














Free
Embark on a transformative journey with our exceptional range of medical treatments. As a leading medical tour operator, we offer a comprehensive selection of world-class treatments and procedures to address your unique healthcare needs. From advanced surgeries to cutting-edge therapies, our team of experienced professionals is dedicated to providing top-notch care and ensuring your comfort and satisfaction. Discover a new level of healthcare excellence with our tailored treatment options. Book now to start your journey towards a healthier and happier you.
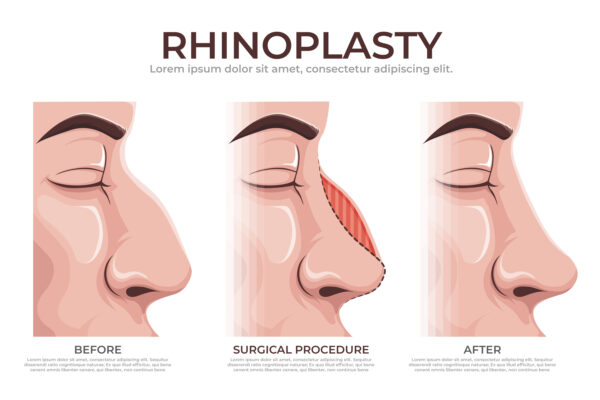
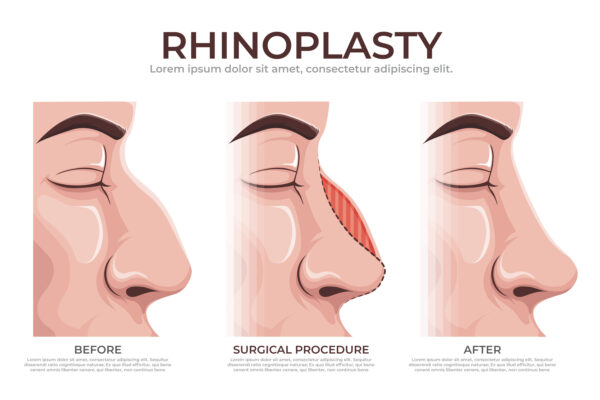
Open rhinoplasty is a surgical technique used to modify the shape and structure of the nose. It involves making an incision across the columella, the narrow strip of tissue that separates the nostrils, to gain access to the underlying nasal structures. The procedure provides improved visualization for the surgeon, allowing for more precise modifications and corrections.
Here is a general overview of the open rhinoplasty procedure:
Anesthesia: Before the procedure, anesthesia is administered to ensure your comfort. The options include intravenous sedation or general anesthesia, and your surgeon will recommend the best choice for you.
Incision: In open rhinoplasty, a small incision is made across the columella, which is the external portion of the nose between the nostrils. This incision allows the surgeon to lift the skin and gain direct access to the nasal structures.
Exposure and Reshaping: With the skin lifted, the surgeon can visualize and modify the underlying nasal bones, cartilage, and soft tissues. The surgeon may use various techniques, such as removing or reshaping cartilage, repositioning bones, or adding grafts, to achieve the desired changes in the nose’s shape and structure.
Closure: After the necessary modifications are made, the skin is repositioned and sutured closed. The incision is typically well-hidden and heals with minimal scarring.
Open rhinoplasty is often recommended for complex nasal deformities, revision rhinoplasty, or cases where precise modifications to the nasal tip are required. It allows for a more comprehensive view of the nasal structures, facilitating intricate adjustments.
Open rhinoplasty is suitable for individuals who require extensive modifications to their nose or have complex nasal deformities. It is commonly recommended for the following cases:
Revision Rhinoplasty: Open rhinoplasty is often preferred for revision cases where previous nasal surgeries have been performed. The open approach allows for better visualization and access to correct any previous surgical complications or unsatisfactory results.
Nasal Tumors: Individuals with nasal tumors may benefit from open rhinoplasty as it provides better access to remove the tumor and reconstruct the nose.
