Description
Familiarity with treatment
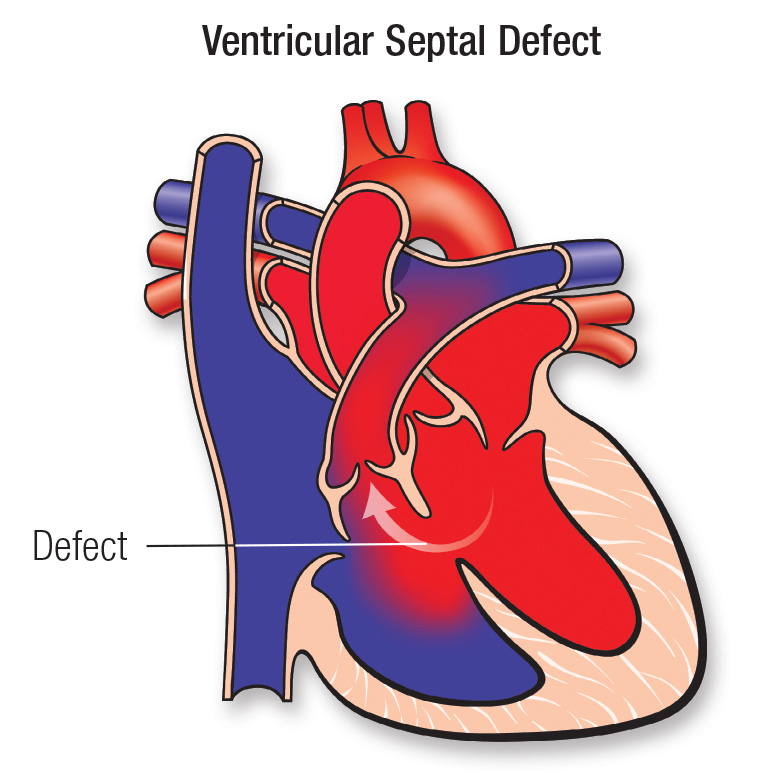
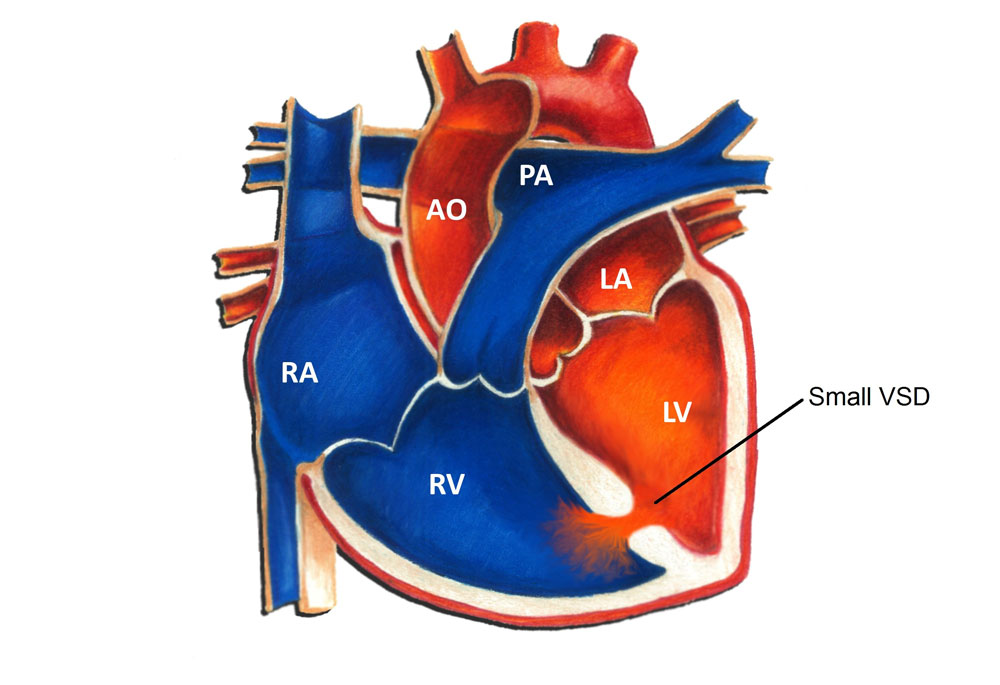
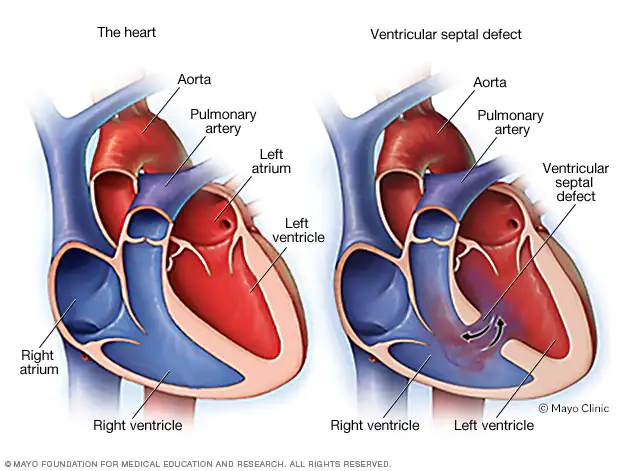
Ventricular Septal Defect (VSD) repair surgery is a procedure performed to close a hole in the wall (septum) between the two lower chambers (ventricles) of the heart. The goal of the surgery is to prevent the flow of oxygenated and deoxygenated blood between the ventricles, allowing the heart to function more efficiently.
Here are some key points about VSD repair surgery:
Surgical Approaches: VSD repair surgery can be performed using different approaches, including open-heart surgery or minimally invasive techniques. The choice of approach depends on various factors, such as the size and location of the defect, the individual’s overall health, and the surgeon’s expertise.
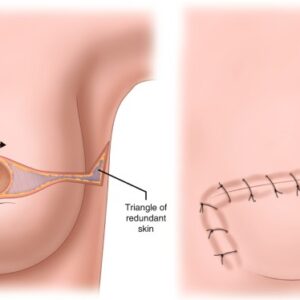
Closure Techniques: There are different techniques used to close the VSD during surgery. These can include direct suture closure, patch closure (using a synthetic material or the patient’s own tissue), or device closure (using a device inserted through a catheter).
Anesthesia: VSD repair surgery is typically performed under general anesthesia, which means the individual is asleep and pain-free during the procedure.
Hospital Stay: The length of the hospital stay following VSD repair surgery can vary depending on the individual’s condition and the specific surgical approach used. It may range from a few days to a week or more.
Recovery and Aftercare: After surgery, the individual will require a period of recovery and healing. The healthcare team will provide instructions on wound care, pain management, physical activity restrictions, and follow-up appointments.
