Description
Familiarity with treatment
Aortic dissection repair involves addressing a tear or separation in the inner layer of the aorta, the body’s main artery. This condition is considered a medical emergency, and prompt treatment is crucial to prevent potentially life-threatening complications.
Here are key points regarding aortic dissection repair:
- Surgical Intervention: Aortic dissection repair often involves surgical intervention aimed at repairing the tear in the aortic wall to prevent further propagation of the dissection and restore normal blood flow.
- Types of Repair:
- Open Surgical Repair: In some cases, open surgical repair is performed, involving a large incision in the chest or abdomen to access the aorta and directly repair the dissection.
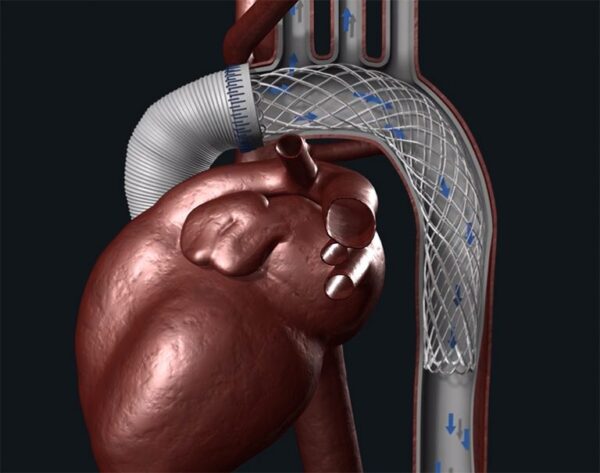
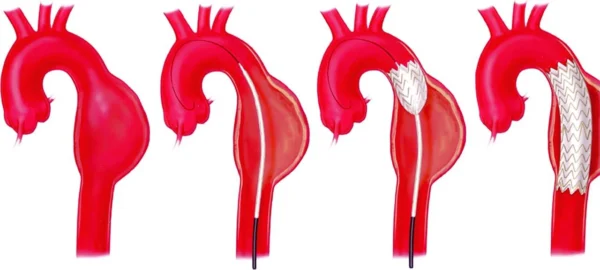
- Endovascular Repair: Endovascular techniques, such as stent grafting, may be used to treat certain types of aortic dissections. This minimally invasive approach involves inserting a stent graft into the aorta to seal off the entry and exit points of the dissection.
- Treatment Goals: The primary goals of aortic dissection repair are to prevent the dissection from worsening, restore blood flow to vital organs, and reduce the risk of complications such as aortic rupture or organ damage.
- Postoperative Care: Following aortic dissection repair, patients typically require intensive postoperative care, including close monitoring in the intensive care unit (ICU) to assess their hemodynamic status and overall condition.
- Medication Management: Patients may receive medications to control blood pressure and heart rate, as well as to reduce the risk of further dissection or complications.
- Long-Term Management: After the initial repair, long-term management may involve ongoing surveillance, medication management, and lifestyle modifications to reduce the risk of recurrent dissection or related cardiovascular complications.
- Rehabilitation and Recovery: Depending on the extent of the dissection repair and the patient’s overall health, rehabilitation and recovery may be necessary to regain strength and mobility.
It’s important to note that aortic dissection repair is a complex procedure that requires a multidisciplinary approach involving cardiovascular surgeons, interventional radiologists, anesthesiologists, and critical care specialists. The choice of repair method depends on factors such as the location and extent of the dissection, the patient’s overall health, and the expertise of the surgical team.
Who is it suitable for?
Aortic dissection repair is typically suitable for individuals who have been diagnosed with aortic dissection, a serious condition characterized by a tear in the inner layer of the aorta. The suitability for aortic dissection repair is determined based on several factors, including the type and extent of the dissection, the patient’s overall health, and the expertise of the medical team. Here are some key considerations regarding the suitability for aortic dissection repair:
- Type of Dissection:
- The type and location of the aortic dissection play a crucial role in determining the most suitable treatment approach. The extent of the dissection, including whether it involves the ascending aorta, aortic arch, descending aorta, or abdominal aorta, influences the choice of repair method.