Congenital Disabilities: Open rhinoplasty may be suitable for individuals with congenital disabilities such as cleft lip or dermoid cysts, where more extensive modifications and corrections are required.
Nasal Tip Modifications: If the nasal tip requires significant reshaping or modifications, open rhinoplasty may be recommended. The direct access provided by the open approach allows for more precise adjustments to the nasal tip cartilage.
Complex Surgeries: Open rhinoplasty is generally preferred for complex nasal surgeries that involve multiple areas of the nose, such as the septum, dorsum, nostrils, or removal of lumps or bumps.
Open rhinoplasty may not be suitable for everyone, and there are certain situations where an alternative approach may be recommended. Here are some scenarios where open rhinoplasty may not be suitable:
Minor Nasal Modifications: If you only require minor modifications to the nasal tip or other areas of the nose, a closed rhinoplasty approach may be more appropriate. Closed rhinoplasty involves incisions made inside the nostrils, avoiding any external incisions.
Thin or Delicate Skin: Open rhinoplasty involves making an external incision, which can result in more visible scarring. If you have thin or delicate skin, it may be more prone to noticeable scarring, and a closed rhinoplasty approach may be recommended to minimize this risk.
Limited Nasal Concerns: If your concerns are primarily limited to a specific area of the nose, such as the nasal bridge or nasal tip, and do not require extensive modifications to the underlying structures, a more focused approach like tip rhinoplasty or bridge augmentation may be appropriate.
Unfavorable Anatomy: In some cases, the anatomy of the nose may not be suitable for open rhinoplasty. This could include individuals with very thick or sebaceous skin, inadequate blood supply, or previous trauma that has compromised the blood flow to the nose.
Medical Conditions: Certain medical conditions or factors, such as uncontrolled diabetes, bleeding disorders, or compromised immune system, may increase the risks associated with open rhinoplasty. In such cases, your surgeon may recommend alternative options or additional precautions.
Open rhinoplasty offers several advantages compared to other techniques. Here are some of the advantages of open rhinoplasty:
Improved Visualization: One of the main advantages of open rhinoplasty is the enhanced visualization it provides to the surgeon. The open approach allows for direct visualization of the nasal structures, including the cartilage, bones, and soft tissues. This improved visibility enables the surgeon to make more precise modifications and achieve optimal results 1.
Complex Modifications: Open rhinoplasty is particularly beneficial for cases that require extensive modifications or corrections. It allows the surgeon to have better access to the nasal structures, making it suitable for complex surgeries, revision rhinoplasty, or cases involving significant reshaping of the nose 2.
Cartilage Grafting: Open rhinoplasty provides easier access to the nasal cartilage, making it advantageous for procedures that involve cartilage grafting. The surgeon can harvest cartilage from various sources, such as the septum or ear, and use it to reshape or reconstruct the nose 3.
Precise Tip Modifications: The open approach allows for more precise modifications to the nasal tip. It provides a clear view of the nasal tip cartilage, enabling the surgeon to refine its shape, projection, and symmetry with greater accuracy 1.
Better Assessment of Nasal Asymmetry: Open rhinoplasty allows the surgeon to thoroughly examine and address nasal asymmetry. The direct visualization provided by the open approach helps identify and correct any structural imbalances or deviations that contribute to asymmetry 4.
Suitable for Challenging Cases: Open rhinoplasty is often preferred for cases with challenging nasal anatomy, such as thick or sebaceous skin, inadequate blood supply, or previous trauma. The open approach provides better access and control in such situations.
Open rhinoplasty, like any surgical procedure, carries potential risks and complications. Here are some of the complications that can occur with open rhinoplasty:
Scarring: Open rhinoplasty involves an external incision on the columella, which can result in visible scarring. However, with proper surgical techniques and wound care, the scar can often heal well and become less noticeable over time.
Bleeding: Bleeding is a common risk associated with any surgical procedure, including open rhinoplasty. While bleeding during the surgery is managed by the surgical team, postoperative bleeding can occur and may require medical attention.