Potential Risks and Complications: As with any surgical procedure, VSD repair surgery carries some risks. These can include bleeding, infection, adverse reactions to anesthesia, abnormal heart rhythms, residual VSD, or damage to surrounding structures. The specific risks and complications can vary depending on individual factors.
Who is it suitable for?
Ventricular Septal Defect (VSD) repair surgery may be suitable for individuals who meet certain criteria, although the specific suitability for surgery is determined on a case-by-case basis by healthcare professionals. Here are some general considerations for suitability:
Size and Location of the VSD: The size and location of the VSD play a significant role in determining suitability for surgery. Larger defects or those located in critical areas of the heart may require surgical intervention to prevent complications.
Symptoms and Complications: Individuals experiencing symptoms such as shortness of breath, fatigue, poor growth in infants, or signs of heart failure due to the VSD may be considered suitable candidates for surgery to alleviate these symptoms and prevent long-term complications.
Pulmonary Hypertension: The presence of pulmonary hypertension, a condition characterized by high blood pressure in the arteries of the lungs, may impact the suitability for VSD repair surgery. Severe pulmonary hypertension may require careful evaluation before surgical intervention is considered.
Overall Health and Cardiac Function: The individual’s overall health and cardiac function are important factors in determining suitability for surgery. A thorough evaluation of the heart’s structure and function, as well as the individual’s general health, is typically conducted to assess the risks and benefits of surgical intervention.