- Acute Aortic Dissection:
- In cases of acute aortic dissection, prompt surgical intervention is often necessary to prevent further propagation of the dissection and reduce the risk of life-threatening complications, making surgical repair suitable for many patients in this category.
- Chronic Aortic Dissection:
- Patients with chronic or stable aortic dissection may be managed through careful monitoring and medical therapy. However, some individuals with chronic dissections may still require surgical intervention based on specific clinical considerations.
- Overall Health Status:
- The patient’s overall health, including cardiovascular function, respiratory status, and other medical conditions, is an important factor in determining suitability for aortic dissection repair. Patients with significant comorbidities may require a thorough evaluation to assess the risks and benefits of surgical intervention.
- Risk of Complications:
- The risk of complications associated with aortic dissection, such as aortic rupture, organ malperfusion, or progression of the dissection, may influence the decision to pursue surgical repair.
- Anatomical Considerations:
- The anatomical features of the aortic dissection, including the size, location, and involvement of branch vessels, are carefully evaluated to determine the most appropriate treatment strategy.
- Patient Preferences:
- Patient preferences and values are important considerations in the decision-making process. Shared decision-making between patients and their healthcare providers is essential in determining the most suitable approach for aortic dissection repair.
Who is it not suitable for?
Aortic dissection repair may not be suitable for certain individuals based on specific clinical considerations. While the determination of suitability for aortic dissection repair is highly individualized and requires a comprehensive evaluation by a multidisciplinary team of cardiovascular specialists, there are some general factors that may influence the decision not to pursue surgical intervention. Here are some scenarios in which aortic dissection repair may not be suitable:
- Advanced Age and Frailty:
- For elderly individuals or those with significant frailty and compromised overall health, the risks associated with surgical intervention may outweigh the potential benefits. In such cases, conservative management and palliative care may be considered.
- Extensive Comorbidities:
- Patients with extensive comorbid conditions, such as severe respiratory insufficiency, end-stage renal disease, or advanced malignancies, may not be suitable candidates for aortic dissection repair due to the increased perioperative risks and limited life expectancy.
- Uncontrolled Hemodynamic Instability:
- Individuals with uncontrolled hemodynamic instability, severe multiorgan failure, or profound shock may not be suitable for immediate surgical intervention. Stabilization and medical management are prioritized in these critical scenarios.
- Extensive Dissection Involvement:
- In cases where the aortic dissection involves extensive portions of the aorta, multiple organ malperfusion, or complex anatomical considerations that pose high surgical risks, the feasibility and benefit of repair may be limited.
- Patient Preferences and Values:
- Patient preferences, values, and goals of care play a significant role in decision-making. Individuals who express a clear preference for conservative, non-surgical management, or those who prioritize quality of life over aggressive interventions, may not be suitable candidates for aortic dissection repair.
- Unfavorable Risk-Benefit Ratio:
- In some cases, the potential risks associated with aortic dissection repair, such as the risk of mortality, stroke, or other major complications, may outweigh the potential benefits, leading to a decision to pursue alternative management strategies.
- Limited Life Expectancy:
- For individuals with limited life expectancy due to advanced age, significant comorbidities, or end-stage diseases, the pursuit of aortic dissection repair may not align with their overall care goals.
Advantages
Aortic dissection repair, whether performed surgically or through endovascular techniques, offers several potential advantages for individuals diagnosed with aortic dissection. Some of the key advantages of aortic dissection repair include:
- Prevention of Aortic Rupture: Repairing the aortic dissection helps to prevent the risk of aortic rupture, a life-threatening complication associated with untreated dissections.
- Restoration of Blood Flow: Surgical repair aims to restore normal blood flow within the aorta, reducing the risk of organ malperfusion and related complications.
- Reduction of Long-Term Complications: By addressing the dissection, repair procedures can help reduce the risk of long-term complications, such as chronic pain, recurrent dissections, and the development of aneurysms.
- Improved Organ Function: Successful repair can lead to improved blood supply to vital organs, potentially preserving or enhancing their function.