Infection: Infection is a potential complication of any surgical procedure. Although rare, it can occur after open rhinoplasty. Proper sterile techniques during surgery and postoperative care can help minimize the risk of infection.
Nasal Obstruction: In some cases, open rhinoplasty can lead to nasal obstruction or difficulty breathing through the nose. This can occur due to changes in the nasal structures or excessive scar tissue formation. Nasal obstruction may require additional treatment or revision surgery to address the issue.
Nasal Asymmetry: Despite the surgeon’s best efforts, there is a risk of postoperative nasal asymmetry. This can occur due to factors such as healing patterns, tissue response, or inadequate surgical techniques. Revision surgery may be necessary to correct any noticeable asymmetry.
Altered Sensation: Temporary or permanent changes in sensation, such as numbness or altered feeling in the nasal area, can occur after open rhinoplasty. These changes are usually temporary but can persist in rare cases.
Unsatisfactory Aesthetic Results: While open rhinoplasty aims to achieve desired aesthetic outcomes, there is a possibility of unsatisfactory results. Factors such as individual healing, tissue response, or unrealistic expectations can contribute to suboptimal aesthetic outcomes.
Preoperative care is an essential part of preparing for open rhinoplasty. While the specific instructions may vary depending on the surgeon and individual case, here are some general preoperative care guidelines:
Medication: Follow your surgeon’s instructions regarding medication use before surgery. Avoid medications that can increase the risk of bleeding, such as aspirin, ibuprofen, and other non-steroidal anti-inflammatory drugs (NSAIDs). It is important to inform your surgeon about any medications, supplements, or herbal remedies you are currently taking.
Smoking: Refrain from smoking for at least two weeks before and after surgery. Smoking can delay healing and increase the risk of complications, including poor wound healing and scarring.
Medical Evaluation: Your surgeon may require you to undergo a preoperative medical evaluation to ensure that you are in good health for the procedure. This evaluation may include blood tests, imaging studies, and consultations with other specialists if necessary.
Avoiding Illness: If you develop any signs of illness, such as a cold, flu, or fever, notify your surgeon. Surgery should be postponed until you have fully recovered to minimize the risk of complications.
Preoperative Instructions: Follow any specific preoperative instructions provided by your surgeon. These may include guidelines on eating and drinking before surgery, showering with antibacterial soap, and avoiding certain skincare products or makeup on the day of surgery.
Arrangements for Recovery: Make necessary arrangements for your recovery period. Arrange for someone to drive you home after the surgery and have someone available to assist you during the initial days of recovery if needed.
Postoperative care is crucial for a successful recovery after open rhinoplasty. While specific instructions may vary depending on the surgeon and individual case, here are some general postoperative care guidelines:
Follow Surgeon’s Instructions: It is essential to carefully follow the postoperative instructions provided by your surgeon. These instructions may include wound care, medication usage, and activity restrictions. Adhering to these guidelines will help promote proper healing and minimize the risk of complications.
Nasal Care: Keep the splint and dressings dry as instructed by your surgeon. Avoid blowing your nose for at least two weeks after surgery. If you need to sneeze, do so with your mouth open to minimize pressure on the nose. Your surgeon may provide specific instructions for nasal irrigation or saline sprays to keep the nasal passages clean.
Pain Management: Take prescribed pain medications as directed by your surgeon to manage any discomfort or pain. Over-the-counter pain relievers should be avoided unless approved by your surgeon.
Swelling and Bruising: Swelling and bruising are common after open rhinoplasty. Apply cold compresses or ice packs to the nasal area as instructed by your surgeon to help reduce swelling and alleviate discomfort. Keep your head elevated while resting or sleeping to further minimize swelling.
Rest and Recovery: Allow yourself ample time to rest and recover after surgery. Avoid strenuous activities, heavy lifting, and exercise for the duration specified by your surgeon. Engage in light activities, such as walking, as recommended to promote circulation and aid in healing.
