
Free
Embark on a transformative journey with our exceptional range of medical treatments. As a leading medical tour operator, we offer a comprehensive selection of world-class treatments and procedures to address your unique healthcare needs. From advanced surgeries to cutting-edge therapies, our team of experienced professionals is dedicated to providing top-notch care and ensuring your comfort and satisfaction. Discover a new level of healthcare excellence with our tailored treatment options. Book now to start your journey towards a healthier and happier you.
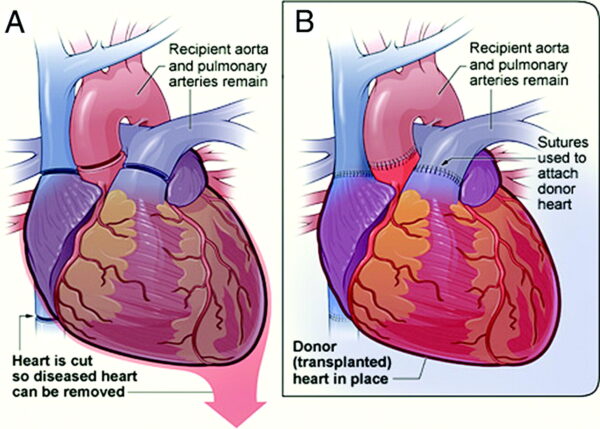
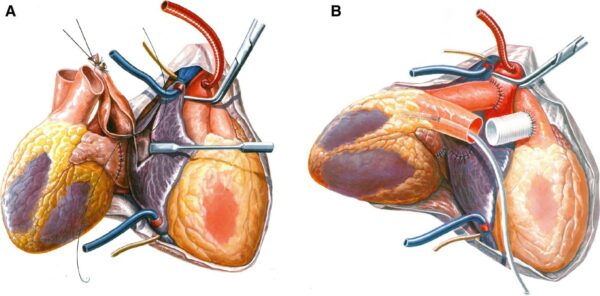
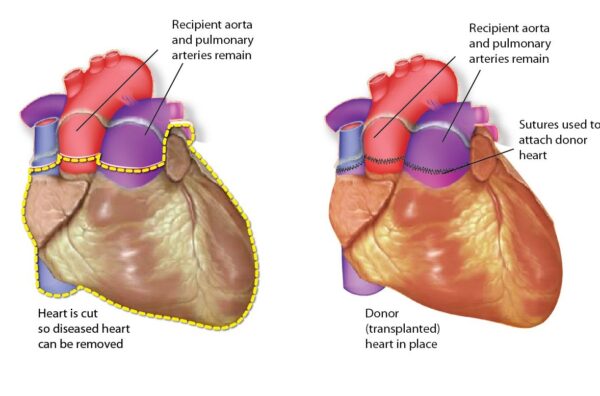
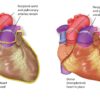
Heart transplantation is a complex and life-saving procedure performed in individuals with end-stage heart failure or severe heart conditions that cannot be effectively managed with other treatments. It involves replacing a diseased or failing heart with a healthy heart from a deceased donor.
The process of heart transplantation typically involves several steps, including:
Heart transplantation is typically considered as a treatment option for individuals with end-stage heart failure or severe heart conditions that cannot be effectively managed with other treatments. It may be suitable for individuals who meet certain criteria, including:
While heart transplantation can be a life-saving procedure for many individuals with end-stage heart failure, there are certain situations in which it may not be considered suitable. Some factors that may make a person ineligible for heart transplantation include:
Heart transplantation offers several potential advantages for individuals with end-stage heart failure or severe heart conditions that cannot be effectively managed with other treatments. Some of the advantages of heart transplantation include:
A heart transplant is a complex surgical procedure that involves replacing a diseased heart with a healthy one from a donor. While heart transplantation can be life-saving, there are potential complications that can arise. It’s important to note that the specific risks and complications can vary depending on individual factors such as overall health, age, and the specific circumstances of the transplant. Here are some of the potential complications associated with heart transplant:
Rejection: One of the most common complications of a heart transplant is rejection of the donor heart. This occurs when the immune system recognizes the transplanted heart as foreign and attacks it. Rejection can occur in the days, weeks, or months after the transplant, and sometimes even years later. Immunosuppressant medications are prescribed to reduce the risk of rejection, but it cannot always be completely prevented 1 2.
Infection: Infections can occur after any surgery, including heart transplantation. The use of immunosuppressant medications to prevent rejection can increase the risk of infections. Common infections that can occur after a heart transplant include surgical site infections, pneumonia, urinary tract infections, and viral infections. Close monitoring and appropriate treatment are essential to manage infections.
Bleeding: Bleeding during or after the surgery is a potential complication of heart transplant. Surgeons take precautions to minimize the risk of bleeding, but it can still occur. Blood transfusions or surgical interventions may be necessary to control bleeding 1.
Blood clots: Blood clots can form after a heart transplant, which can lead to serious complications such as heart attack, stroke, or lung problems. Medications are often prescribed to prevent blood clot formation 1.
Breathing problems: Some patients may experience breathing problems after a heart transplant. This can be due to various factors such as fluid accumulation in the lungs, infection, or rejection. Close monitoring and appropriate treatment are important to manage breathing difficulties.
