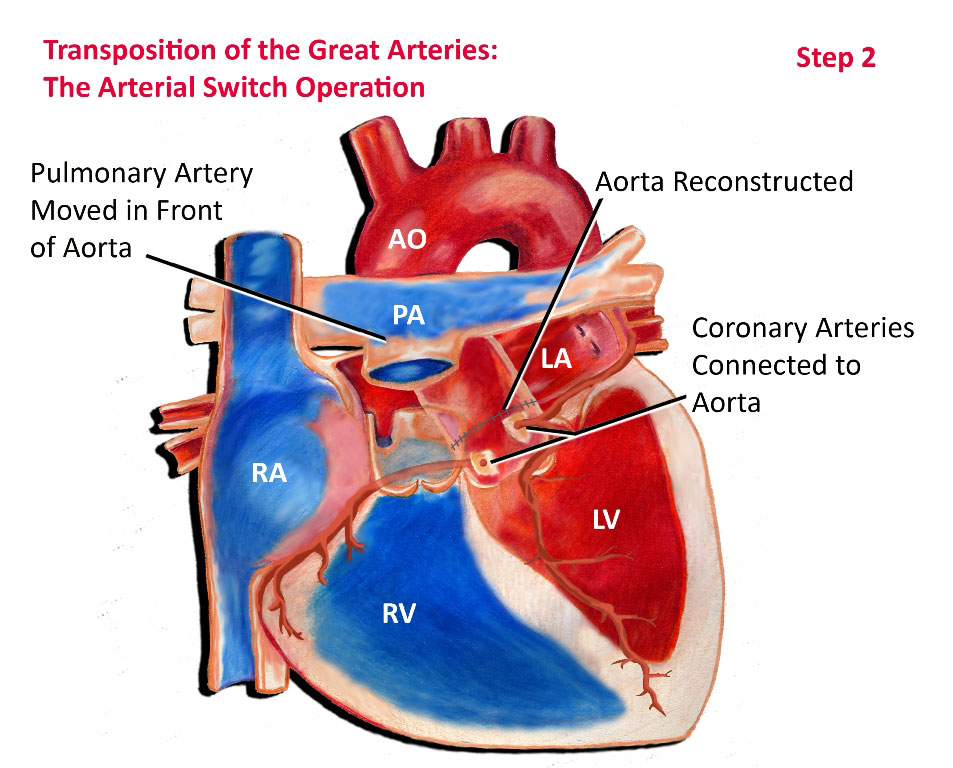
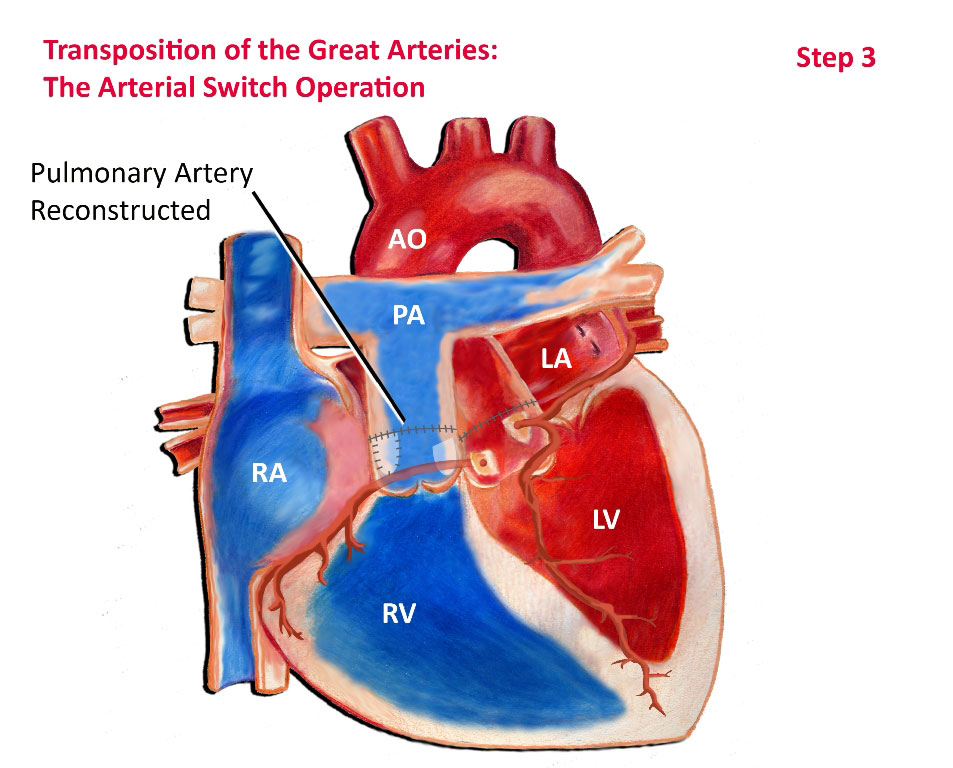
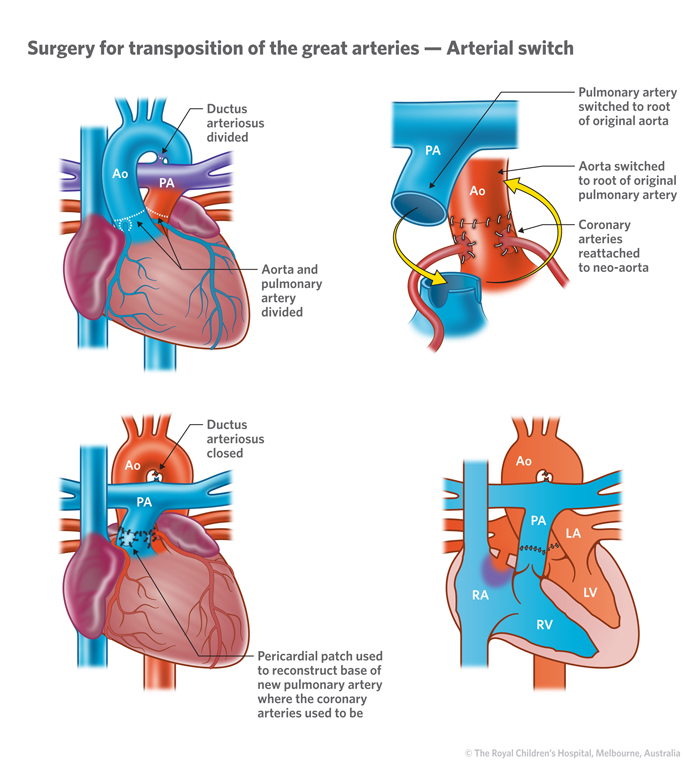
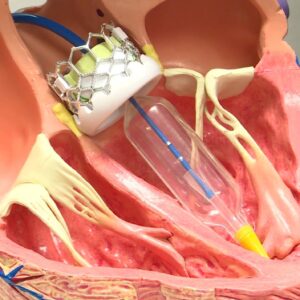
The most common surgical procedure for TGA repair is called the arterial switch operation (ASO). During this procedure, the surgeon switches the positions of the pulmonary artery and the aorta, and also reattaches the coronary arteries to the new aorta. This allows for the proper circulation of oxygenated blood to the body and deoxygenated blood to the lungs.
The ASO is typically performed in the first few weeks of life, often within the first few days after birth. The timing of the surgery depends on various factors, including the overall health of the baby and the presence of any associated heart defects.
During the surgery, the individual is placed under general anesthesia, and a heart-lung bypass machine is used to maintain circulation while the surgeon operates on the heart. The surgeon makes an incision in the chest and carefully disconnects and repositions the arteries. The coronary arteries are carefully reattached to the new aorta, ensuring proper blood supply to the heart muscle.
Who is it suitable for?
TGA repair surgery is typically suitable for infants and children diagnosed with TGA. The surgery is usually performed in the first few weeks of life, often within the first few days after birth. The timing of the surgery depends on various factors, including the overall health of the baby and the presence of any associated heart defects.