Diet and Hydration: Maintain a healthy diet and stay hydrated to support the healing process. Follow any dietary restrictions provided by your surgeon, such as avoiding certain foods or beverages that may interfere with healing.
Avoiding Sun Exposure: Protect your nose from direct sun exposure for several months following surgery. Apply sunscreen with a high SPF and wear a wide-brimmed hat when outdoors to prevent sunburn and minimize the risk of hyperpigmentation.
Follow-up Appointments: Attend all scheduled follow-up appointments with your surgeon. These appointments allow your surgeon to monitor your healing progress, remove any sutures or dressings, and address any concerns or questions you may have.
Only logged in customers who have purchased this product may leave a review.
Functional Rhinoplasty is a surgical procedure that focuses on improving the function of the nose, particularly in cases where there are structural issues or breathing difficulties. While cosmetic rhinoplasty primarily aims to enhance the appearance of the nose, functional rhinoplasty goes beyond aesthetics to address functional concerns.
During a functional rhinoplasty procedure, the surgeon may perform various techniques to correct structural abnormalities and improve nasal function. These techniques can include:
Nasal Valve Reconstruction: The nasal valves, located at the junction between the lower third and middle third of the nose, are responsible for a significant portion of nasal airflow resistance. In functional rhinoplasty, the surgeon may rebuild and strengthen the nasal valves to alleviate nasal obstruction and improve breathing.
Nasal Tip Elevation: If the nasal tip is drooping or obstructing the nasal airway, the surgeon may elevate and reshape it to improve nasal airflow.
Straightening the Nose: In cases where the nose is deviated or crooked, the surgeon may straighten it to enhance both the appearance and function of the nose.
Functional rhinoplasty can have a significant impact on a person’s quality of life by improving breathing, reducing nasal obstruction, and enhancing overall nasal function. It is worth noting that the specific techniques used and the extent of the procedure will depend on the individual’s unique case and the surgeon’s assessment.
Functional Rhinoplasty is suitable for individuals who have functional issues with their nose that affect their breathing and overall nasal function. It is not solely performed for cosmetic reasons, but rather to address structural abnormalities and improve nasal airflow.
Here are some factors that may make someone a suitable candidate for Functional Rhinoplasty:
Nasal Obstruction: If you experience chronic nasal obstruction or difficulty breathing through your nose due to structural issues, such as a deviated septum, collapsed nasal valves, or other obstructions, Functional Rhinoplasty may be recommended to correct these problems.
Nasal Trauma: Individuals who have experienced nasal trauma resulting in a nasal deformity or functional impairment may benefit from Functional Rhinoplasty to restore proper nasal function.
Congenital Conditions: Some individuals are born with structural abnormalities in the nose that can cause breathing difficulties. Functional Rhinoplasty can help correct these congenital conditions and improve nasal function.
Revision Rhinoplasty: If you have previously undergone rhinoplasty and are experiencing functional issues or dissatisfaction with the results, Functional Rhinoplasty may be performed to address these concerns and improve nasal function.
Functional Rhinoplasty may not be suitable for everyone. Here are some factors that may make someone not suitable for Functional Rhinoplasty:
Purely Cosmetic Concerns: Functional Rhinoplasty primarily focuses on improving nasal function rather than solely addressing cosmetic concerns. If an individual’s primary goal is to enhance the appearance of their nose without any functional issues, they may be better suited for cosmetic rhinoplasty.
Unrealistic Expectations: It is important for individuals considering Functional Rhinoplasty to have realistic expectations about the outcomes of the procedure. While it can improve nasal function, it may not completely resolve all breathing difficulties or achieve aesthetic perfection.
Medical Ineligibility: Some individuals may have medical conditions or health factors that make them ineligible for surgery. It is important to consult with a qualified plastic surgeon who can evaluate your medical history and determine if you are a suitable candidate for Functional Rhinoplasty.