Age and Developmental Stage: The age and developmental stage of the individual can also influence the suitability for surgery. In some cases, infants or young children with significant VSDs may require early intervention to prevent complications and support normal growth and development.
Who is it not suitable for?
While Ventricular Septal Defect (VSD) repair surgery is a common treatment option for many individuals with VSD, there are certain situations where surgery may not be suitable or may be contraindicated. The decision regarding suitability for surgery is made by healthcare professionals based on a comprehensive assessment of the individual’s specific condition. Here are some factors that may indicate that VSD repair surgery is not suitable:
Small and asymptomatic VSD: If the VSD is small and not causing significant symptoms or complications, it may be monitored over time without surgical intervention. In such cases, the risks associated with surgery may outweigh the potential benefits.
Spontaneous closure: In some cases, VSDs may spontaneously close on their own as the individual grows, especially if they are small defects. If the defect shows signs of spontaneous closure, surgery may not be necessary.
Presence of other serious medical conditions: Individuals with severe comorbidities or other serious medical conditions may not be suitable candidates for VSD repair surgery. The risks associated with surgery may be higher in these cases, and the healthcare team may prioritize managing the other medical conditions.
Risk of complications: If the individual has a high risk of surgical complications due to factors such as advanced age, poor overall health, or significant lung or kidney disease, surgery may not be recommended.
Uncontrolled pulmonary hypertension: If the individual has severe and uncontrolled pulmonary hypertension (high blood pressure in the arteries of the lungs), it may increase the risks of surgery and affect the suitability for surgical intervention.
Unfavorable anatomy: In some cases, the location or characteristics of the VSD may make it technically challenging to repair surgically. The healthcare team will assess the feasibility of surgical closure based on the specific anatomy of the defect.
Individual preference: It’s important to consider the individual’s preferences and values when determining suitability for surgery. If the individual does not wish to undergo surgery or prefers a conservative approach, alternative management options may be considered.
Advantages
Ventricular Septal Defect (VSD) repair surgery offers several advantages for individuals who require intervention to close the hole in the heart. Here are some potential benefits of VSD repair surgery:
Improved Heart Function: Closing the VSD helps restore normal blood flow within the heart. By repairing the defect, the surgery aims to prevent the abnormal flow of blood between the ventricles, allowing the heart to pump more efficiently and reducing strain on the heart muscle.
Relief of Symptoms: VSD repair surgery can alleviate symptoms associated with the defect, such as shortness of breath, fatigue, poor growth in infants, and signs of heart failure. By improving blood flow and reducing the volume overload on the heart, surgery can help relieve these symptoms and improve overall well-being.
Prevention of Complications: Repairing the VSD can help prevent potential complications that may arise from the defect. These complications can include the development of pulmonary hypertension (high blood pressure in the arteries of the lungs), heart valve problems, or the risk of infective endocarditis (infection of the heart tissue).
Promotion of Normal Growth and Development: In infants and children, VSD repair surgery can support normal growth and development. By correcting the defect early, surgery can help ensure adequate oxygenation of the blood and prevent potential developmental delays or growth restrictions associated with untreated VSDs.
Reduced Long-Term Risks: Closing the VSD surgically can reduce the long-term risks associated with the defect. By preventing the abnormal flow of blood and reducing strain on the heart, surgery may help minimize the risk of complications later in life, such as heart failure, arrhythmias, or the need for additional interventions.
Complications
Ventricular Septal Defect (VSD) repair surgery, like any surgical procedure, carries potential risks and complications. While most children and individuals who undergo VSD repair surgery do well, it’s important to be aware of the possible complications. Here are some potential complications associated with VSD repair surgery:
Excess bleeding: Surgery involves incisions and manipulation of tissues, which can lead to bleeding. Although rare, excessive bleeding may require additional interventions or blood transfusions.
Infection: Infection at the surgical site or in the heart can occur after surgery. Steps are taken to minimize the risk of infection, such as administering antibiotics during and after the procedure.
Blood clot: Surgery and the use of cardiopulmonary bypass can increase the risk of blood clot formation. Blood clots can potentially lead to stroke or other complications. Medications and preventive measures are often taken to minimize this risk.