The suitability for TGA repair surgery is determined through a comprehensive evaluation by a healthcare team, including pediatric cardiologists and cardiac surgeons. They consider factors such as the severity of the TGA, the presence of any associated heart abnormalities, the overall health of the individual, and the potential risks and benefits of the surgery.
In general, individuals who are suitable for TGA repair surgery are those who are in good overall health and have a favorable prognosis for the surgery. However, each case is unique, and the suitability for surgery is determined on an individual basis.
Who is it not suitable for?
Individuals who may not be suitable for TGA repair surgery include those with severe associated heart defects or other significant medical conditions that pose a high risk for surgery. The decision to proceed with surgery depends on factors such as the overall health of the individual, the severity of the TGA, and the potential risks and benefits of the surgery.
In some cases, if the associated heart defects are too complex or if the individual’s overall health is compromised, alternative treatment options may be considered. These options can include palliative procedures to improve blood flow or heart function without fully correcting the TGA, or in some cases, heart transplantation may be necessary.
Advantages
Restoration of Normal Blood Flow: TGA repair surgery aims to correct the abnormal positioning of the pulmonary artery and the aorta, allowing for the proper circulation of oxygenated blood to the body and deoxygenated blood to the lungs. By restoring normal blood flow, the surgery improves overall heart function and oxygenation of the body.