Insufficient Nasal Structure: In some cases, individuals may have insufficient nasal structure or anatomy that cannot be adequately addressed through Functional Rhinoplasty alone. In such cases, alternative treatments or procedures may be recommended.
Functional Rhinoplasty offers several advantages, addressing both functional and aesthetic concerns. Here are some benefits associated with Functional Rhinoplasty:
Improved Nasal Function: The primary advantage of Functional Rhinoplasty is the improvement of nasal function. The procedure aims to correct structural abnormalities that may obstruct airflow, such as a deviated septum, collapsed nasal valves, or other obstructions. By addressing these issues, Functional Rhinoplasty can enhance nasal breathing and alleviate symptoms of nasal obstruction.
Enhanced Quality of Life: Functional Rhinoplasty can significantly improve the quality of life for individuals who have been experiencing breathing difficulties or nasal obstruction. By restoring proper nasal function, it can lead to better sleep, increased energy levels, improved exercise tolerance, and overall enhanced well-being.
Correction of Nasal Deformities: In addition to improving nasal function, Functional Rhinoplasty can also address cosmetic concerns associated with nasal deformities. While the primary focus is on functional improvement, the procedure can result in a more balanced and aesthetically pleasing nasal appearance.
Customized Approach: Functional Rhinoplasty is tailored to each individual’s specific needs. The surgeon will assess the patient’s nasal structure, functional concerns, and cosmetic goals to develop a personalized surgical plan. This customized approach ensures that the procedure addresses both functional and aesthetic aspects, providing optimal results.
Long-Term Results: Functional Rhinoplasty aims to provide long-lasting results. By addressing the underlying structural issues, the procedure can lead to sustained improvement in nasal function and aesthetics. However, it’s important to note that individual healing and recovery times may vary.
Functional Rhinoplasty, like any surgical procedure, carries potential risks and complications. Here are some complications that can occur:
Bleeding: Postoperative bleeding is a common complication in rhinoplasty. It is typically mild and resolves with conservative measures such as head elevation, nasal decongestants, and compression. In rare cases, persistent bleeding may require further intervention.
Infection: Although infections are rare, they can occur after rhinoplasty. Proper surgical techniques, sterile conditions, and postoperative care help minimize the risk of infection. Infections may require antibiotic treatment.
Poor Wound Healing: In some cases, wound healing may be delayed or compromised. Factors such as smoking, poor nutrition, or certain medical conditions can contribute to this complication. Proper preoperative care and adherence to postoperative instructions can help minimize the risk.
Nasal Obstruction: While the goal of Functional Rhinoplasty is to improve nasal function, there is a possibility of persistent or new-onset nasal obstruction. This can occur due to factors such as scar tissue formation, inadequate correction of structural abnormalities, or other anatomical variations.
Altered Sensation: Temporary or permanent changes in nasal sensation can occur after rhinoplasty. This can manifest as numbness, altered sensitivity, or hypersensitivity in the nasal area. In most cases, sensation returns to normal over time, but in rare instances, it may persist.
Asymmetry: Achieving perfect symmetry is challenging in rhinoplasty. Some degree of asymmetry may persist after surgery, especially in complex cases or revisions. Surgeons strive to achieve the best possible symmetry, but complete symmetry cannot always be guaranteed.
Unsatisfactory Aesthetic Outcome: While Functional Rhinoplasty primarily focuses on improving nasal function, it can also have aesthetic implications. There is a possibility that the desired cosmetic outcome may not be fully achieved or may not meet the patient’s expectations. Open communication with the surgeon during the preoperative planning phase is crucial to align expectations.
Preoperative care is an essential part of the overall rhinoplasty process, including functional rhinoplasty. It involves various steps and considerations to ensure a safe and successful surgical outcome. While the specific preoperative care may vary depending on individual circumstances and the surgeon’s recommendations, here are some general aspects to be aware of:
Patient Evaluation: Before undergoing functional rhinoplasty, a thorough evaluation is conducted by the surgeon. This evaluation typically includes a comprehensive medical history review, physical examination, and any necessary diagnostic tests or imaging. The purpose is to assess the patient’s overall health, nasal structure, and functional concerns to determine the most appropriate surgical approach.