Abnormal heart rhythm: Surgery can sometimes disrupt the normal electrical pathways of the heart, leading to abnormal heart rhythms (arrhythmias). In most cases, these arrhythmias are temporary and resolve on their own, but in rare cases, additional treatment or intervention may be required.
Heart block: Heart block is a condition where the electrical signals in the heart are delayed or blocked, leading to an abnormal heart rhythm. In some cases, heart block may require the placement of a pacemaker to regulate the heart’s electrical activity.
Complications from anesthesia: Anesthesia carries its own risks, including allergic reactions, respiratory problems, or adverse reactions to medications. Anesthesia-related complications are generally rare but can occur.
Previous care
Prior to considering Ventricular Septal Defect (VSD) repair surgery, individuals with VSD may receive various forms of care, depending on the severity of their condition and associated symptoms. Here are some aspects of previous care that may be involved:
Diagnosis and Evaluation: The initial step in the management of VSD involves diagnosing the condition. This typically includes a thorough medical history review, physical examination, and diagnostic tests such as echocardiography, electrocardiogram (ECG), and possibly cardiac catheterization. These evaluations help determine the size, location, and impact of the VSD on the heart.
Monitoring and Observation: In cases where the VSD is small and not causing significant symptoms, a period of monitoring and observation may be recommended. Regular check-ups with a healthcare professional, including echocardiograms, allow for the assessment of the VSD’s progression and its impact on the heart’s function.
Medication Management: Medications may be prescribed to manage symptoms associated with VSD, particularly in cases of heart failure or pulmonary hypertension. Medications such as diuretics, ACE inhibitors, or beta-blockers can help alleviate symptoms, reduce fluid accumulation, and improve heart function.
Lifestyle Modifications: Individuals with VSD may be advised to make certain lifestyle modifications to minimize the impact of the condition. This can include maintaining a healthy diet, regular exercise (if not restricted by symptoms), and avoiding activities that may excessively strain the heart.
Infective Endocarditis Prophylaxis: Prior to surgical intervention, individuals with VSD may receive prophylactic antibiotics before dental or surgical procedures to reduce the risk of infective endocarditis, a potentially serious infection of the heart tissue.
Aftercare
After undergoing Ventricular Septal Defect (VSD) repair surgery, individuals require appropriate aftercare to ensure a smooth recovery and long-term well-being. Here are some key aspects of aftercare following VSD repair surgery:
Hospital Stay: After the surgery, individuals will typically spend a few days in the hospital for close monitoring. During this time, healthcare professionals will assess vital signs, manage pain, administer medications, and monitor for any signs of complications.
Wound Care: Proper care of the surgical incision site is essential to prevent infection and promote healing. The healthcare team will provide instructions on how to keep the incision clean and dry, and when to follow up for suture removal or wound assessment.
Medication Management: Medications may be prescribed after surgery to support the healing process and manage symptoms. These may include pain medications, antibiotics to prevent infection, and medications to support heart function, if necessary. It is important to take medications as prescribed and follow up with the healthcare team regarding any concerns or side effects.
Activity and Rest: Initially, individuals will need to limit physical activity and get plenty of rest to allow the body to heal. The healthcare team will provide guidance on gradually increasing activity levels over time. It is important to follow these instructions to avoid strain on the heart and promote a safe recovery.
Follow-up Appointments: Regular follow-up appointments with the healthcare team are crucial to monitor the healing process, assess heart function, and address any concerns or complications. These appointments may include echocardiograms, ECGs, or other diagnostic tests to evaluate the success of the surgery and ensure optimal recovery.
Lifestyle Modifications: Depending on the individual’s specific condition, the healthcare team may recommend certain lifestyle modifications to promote heart health. This can include maintaining a healthy diet, regular exercise (as advised by the healthcare team), managing stress, and avoiding tobacco smoke and excessive alcohol consumption.
Emotional Support: Recovering from surgery can be emotionally challenging. It is important to seek emotional support from loved ones, support groups, or mental health professionals, if needed. Openly discussing concerns and feelings can help in the recovery process.





Reviews
There are no reviews yet.