Description
Familiarity with treatment
Pacemaker placement is a common procedure used to treat certain heart conditions, such as bradycardia (a slow heart rate) or heart block. Familiarity with pacemaker placement involves understanding the procedure itself, the postoperative care required, and the potential complications that may arise. Here are some key points about pacemaker placement:
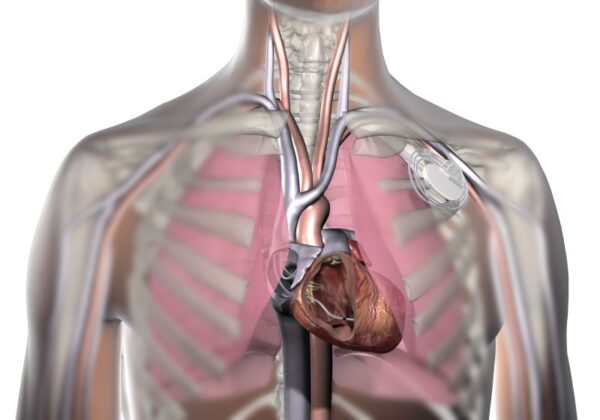
- Procedure: Pacemaker placement is typically performed in a hospital setting under local anesthesia. During the procedure, a small incision is made near the collarbone, and leads (thin wires) are threaded through a vein into the heart. The leads are then connected to a small device called a pacemaker, which is implanted under the skin.
- Postoperative Care: After pacemaker placement, it is important to keep the incision site clean and dry. Follow the surgeon’s instructions regarding dressing changes and wound care. Avoid strenuous activities and heavy lifting for a few weeks. Attend all scheduled follow-up appointments to monitor the functioning of the pacemaker and make any necessary adjustments.
- Pacemaker Functioning: The pacemaker continuously monitors the heart’s electrical activity and delivers electrical impulses to regulate the heart rate if it becomes too slow or irregular. Regular check-ups and device checks are necessary to ensure the pacemaker is functioning properly.
- Battery Life: Pacemakers have a battery that powers the device. The battery life varies depending on the type of pacemaker and the settings programmed by the healthcare provider. Regular follow-up appointments are important to monitor the battery life and plan for a battery replacement when needed.
- Potential Complications: While pacemaker placement is generally safe, there are potential complications that can occur, including infection, bleeding, lead dislodgement, or damage to blood vessels or nerves. It is important to report any signs of infection, such as redness, swelling, or discharge, to your healthcare provider.
- Lifestyle Modifications: After pacemaker placement, most people can resume their normal activities. However, certain precautions may be advised, such as avoiding strong magnetic fields or activities that involve intense contact sports. Your healthcare provider will provide specific guidelines based on your individual situation.
Who is it suitable for?
Pacemaker placement is suitable for individuals who have certain heart conditions that require the regulation of their heart rate. It is commonly recommended for individuals with:
- Bradycardia: Pacemakers are often used to treat bradycardia, which is a slow heart rate. If the heart beats too slowly, it can cause symptoms such as fatigue, dizziness, fainting, or shortness of breath. Pacemakers help regulate the heart rate and ensure that it beats at a normal pace.
- Heart Block: Heart block is a condition where the electrical signals that control the heart’s rhythm are delayed or blocked. This can cause the heart to beat irregularly or too slowly. Pacemakers can help restore a normal heart rhythm by providing electrical impulses to stimulate the heart when needed.
- Other Heart Conditions: Pacemakers may also be recommended for individuals with certain heart conditions, such as hypertrophic cardiomyopathy, dilated cardiomyopathy, or certain types of arrhythmias. In these cases, the pacemaker may be used in combination with other treatments to manage the condition.
The suitability for pacemaker placement is determined by a cardiologist or electrophysiologist based on a thorough evaluation of the individual’s medical history, symptoms, and diagnostic tests. They will assess the specific heart condition and determine if pacemaker placement is the appropriate treatment option.
Who is it not suitable for?
