
Free
Embark on a transformative journey with our exceptional range of medical treatments. As a leading medical tour operator, we offer a comprehensive selection of world-class treatments and procedures to address your unique healthcare needs. From advanced surgeries to cutting-edge therapies, our team of experienced professionals is dedicated to providing top-notch care and ensuring your comfort and satisfaction. Discover a new level of healthcare excellence with our tailored treatment options. Book now to start your journey towards a healthier and happier you.
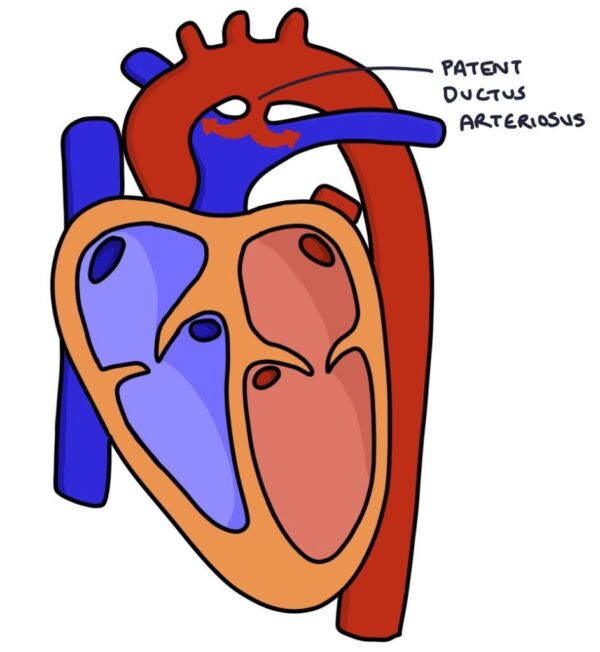
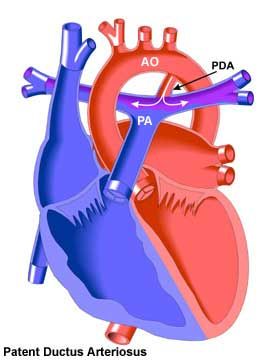
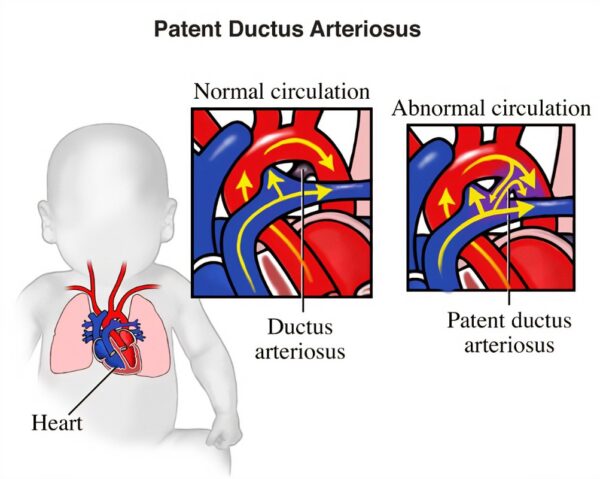
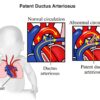
PDA closure surgery is a procedure performed to close a patent ductus arteriosus, which is a persistent opening between the pulmonary artery and the aorta. This opening, which is present in fetal circulation, is supposed to close shortly after birth. However, in some cases, the ductus arteriosus remains open, causing abnormal blood flow between the two major blood vessels of the heart.
The surgical closure of PDA is typically recommended when the defect is large, causing significant symptoms or complications. The procedure aims to close the opening and restore normal blood flow within the heart. There are two main approaches to PDA closure surgery:
Open-heart surgery: This traditional approach involves making an incision in the chest to access the heart. The surgeon then directly closes the PDA using sutures or a patch. Open-heart surgery is typically performed under general anesthesia and requires the use of a heart-lung bypass machine to maintain circulation during the procedure.
Catheter-based closure: In recent years, minimally invasive techniques have been developed for PDA closure. This approach involves inserting a catheter through a small incision in the groin and guiding it to the site of the PDA using imaging techniques. The catheter is used to deliver a device, such as a coil or an occluder, to close the PDA. This procedure is less invasive, requires a shorter hospital stay, and generally has a quicker recovery time compared to open-heart surgery.
The choice of surgical approach depends on various factors, including the size and location of the PDA, the individual’s age and overall health, and the expertise of the healthcare team.
Patent Ductus Arteriosus (PDA) closure surgery is typically suitable for individuals who meet certain criteria. The decision for surgery is usually based on factors such as the size of the PDA, the presence of symptoms or complications, and the individual’s overall health. Here are some general considerations:
Size of the PDA: Large PDAs are more likely to require surgical closure compared to small PDAs. A large PDA can cause significant symptoms and complications, such as heart failure or pulmonary hypertension, which may necessitate surgery.
