Description
Familiarity with treatment
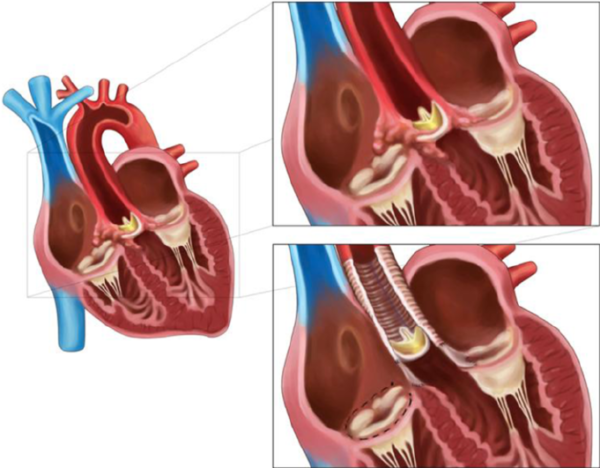
Bioprosthetic valve replacement is a widely used approach in cardiac surgery for addressing heart valve disease.
Types of Prosthetic Heart Valves
-
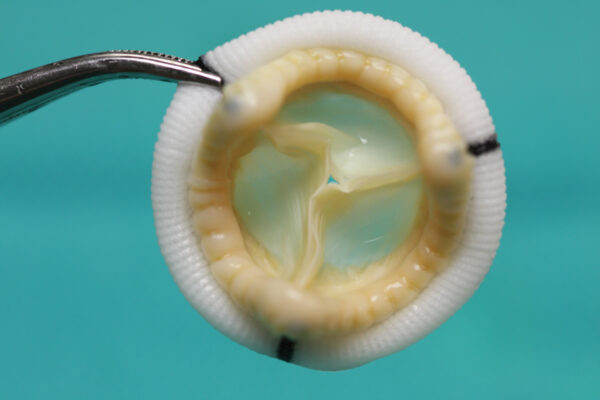
- Bioprosthetic Valves:
- Bioprosthetic valves are created from biological tissue and are known to offer functional properties similar to native valves. However, they are associated with limited longevity compared to mechanical valves 1.
- The choice of prosthesis, whether bioprosthetic or mechanical, is determined by the anticipated longevity of the patient and their ability to tolerate anticoagulation 1.
- The use of bioprosthetic valves has been increasing, especially among young patients, aiming to avoid the need for long-term anticoagulation 3.
- Mechanical Valves:
- Mechanical valves have subpar hemodynamics with increased thrombogenicity, requiring anticoagulation, but they generally have greater long-term durability 1.
- Homografts:
- Homografts are also mentioned as a type of prosthetic heart valve, representing another category of valve used in cardiac surgery 2.
Who is it suitable for?
Bioprosthetic valve replacement in cardiac surgery is suitable for a variety of patients, particularly those who may benefit from the unique characteristics of bioprosthetic valves. Here are some considerations for the suitability of bioprosthetic valve replacement:
Elderly Patients
-
- Reduced Anticoagulation Requirement: Bioprosthetic valves are well-suited for elderly patients who may have difficulty complying with long-term anticoagulation therapy, as these valves have a lower risk of thrombosis compared to mechanical valves.
- Improved Quality of Life: Elderly patients often benefit from the improved hemodynamics and reduced risk of complications associated with bioprosthetic valves, contributing to an improved quality of life.
Women of Childbearing Age
-
- Avoidance of Long-Term Anticoagulation: Bioprosthetic valves are considered for women of childbearing age who may wish to avoid the potential risks and limitations associated with long-term anticoagulation therapy during pregnancy.
Patients with Bleeding Risks
-
- Reduced Bleeding Risks: Patients with a history of bleeding disorders or those at an increased risk of bleeding due to concurrent medications or medical conditions may be suitable candidates for bioprosthetic valve replacement to minimize the need for anticoagulation.