Improved Quality of Life: TGA repair surgery can significantly improve the quality of life for individuals with this congenital heart defect. By correcting the abnormal circulation, the surgery helps alleviate symptoms such as fatigue, shortness of breath, and poor exercise tolerance, allowing individuals to lead more active and fulfilling lives.
Long-Term Health Benefits: Successful TGA repair surgery can lead to long-term health benefits. It reduces the risk of complications associated with untreated TGA, such as heart failure, arrhythmias, and decreased exercise capacity. It also decreases the likelihood of developing complications later in life, improving overall cardiovascular health.
Potential for Normal Development: Early TGA repair surgery, typically performed in the first few weeks of life, allows for normal development and growth of the individual. By restoring normal blood flow and oxygenation, the surgery supports healthy development and reduces the risk of developmental delays or complications.
Favorable Long-Term Outcomes: In general, TGA repair surgery has favorable long-term outcomes. Most individuals experience improved heart function, reduced symptoms, and an increased lifespan. However, it’s important to note that each case is unique, and the specific outcomes can vary depending on individual factors and any associated heart abnormalities.
Complications
Transposition of the Great Arteries (TGA) repair surgery is generally effective, but like any surgical procedure, there can be potential complications. Here are some possible complications associated with TGA repair surgery:
Heart Function and Rhythm Issues: Some individuals may experience problems with heart function or develop arrhythmias (abnormal heart rhythms) after TGA repair surgery. Medications may be required to control blood pressure, improve heart pumping, or regulate heart rhythm. In some cases, a pacemaker may be necessary to help regulate the heart’s rhythm. 1
Cyanosis: Cyanosis refers to bluish skin, lips, and nails due to inadequate oxygenation. Even after TGA repair surgery, some individuals may still experience cyanosis, especially if there are additional heart defects or complications.
Additional Surgeries: In some cases, additional surgeries may be needed after TGA repair. This can be due to the presence of other associated heart defects or complications that require further intervention.
Surgical Complications: As with any surgical procedure, there is a risk of surgical complications, such as bleeding, infection, or adverse reactions to anesthesia. However, these complications are relatively rare and can be managed by the healthcare team. It’s important to note that the specific complications and their likelihood can vary depending on individual factors, the presence of associated heart defects, and the overall health of the individual. The healthcare team will closely monitor the individual after surgery and provide appropriate care to manage any complications that may arise.
Previous care
Preoperative Care: Before TGA repair surgery, infants may receive medical care to maintain ductal patency with continuous intravenous prostaglandin E1 (PgE1) infusion. This helps promote pulmonary blood flow and increase left-to-right intercirculatory mixing.
Surgical Procedure: The most common surgical approach for TGA repair is the arterial switch operation. This procedure involves reattaching the aorta to the left ventricle and the pulmonary artery to the right ventricle, restoring normal blood flow. The surgery requires extensive experience with the anomaly and is typically performed within a few days of birth.
Intraoperative Care: During the surgery, careful attention is given to the coronary arteries to ensure they are not damaged or distorted. The size and delicate nature of the coronary arteries pose a technical challenge during the procedure.
Aftercare
Postoperative Monitoring: After TGA repair surgery, patients are closely monitored in the intensive care unit (ICU). The healthcare team checks for any signs of bleeding or distortion in the coronary arteries. The patient’s chest is usually closed, and extubation (removal of the breathing tube) may occur within the first 24 hours.
Medications: Some individuals may require medications to manage heart function and rhythm issues. These medications can help control blood pressure, improve heart pumping, regulate heart rhythm, and address arrhythmias. In some cases, a pacemaker may be necessary to help regulate the heart’s rhythm.
Long-Term Follow-Up: Regular follow-up visits with healthcare professionals, such as pediatric cardiologists or cardiac surgeons, are crucial for monitoring heart function, addressing potential complications, and ensuring ongoing care. These visits may include imaging tests, such as echocardiograms, to assess heart structure and function.
Potential Complications: While TGA repair surgery is generally successful, some individuals may still experience complications. These can include heart function issues, arrhythmias, or cyanosis (bluish skin, lips, and nails). Additional surgeries or interventions may be necessary in some cases.
Lifestyle Considerations: Individuals who have undergone TGA repair surgery may need to make certain lifestyle adjustments. This can include regular physical activity, a heart-healthy diet, and adherence to any prescribed medications or treatments. It’s important to discuss specific lifestyle considerations with the healthcare team.




Reviews
There are no reviews yet.