Pacemaker placement may not be suitable for everyone, and there are certain situations where it may not be recommended. Here are some factors that may make an individual not suitable for pacemaker placement:
- Stable Heart Rate: If an individual has a stable and normal heart rate without any symptoms or complications, pacemaker placement may not be necessary. Pacemakers are typically recommended for individuals with bradycardia (slow heart rate) or heart block, where the heart rate is significantly affected.
- Terminal Illness: In cases where an individual has a terminal illness with a limited life expectancy and the pacemaker placement would not significantly improve their quality of life, the procedure may not be recommended.
- Inability to Undergo Surgery: Pacemaker placement is a surgical procedure that requires making an incision and implanting the device. If an individual has significant health issues that make them unable to tolerate surgery or anesthesia, pacemaker placement may not be suitable.
- Active Infection: If an individual has an active infection, especially in the area where the pacemaker would be implanted, the procedure may be postponed until the infection is treated and resolved.
- Unrealistic Expectations: If an individual has unrealistic expectations about the benefits or outcomes of pacemaker placement, it may not be recommended. It is important to have a clear understanding of the purpose and limitations of the pacemaker.
Advantages
Pacemaker placement offers several advantages for individuals with certain heart conditions. Here are some of the key advantages of pacemaker placement:
- Heart Rate Regulation: Pacemakers are designed to regulate the heart rate and ensure that it beats at a normal pace. They can help treat bradycardia (slow heart rate) or heart block, where the electrical signals controlling the heart’s rhythm are delayed or blocked. By providing electrical impulses, pacemakers help maintain a steady and appropriate heart rate, improving overall heart function.
- Symptom Relief: For individuals experiencing symptoms related to bradycardia or heart block, such as fatigue, dizziness, fainting, or shortness of breath, pacemakers can provide significant symptom relief. By ensuring a proper heart rate, pacemakers help alleviate these symptoms and improve quality of life.
- Improved Exercise Tolerance: Pacemakers can enhance an individual’s ability to engage in physical activities. By regulating the heart rate, pacemakers allow individuals to exercise without experiencing symptoms related to a slow heart rate. This can lead to improved exercise tolerance and overall cardiovascular fitness.
- Prevention of Fainting Episodes: In individuals prone to fainting or syncope due to bradycardia or heart block, pacemakers can help prevent these episodes. By maintaining a stable heart rate, pacemakers reduce the risk of sudden drops in blood pressure and loss of consciousness.
- Customized Programming: Pacemakers can be programmed to meet the specific needs of each individual. The settings can be adjusted to deliver the appropriate level of electrical impulses based on the individual’s heart condition and activity level. This customization ensures optimal heart rate regulation and function.
- Long-Term Management: Pacemakers are designed to be long-lasting and durable. With regular follow-up appointments and monitoring, the pacemaker can be adjusted and optimized over time to meet the changing needs of the individual. This long-term management helps maintain heart health and overall well-being.
Complications
While pacemaker placement is generally considered safe and effective, there are potential complications that can arise. It’s important to be aware of these complications and discuss them with your healthcare provider before undergoing the procedure. Here are some possible complications associated with pacemaker placement:
- Infection: Infection at the site of pacemaker placement is a potential complication. Signs of infection may include redness, swelling, warmth, pain, or discharge at the incision site. In some cases, the infection may spread to the pacemaker leads or the heart itself, requiring further treatment.
- Bleeding or Hematoma: Bleeding or the formation of a hematoma (a collection of blood) at the incision site can occur after pacemaker placement. This may require additional intervention, such as drainage or blood transfusion, depending on the severity.
- Lead Dislodgement or Fracture: The leads that connect the pacemaker to the heart can become dislodged or fractured, which may affect the proper functioning of the pacemaker. This can occur due to trauma, improper lead placement, or natural movement of the leads over time.
- Pneumothorax: In rare cases, the insertion of the pacemaker leads can cause a pneumothorax, which is the accumulation of air in the space between the lung and chest wall. This can lead to difficulty breathing and may require treatment, such as chest tube insertion.
- Allergic Reaction: Some individuals may have an allergic reaction to the materials used in the pacemaker or the sutures used to close the incision. This can cause symptoms such as rash, itching, or swelling.