Younger Patients
-
- Individual Considerations: While bioprosthetic valves have traditionally been less preferred in younger patients due to their limited longevity, advancements in valve technology and the potential for future valve-in-valve transcatheter interventions have expanded their suitability for select younger patients.
Patients with Limited Longevity Expectations
-
- Palliative Care Considerations: In patients with limited life expectancy, such as those with advanced age or significant comorbidities, bioprosthetic valve replacement may be a suitable option to provide symptom relief without the need for long-term anticoagulation.
Patient Preferences
-
- Lifestyle Considerations: Patients’ preferences and lifestyle considerations, including their ability to adhere to anticoagulation therapy and their desire to avoid the potential limitations associated with mechanical valves, play a significant role in the suitability of bioprosthetic valve replacement.
Who is it not suitable for?
Bioprosthetic valve replacement in cardiac surgery may not be suitable for certain patients due to specific clinical considerations. Here are some scenarios where bioprosthetic valve replacement may be less suitable:
Younger Patients with Long Life Expectancy
-
- Limited Longevity: Bioprosthetic valves have limited durability compared to mechanical valves, making them less suitable for younger patients with a long life expectancy who may face the need for multiple valve replacements over their lifetime.
- Potential Need for Anticoagulation: While bioprosthetic valves generally require less anticoagulation than mechanical valves, younger patients may still need anticoagulation, especially if they have other indications for it.
Patients Requiring Long-Term Anticoagulation
-
- High Thrombotic Risk: Patients with a history of or predisposition to thrombotic events may not be suitable candidates for bioprosthetic valves, as they may benefit from the thromboresistant properties of mechanical valves that necessitate anticoagulation.
Patients with Prior Bioprosthetic Valve Failure
-
- Risk of Reoperation: Patients who have previously undergone bioprosthetic valve replacement and experienced valve failure may not be suitable candidates for repeat bioprosthetic valve replacement due to concerns about the durability of subsequent bioprosthetic valves.
Patients with Complex Valve Pathology
-
- Need for Valve Repair: Patients with complex valve pathology that may be amenable to repair rather than replacement, such as certain forms of congenital valve disease or specific anatomical considerations, may not be ideal candidates for bioprosthetic valve replacement.
Patients with Contraindications to Biological Tissue
-
- Biological Material Allergies or Rejection: Patients with known allergies or hypersensitivity to biological materials used in bioprosthetic valves may not be suitable candidates due to the risk of adverse reactions or valve failure.
Patients with Specific Lifestyle Considerations
-
- Occupational or Lifestyle Factors: Patients with occupational or lifestyle factors that may increase the risk of accelerated valve degeneration, such as exposure to toxins or extreme physical activities, may not be ideal candidates for bioprosthetic valve replacement.
Advantages
Bioprosthetic valve replacement offers several advantages in cardiac surgery, particularly for specific patient populations. Here are some of the key advantages:
Reduced Need for Anticoagulation
-
- Lower Thrombotic Risk: Bioprosthetic valves generally have a lower risk of thrombosis compared to mechanical valves, reducing the need for lifelong anticoagulation therapy.
- Suitability for Elderly Patients: Patients who may have difficulty adhering to strict anticoagulation regimens, such as the elderly, may benefit from the reduced anticoagulation requirement associated with bioprosthetic valves.
Improved Hemodynamics
-
- Enhanced Flow Dynamics: Bioprosthetic valves offer improved hemodynamics, closely mimicking the function of natural heart valves and potentially contributing to better overall cardiac function and reduced risk of complications.
- Enhanced Quality of Life: The improved flow characteristics of bioprosthetic valves may lead to improved exercise tolerance and quality of life for patients.
Minimally Invasive Options
-
- Transcatheter Approaches: The development of transcatheter aortic valve replacement (TAVR) has expanded the application of bioprosthetic valves, providing minimally invasive options for patients with aortic valve disease, including those at high surgical risk.