Discussion of Expectations: It is crucial for patients to have realistic expectations about the outcomes of functional rhinoplasty. The surgeon will discuss the patient’s goals, explain what can be achieved through the procedure, and address any concerns or questions. Open communication between the patient and surgeon is essential to ensure a shared understanding of the expected results.
Medical Clearance: Depending on the patient’s medical history and overall health, the surgeon may request medical clearance from the patient’s primary care physician or other specialists. This step helps ensure that the patient is in good overall health and can safely undergo surgery.
Smoking Cessation: Smoking can significantly impact the healing process and increase the risk of complications. Therefore, patients are typically advised to quit smoking well in advance of the surgery. This includes avoiding smoking during the preoperative period to optimize healing and reduce the risk of complications.
Medication Review: The surgeon will review the patient’s current medications, including prescription drugs, over-the-counter medications, and supplements. Some medications may need to be adjusted or temporarily discontinued before the surgery to minimize the risk of bleeding or other complications.
Preoperative Instructions: Patients will receive specific preoperative instructions from their surgeon. These instructions may include guidelines regarding fasting before surgery, restrictions on eating or drinking, and the use of certain skincare products or medications. It is important to carefully follow these instructions to ensure a smooth and safe surgical experience.
Preoperative Testing: Depending on the patient’s medical history and the surgeon’s recommendations, preoperative testing may be required. This can include blood tests, imaging studies, or other diagnostic procedures to assess the patient’s overall health and identify any potential risk factors.
Proper postoperative care is crucial for a successful recovery after Functional Rhinoplasty. While specific instructions may vary depending on the surgeon’s preferences and the individual patient’s needs, here are some general guidelines:
Follow Surgeon’s Instructions: It is essential to carefully follow the postoperative instructions provided by your surgeon. These instructions may include guidelines for wound care, medication usage, activity restrictions, and follow-up appointments. Adhering to these instructions will help optimize healing and minimize the risk of complications.
Manage Discomfort: Pain and discomfort are common after rhinoplasty. Your surgeon may prescribe pain medication or recommend over-the-counter pain relievers to manage any discomfort. It’s important to take medications as directed and report any severe or worsening pain to your surgeon.
Nasal Splint and Dressings: After surgery, you may have a nasal splint or dressings in place to support and protect the nose. It’s important to keep the splint and dressings dry and clean as instructed by your surgeon. Avoid touching or manipulating them unless specifically advised by your surgeon.
Nasal Hygiene: Your surgeon may provide specific instructions for nasal hygiene. This may include saline nasal rinses or sprays to keep the nasal passages clean and moist. Following proper nasal hygiene practices can help reduce the risk of infection and promote healing.
Elevate Your Head: Keeping your head elevated while resting or sleeping can help reduce swelling and promote better healing. It’s recommended to sleep with your head elevated on pillows for the first few weeks following surgery.
Avoid Strenuous Activities: It’s important to avoid strenuous activities, heavy lifting, and exercise for a period of time as advised by your surgeon. Engaging in these activities too soon can increase the risk of bleeding, swelling, and complications.
Protect Your Nose: During the initial healing phase, it’s important to protect your nose from accidental bumps or trauma. Be cautious when engaging in activities that may pose a risk to your nose, and avoid wearing glasses or sunglasses that rest on the bridge of your nose until cleared by your surgeon.
Attend Follow-up Appointments: Regular follow-up appointments with your surgeon are crucial for monitoring your healing progress and addressing any concerns. It’s important to attend these appointments as scheduled and communicate any changes or issues you may be experiencing.
There are no reviews yet.
Only logged in customers who have purchased this product may leave a review.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment. The preferred choice for many patients is choosing private care.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment.
Reviews
There are no reviews yet.