- Nerve or Blood Vessel Damage: During the pacemaker placement procedure, there is a small risk of damage to nearby nerves or blood vessels. This can result in numbness, weakness, or circulation problems in the affected area.
- Device-related Complications: Over time, pacemakers may experience device-related complications, such as battery depletion, lead insulation failure, or malfunctioning of the electronic components. Regular follow-up appointments and device checks are necessary to monitor the functioning of the pacemaker and address any potential issues.
Preoperative care
Preoperative care for pacemaker placement involves several important steps to ensure the safety and success of the procedure. Here are some key aspects of preoperative care for pacemaker placement:
- Medical Evaluation: The patient should undergo a thorough medical evaluation to assess their overall health and suitability for the procedure. This may include a physical examination, blood tests, electrocardiogram (ECG), and other diagnostic tests.
- Medication Review: The patient’s current medications should be reviewed to identify any that may need to be adjusted or temporarily stopped before the procedure. Certain medications, such as blood thinners, may need to be managed carefully to minimize the risk of bleeding during and after the procedure.
- Fasting: The patient will typically be instructed to fast for a certain period of time before the procedure. This is to ensure that the stomach is empty, reducing the risk of complications during anesthesia.
- Informed Consent: The patient should be fully informed about the procedure, its risks, benefits, and alternatives. Informed consent should be obtained before the procedure.
- Preoperative Instructions: The patient will receive specific instructions regarding preoperative preparations, such as showering with a special antibacterial soap the night before the procedure. They may also be advised to avoid certain activities or medications in the days leading up to the procedure.
- Anesthesia Evaluation: If general anesthesia will be used during the procedure, the patient may need to undergo a separate anesthesia evaluation to assess their fitness for anesthesia and to discuss any concerns or questions.
- Preoperative Testing: Additional tests may be ordered to assess the patient’s cardiac function and anatomy, such as echocardiogram or cardiac catheterization.
- Arrangements for Transportation: The patient will need to arrange for transportation to and from the hospital or surgical center on the day of the procedure, as they may not be able to drive themselves after the procedure.
Postoperative care
Postoperative care after pacemaker placement is crucial to promote healing, prevent complications, and ensure the proper functioning of the pacemaker. Here are some key aspects of postoperative care for pacemaker placement:
- Monitoring: The patient will be closely monitored in the immediate postoperative period, including vital signs, heart rhythm, and oxygen levels. This may involve continuous monitoring in the hospital or periodic monitoring at home.
- Incision Care: The incision site should be kept clean and dry to prevent infection. The patient may be instructed to avoid getting the incision wet for a certain period of time and to change dressings as directed by their healthcare provider.
- Pain Management: The patient may experience some discomfort or pain at the incision site. Pain medication may be prescribed to manage pain and promote comfort. It is important for the patient to follow the prescribed pain management regimen and report any severe or worsening pain to their healthcare provider.
- Activity Restrictions: The patient will be given specific instructions regarding activity restrictions and limitations. This may include avoiding heavy lifting, strenuous exercise, or activities that may strain the incision site. Gradual resumption of normal activities will be guided by the healthcare provider.
- Medication Management: The patient will be prescribed medications to prevent infection and manage any underlying heart conditions. It is important for the patient to take medications as prescribed and follow up with their healthcare provider for any necessary adjustments or changes.
- Follow-up Appointments: The patient will need to schedule and attend follow-up appointments with their healthcare provider to monitor the pacemaker function, assess healing, and make any necessary adjustments to the pacemaker settings.
- Pacemaker Care: The patient will receive instructions on how to care for the pacemaker, including avoiding certain activities or movements that may disrupt the pacemaker leads or cause damage. They may also be advised to avoid certain electronic devices or environments that may interfere with the pacemaker’s function.
- Signs of Complications: The patient should be aware of the signs and symptoms of potential complications, such as infection, bleeding, or changes in heart rhythm. They should promptly report any concerning symptoms to their healthcare provider.
Only logged in customers who have purchased this product may leave a review.



Reviews
There are no reviews yet.