- Reduced Surgical Trauma: Transcatheter deployment of bioprosthetic valves can reduce the need for traditional open-heart surgery, leading to shorter recovery times and reduced postoperative complications.
Suitable for Women of Childbearing Age
-
- Avoidance of Long-Term Anticoagulation: Bioprosthetic valves are considered for women of childbearing age who may wish to avoid the potential risks and limitations associated with long-term anticoagulation therapy during pregnancy.
Advancements in Valve Technology
-
- Long-Term Durability Improvements: Ongoing advancements in valve design and tissue processing aim to improve the longevity and durability of bioprosthetic valves, expanding their suitability for a broader range of patients, including younger individuals.
- Expansion of Clinical Indications: Growing evidence and clinical experience are expanding the appropriate clinical indications for bioprosthetic valve replacement, making these valves a viable option for a larger patient population.
Complications
Bioprosthetic valve replacement in cardiac surgery, while offering several advantages, is associated with potential complications. Here are some common complications associated with bioprosthetic valve replacement:
Structural Valve Deterioration
-
- Degeneration Over Time: Bioprosthetic valves are prone to structural degeneration over time, leading to valve dysfunction, regurgitation, or stenosis, which may necessitate reoperation or valve-in-valve transcatheter interventions.
Thrombosis and Embolism
-
- Valve Thrombosis: Although less common than with mechanical valves, bioprosthetic valves can still be associated with the risk of thrombosis, potentially leading to valve dysfunction and embolic events.
Endocarditis
-
- Infective Endocarditis: Bioprosthetic valves are susceptible to infective endocarditis, which requires prompt diagnosis and appropriate management to mitigate the risk of valve damage and systemic complications.
Valve-Related Hemolysis
-
- Mechanical Hemolytic Anemia: In some cases, bioprosthetic valves may cause mechanical hemolytic anemia due to turbulent blood flow, potentially leading to anemia and related symptoms.
Paravalvular Leak
-
- Leak Around the Valve: Paravalvular leaks can occur, leading to regurgitation around the valve, potentially compromising cardiac function and requiring intervention to address the leakage.
Prosthetic Valve Thrombosis
-
- Obstruction of the Valve: Prosthetic valve thrombosis can occur, leading to obstruction of blood flow through the valve and potentially causing symptoms of heart failure or embolic events.
Patient-Specific Complications
-
- Age-Related Degeneration: In younger patients, the risk of accelerated valve degeneration may lead to earlier reoperation or intervention to address valve dysfunction.
- Biological Material-related Reactions: Some patients may experience allergic or hypersensitivity reactions to the biological materials used in bioprosthetic valves, potentially leading to inflammation and valve dysfunction.
Procedural Complications
-
- Surgical Risks: As with any cardiac surgery, bioprosthetic valve replacement carries inherent risks related to the surgical procedure, anesthesia, and postoperative recovery.
Previous care
The care of patients following bioprosthetic valve replacement in cardiac surgery involves several key components to ensure optimal outcomes. Here are important aspects of postoperative care for individuals who have undergone bioprosthetic valve replacement:
Immediate Postoperative Period
-
- Intensive Care Monitoring: Close monitoring in the intensive care unit immediately following surgery to assess hemodynamic stability, respiratory function, and recovery from anesthesia.
- Pain Management: Adequate pain management to ensure patient comfort and facilitate early mobilization and respiratory function.
- Anticoagulation Management: Initiation of appropriate anticoagulation therapy, if indicated, in accordance with individual patient factors and the type of bioprosthetic valve used.
Early Mobilization and Rehabilitation
-
- Physical Therapy: Early mobilization and physical therapy to promote recovery, prevent complications such as deep vein thrombosis, and optimize functional outcomes.
- Rehabilitation Planning: Development of a comprehensive rehabilitation plan to support the patient’s recovery and return to daily activities.
Long-Term Follow-Up and Monitoring
-
- Regular Follow-Up Visits: Scheduled follow-up visits with the cardiac surgeon and/or cardiologist to monitor valve function, assess for potential complications, and adjust medication regimens as needed.