Kidney failure: The use of immunosuppressant medications can sometimes affect kidney function. Kidney failure can occur as a potential complication of heart transplant. Regular monitoring of kidney function and appropriate management are necessary to prevent or manage kidney failure 1.
Coronary allograft vasculopathy (CAV): CAV is a condition where the blood vessels that carry blood to the transplanted heart become thick and hard. This can cause serious heart muscle damage. Regular monitoring and appropriate interventions are important to manage CAV 1.
Failure of the donor heart: In some cases, the transplanted heart may fail to function properly. This can be due to various factors such as rejection, infection, or other complications. Close monitoring and appropriate interventions are necessary to manage the failure of the donor heart 1.
Death: While rare, there is a risk of death associated with any surgical procedure, including heart transplant. The overall survival rates after heart transplantation have improved over the years, but it’s important to recognize that there are risks involved. The benefits of a heart transplant often outweigh the risks for patients with end-stage heart failure 1.
Before a heart transplant, patients with end-stage heart failure typically receive comprehensive care to manage their condition and optimize their health. This care may include:
After a heart transplant, patients require ongoing care and monitoring to ensure the success of the transplant and maintain their overall health. The aftercare following a heart transplant typically includes:
Only logged in customers who have purchased this product may leave a review.
Heart transplantation is a complex and life-saving procedure performed in individuals with end-stage heart failure or severe heart conditions that cannot be effectively managed with other treatments. It involves replacing a diseased or failing heart with a healthy heart from a deceased donor.
The process of heart transplantation typically involves several steps, including:
Heart transplantation is typically considered as a treatment option for individuals with end-stage heart failure or severe heart conditions that cannot be effectively managed with other treatments. It may be suitable for individuals who meet certain criteria, including:
While heart transplantation can be a life-saving procedure for many individuals with end-stage heart failure, there are certain situations in which it may not be considered suitable. Some factors that may make a person ineligible for heart transplantation include:
Heart transplantation offers several potential advantages for individuals with end-stage heart failure or severe heart conditions that cannot be effectively managed with other treatments. Some of the advantages of heart transplantation include:
A heart transplant is a complex surgical procedure that involves replacing a diseased heart with a healthy one from a donor. While heart transplantation can be life-saving, there are potential complications that can arise. It’s important to note that the specific risks and complications can vary depending on individual factors such as overall health, age, and the specific circumstances of the transplant. Here are some of the potential complications associated with heart transplant:
Rejection: One of the most common complications of a heart transplant is rejection of the donor heart. This occurs when the immune system recognizes the transplanted heart as foreign and attacks it. Rejection can occur in the days, weeks, or months after the transplant, and sometimes even years later. Immunosuppressant medications are prescribed to reduce the risk of rejection, but it cannot always be completely prevented 1 2.
Infection: Infections can occur after any surgery, including heart transplantation. The use of immunosuppressant medications to prevent rejection can increase the risk of infections. Common infections that can occur after a heart transplant include surgical site infections, pneumonia, urinary tract infections, and viral infections. Close monitoring and appropriate treatment are essential to manage infections.
Bleeding: Bleeding during or after the surgery is a potential complication of heart transplant. Surgeons take precautions to minimize the risk of bleeding, but it can still occur. Blood transfusions or surgical interventions may be necessary to control bleeding 1.
Blood clots: Blood clots can form after a heart transplant, which can lead to serious complications such as heart attack, stroke, or lung problems. Medications are often prescribed to prevent blood clot formation 1.
Breathing problems: Some patients may experience breathing problems after a heart transplant. This can be due to various factors such as fluid accumulation in the lungs, infection, or rejection. Close monitoring and appropriate treatment are important to manage breathing difficulties.
Kidney failure: The use of immunosuppressant medications can sometimes affect kidney function. Kidney failure can occur as a potential complication of heart transplant. Regular monitoring of kidney function and appropriate management are necessary to prevent or manage kidney failure 1.
Coronary allograft vasculopathy (CAV): CAV is a condition where the blood vessels that carry blood to the transplanted heart become thick and hard. This can cause serious heart muscle damage. Regular monitoring and appropriate interventions are important to manage CAV 1.
Failure of the donor heart: In some cases, the transplanted heart may fail to function properly. This can be due to various factors such as rejection, infection, or other complications. Close monitoring and appropriate interventions are necessary to manage the failure of the donor heart 1.
Death: While rare, there is a risk of death associated with any surgical procedure, including heart transplant. The overall survival rates after heart transplantation have improved over the years, but it’s important to recognize that there are risks involved. The benefits of a heart transplant often outweigh the risks for patients with end-stage heart failure 1.
Before a heart transplant, patients with end-stage heart failure typically receive comprehensive care to manage their condition and optimize their health. This care may include:
After a heart transplant, patients require ongoing care and monitoring to ensure the success of the transplant and maintain their overall health. The aftercare following a heart transplant typically includes:
There are no reviews yet.
Only logged in customers who have purchased this product may leave a review.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment. The preferred choice for many patients is choosing private care.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment.
Reviews
There are no reviews yet.