- Prevention of Progression: Repairing the dissection can prevent its further propagation and extension into other areas of the aorta.
- Potential for Minimally Invasive Procedures: Endovascular repair techniques, such as stent grafting, offer the advantage of being minimally invasive compared to traditional open surgical approaches, potentially resulting in shorter recovery times and reduced postoperative complications.
- Individualized Approach: Aortic dissection repair can be tailored to the specific characteristics of the dissection, including its location, extent, and anatomical considerations, allowing for personalized treatment strategies.
- Improved Long-Term Outcomes: Successful repair can contribute to improved long-term outcomes, including reduced risks of recurrent dissection, aortic-related morbidity, and mortality.
- Enhanced Quality of Life: For individuals who undergo successful repair, there may be an improvement in overall quality of life, reduced symptoms, and a lower likelihood of long-term complications.
- Opportunity for Surveillance and Management: Following repair, patients can benefit from ongoing surveillance and management to monitor the repaired aorta and address any potential related issues, contributing to long-term cardiovascular health.
Complications
Aortic dissection repair, whether performed through surgical or endovascular approaches, carries the potential for various complications, some of which can be serious. It’s important for individuals considering aortic dissection repair to be aware of these potential complications. Here are some of the complications associated with aortic dissection repair:
- Stroke: Both surgical and endovascular repair procedures may pose a risk of stroke, which can result from emboli dislodging during the intervention or from manipulation of the aorta or its branches.
- Paraplegia or Paraparesis: In some cases, repair of aortic dissection, particularly those involving the descending thoracic aorta, can lead to the risk of spinal cord injury, resulting in paraplegia (paralysis of the lower extremities) or paraparesis (partial paralysis).
- Endoleak: In the context of endovascular repair, the occurrence of endoleak, which involves persistent blood flow within the aneurysm sac after stent graft placement, can necessitate additional interventions to address the issue.
- Aortic Rupture: While the goal of repair is to prevent aortic rupture, the procedure itself can carry a risk of aortic injury, particularly in cases of complex dissections or when manipulating fragile aortic tissue.
- Renal Complications: Both surgical and endovascular repair procedures can potentially impact renal function, leading to acute kidney injury or exacerbation of preexisting renal insufficiency.
- Respiratory Complications: Following surgical repair, individuals may be at risk of respiratory complications such as pneumonia, atelectasis, or ventilator-associated issues, particularly in the setting of prolonged intubation and intensive care stay.
- Bleeding and Hemorrhage: Surgical repair involves the risk of bleeding, both intraoperatively and postoperatively, which may necessitate blood transfusions or surgical revision.
- Infection: Surgical incisions and the placement of endovascular devices can increase the risk of infection, including deep sternal wound infections in the context of open surgical approaches.
- Cardiac Complications: Procedures involving the aortic root or ascending aorta can pose a risk of cardiac complications, including arrhythmias, myocardial infarction, or heart failure.
- Reintervention and Long-Term Surveillance: Regardless of the repair method, individuals may require long-term surveillance and potential reinterventions to address issues such as graft-related complications, recurrent dissection, or progressive aortic disease.
Previous care
The preoperative care of a patient undergoing aortic dissection repair involves comprehensive evaluation, stabilization, and preparation to optimize the individual’s condition for the upcoming surgical or endovascular intervention. Here are key aspects of the preoperative care for aortic dissection repair:
- Diagnostic Evaluation:
- Accurate diagnostic imaging, such as computed tomography angiography (CTA) or magnetic resonance imaging (MRI), is essential to precisely characterize the type, extent, and location of the aortic dissection.
- Hemodynamic Stabilization:
- Hemodynamic stabilization is a priority, and measures to control blood pressure and heart rate are often initiated to reduce the risk of dissection propagation and rupture.
- Medical Therapy:
- Patients are often initiated on medical therapy to manage blood pressure and heart rate, aiming to reduce the shear forces on the aortic wall and minimize the risk of dissection progression.