- Imaging Studies: Periodic imaging studies, such as echocardiograms, to evaluate the structural integrity and function of the bioprosthetic valve over time.
Anticoagulation Management
-
- Anticoagulation Regimens: Management of anticoagulation therapy, if indicated, with careful consideration of the patient’s clinical factors, individual risk of thrombosis, and bleeding risks.
- Patient Education: Patient education regarding the importance of adherence to anticoagulation therapy, potential side effects, and lifestyle modifications to optimize anticoagulation management.
Infection Prevention and Endocarditis Prophylaxis
-
- Antibiotic Prophylaxis: Administration of antibiotic prophylaxis for dental procedures and other high-risk activities to prevent infective endocarditis, in accordance with current guidelines.
- Infection Surveillance: Vigilant monitoring for signs of infective endocarditis or other potential sources of infection, with prompt evaluation and management as needed.
Lifestyle and Medication Management
-
- Lifestyle Modifications: Guidance on lifestyle modifications, including diet, exercise, and stress management, to promote cardiovascular health and overall well-being.
- Medication Adherence: Patient education on the importance of medication adherence, including anticoagulants, antiplatelet therapy, and other cardiovascular medications prescribed postoperatively.
Aftercare
The aftercare following bioprosthetic valve replacement in cardiac surgery is essential for ensuring the patient’s recovery and long-term well-being. Here are key components of aftercare for individuals who have undergone bioprosthetic valve replacement:
Recovery Period
-
- Hospital Stay: Monitoring the patient’s recovery in the hospital, typically in a specialized cardiac care unit, to ensure stability and assess for any immediate postoperative complications.
- Pain Management: Managing postoperative pain to facilitate comfort and early mobilization.
Medication Management
-
- Anticoagulation Therapy: Guiding the patient on the appropriate use of anticoagulant and/or antiplatelet medications, if prescribed, and ensuring adherence to the prescribed regimen.
- Cardiovascular Medications: Providing education on and ensuring adherence to medications for heart health, blood pressure management, and other relevant conditions.
Lifestyle Modifications
-
- Physical Activity Guidelines: Advising the patient on appropriate levels of physical activity and exercise, as well as any restrictions based on their individual recovery and the specific type of bioprosthetic valve implanted.
- Dietary Recommendations: Offering guidance on heart-healthy dietary choices to manage cardiovascular risk factors and promote overall well-being.
Follow-Up Care
-
- Scheduled Follow-Up Visits: Arranging regular follow-up appointments with the cardiac surgeon and/or cardiologist for ongoing monitoring of the bioprosthetic valve function and the patient’s overall cardiovascular health.
- Imaging Studies: Scheduling periodic echocardiograms or other imaging studies to assess the structural integrity and function of the bioprosthetic valve over time.
Infection Prevention
-
- Endocarditis Prophylaxis: Providing guidance on antibiotic prophylaxis for dental procedures and other high-risk activities to prevent infective endocarditis, as per current medical guidelines.
- Infection Surveillance: Instructing the patient to monitor for signs of potential infections, especially infective endocarditis, and promptly report any concerning symptoms.
Patient Education
-
- Symptom Recognition: Educating the patient about symptoms suggestive of valve dysfunction, embolic events, or other potential complications, and advising them to seek medical attention if such symptoms arise.
- Emergency Action Plan: Developing an emergency action plan with the patient, including instructions on when to seek urgent medical care and how to access emergency services if needed.
Psychological Support
-
- Emotional Well-being: Addressing the patient’s emotional well-being and offering psychological support as they navigate the recovery process and adapt to life with a bioprosthetic valve.
Long-Term Management
-
- Ongoing Care Coordination: Coordinating with the patient’s primary care physician and other healthcare providers to ensure comprehensive and integrated care for their cardiovascular health and overall well-being.
Only logged in customers who have purchased this product may leave a review.


Reviews
There are no reviews yet.