- Multidisciplinary Evaluation:
- A multidisciplinary team, including cardiovascular surgeons, interventional cardiologists, anesthesiologists, and critical care specialists, collaborates to assess the patient’s overall condition and determine the most suitable approach for aortic dissection repair.
- Risk Assessment:
- A thorough assessment of the patient’s comorbidities, including cardiovascular, pulmonary, renal, and neurological status, is conducted to evaluate the overall surgical risk and inform the decision-making process.
- Informed Consent:
- Patients and their families receive detailed information about the nature of the aortic dissection, the potential risks and benefits of repair, and the alternative management options, allowing them to make informed decisions and provide consent for the planned intervention.
- Optimization of Comorbid Conditions:
- Efforts to optimize comorbid conditions, such as managing heart failure, addressing pulmonary issues, or optimizing renal function, are undertaken to enhance the patient’s perioperative well-being.
- Psychosocial Support:
- Patients and their families receive psychosocial support and counseling to address concerns, alleviate anxiety, and ensure understanding of the upcoming procedure and its potential implications.
- Surgical Planning:
- Based on the specific characteristics of the aortic dissection, including its location and anatomical considerations, the surgical team plans the optimal approach for repair, whether open surgical or endovascular, taking into account the patient’s unique anatomy and clinical status.
- Preoperative Imaging and Marking:
- For endovascular repair, preoperative imaging is used to guide the selection and sizing of stent grafts, and the arterial access sites are marked for the upcoming procedure.
Aftercare
The postoperative care following aortic dissection repair, whether performed through surgical or endovascular means, is aimed at monitoring the patient’s recovery, managing potential complications, and promoting long-term cardiovascular health. Here are key aspects of the aftercare for individuals who have undergone aortic dissection repair:
- Intensive Care Monitoring:
- Following the procedure, patients are often initially managed in an intensive care unit (ICU) to allow close monitoring of vital signs, hemodynamic stability, and postoperative recovery.
- Hemodynamic Management:
- Continuation of meticulous blood pressure and heart rate control is essential to minimize the risk of dissection recurrence or extension, particularly in the immediate postoperative period.
- Pain Management:
- Adequate pain control is provided to ensure patient comfort and facilitate early mobilization, particularly in the context of open surgical repair involving sternotomy.
- Respiratory Support:
- Patients may require respiratory support, including monitoring for pulmonary complications and initiation of physiotherapy to prevent postoperative atelectasis and pneumonia.
- Neurological Monitoring:
- Close neurological monitoring is essential to detect any signs of stroke, spinal cord injury, or other neurological complications that may arise as a result of the repair procedure.
- Imaging Surveillance:
- Postoperative imaging studies, such as computed tomography (CT) or magnetic resonance imaging (MRI), are typically performed to assess the integrity of the repair, confirm proper graft/stent positioning, and monitor for any potential complications such as endoleak.
- Anticoagulation or Antiplatelet Therapy:
- Depending on the type of repair and the use of endovascular devices, patients may require anticoagulation or antiplatelet therapy to prevent thromboembolic events or to maintain stent graft patency.
- Rehabilitation and Mobilization:
- Early mobilization and rehabilitation efforts are initiated to promote physical recovery, reduce the risk of complications related to immobility, and support the patient’s overall recovery and well-being.
- Patient Education:
- Patients and their families receive comprehensive education regarding postoperative care, including activity restrictions, medication management, signs of potential complications, and the importance of long-term follow-up.
- Long-Term Surveillance:
- Long-term follow-up and surveillance are crucial to monitor the repaired aorta, assess for potential complications such as endoleak, and manage any ongoing cardiovascular risk factors.
- Cardiac Rehabilitation:
- For patients who have undergone aortic dissection repair, participation in a cardiac rehabilitation program may be recommended to optimize cardiovascular health, promote physical activity, and address modifiable risk factors.
- Psychosocial Support:
- Patients and their families receive ongoing psychosocial support to address any emotional or psychological challenges related to the aortic dissection diagnosis, the repair procedure, and the recovery process.
Only logged in customers who have purchased this product may leave a review.


Reviews
There are no reviews yet.