Symptoms and Complications: Individuals experiencing symptoms related to the PDA, such as difficulty breathing, poor growth, or recurrent respiratory infections, may be candidates for surgery. Additionally, if the PDA is causing complications like heart failure or pulmonary hypertension, surgical closure may be recommended.
Failed Alternative Treatments: If alternative treatments, such as medication or catheter-based closure, have been unsuccessful in closing the PDA or managing symptoms, surgery may be considered.
Risk of Complications: Certain individuals, such as premature infants or those with specific medical conditions, may be at higher risk of complications related to a persistent PDA. In such cases, surgery may be considered to prevent potential long-term complications.
Individualized Assessment: The decision for PDA closure surgery is made on a case-by-case basis. The healthcare team, typically including a pediatric cardiologist or a congenital heart surgeon, will evaluate the individual’s specific condition, symptoms, and overall health to determine the most suitable treatment approach.
There are certain situations where Patent Ductus Arteriosus (PDA) closure surgery may not be suitable. These include:
Small and Asymptomatic PDAs: Small PDAs that are not causing significant symptoms or complications may not require surgical intervention. In such cases, the healthcare team may opt for a period of observation or alternative treatments like medication.
Premature Infants: Premature infants with PDAs may have a higher likelihood of spontaneous closure without the need for surgery. The healthcare team will closely monitor the PDA’s size and the infant’s overall health to determine the most appropriate course of action.
Unfavorable Anatomy: In some cases, the anatomy of the PDA may not be suitable for surgical closure. This could be due to its location, size, or associated abnormalities. The healthcare team will assess the individual’s specific condition to determine if surgery is feasible.
High Surgical Risk: Individuals with significant comorbidities or complex medical conditions may be at higher risk for surgical complications. In such cases, the healthcare team may explore alternative treatment options or consider a conservative approach.
Based on the search results, here are some potential advantages of Patent Ductus Arteriosus (PDA) closure:
Improved Symptoms: Closure of a significant PDA can alleviate symptoms associated with the condition, such as difficulty breathing, poor growth, or recurrent respiratory infections.
Prevention of Complications: Surgical closure of a PDA can help prevent potential long-term complications, including heart failure, pulmonary hypertension, and problems with the lungs and heart 1.
Restoration of Normal Blood Flow: PDA closure surgery aims to restore normal blood flow within the heart by closing the abnormal connection between the pulmonary artery and the aorta 2.
Long-Term Outlook: The long-term outlook after PDA closure surgery is generally excellent. In most cases, no additional surgeries or catheterizations are needed, and individuals can lead normal lives without increased risk 3.
Minimally Invasive Options: In addition to traditional open-heart surgery, there are minimally invasive techniques available for PDA closure, such as catheter-based procedures. These approaches offer advantages such as shorter hospital stays, quicker recovery times, and reduced invasiveness.
Based on the search results, here are some potential complications associated with Patent Ductus Arteriosus (PDA) closure:
Complications of Surgical Closure: Surgical closure of PDA, while generally safe, can be associated with potential complications. These may include bleeding, injury to nearby structures such as the recurrent laryngeal nerve or the vagus nerve, disruption of the thoracic duct leading to chylothorax, and rare but serious complications like ligation of the left pulmonary artery or other arterial structures within the chest.
Complications of Catheter Closure: Transcatheter closure of PDA using catheter-based procedures can also have complications. These may include bleeding at the catheterization site, rupture of blood vessels, tachyarrhythmias, bradyarrhythmias, vascular occlusion, inappropriate deployment or migration of the device, incomplete closure of the ductus, and rare cases of death, particularly in very low birth weight infants.
Postoperative Complications: Following PDA closure surgery, there can be postoperative complications such as pneumothorax (collapsed lung), chylothorax (leakage of lymphatic fluid into the chest cavity), and vocal cord paralysis. However, it’s important to note that the occurrence of these complications is generally low.
The specific care provided before surgery can vary depending on the individual’s condition and the healthcare facility’s protocols. However, here are some general aspects of care that may be involved:
Medical Evaluation: Before surgery, the individual will undergo a thorough medical evaluation, which may include a physical examination, medical history review, and diagnostic tests such as echocardiography, electrocardiography (ECG), and chest X-ray. These tests help determine the size and impact of the PDA and evaluate the individual’s overall health.
Symptom Management: If the individual is experiencing symptoms related to the PDA, such as difficulty breathing or poor growth, appropriate medical management may be initiated. This can include medications to improve heart function, manage symptoms, and stabilize the individual’s condition prior to surgery.
Preoperative Preparation: In preparation for surgery, the healthcare team will provide instructions regarding fasting, medication management, and any necessary preoperative tests or procedures. They will also discuss the surgical procedure, potential risks and benefits, and address any concerns or questions the individual or their family may have.
Preoperative Counseling: The individual and their family will have the opportunity to meet with the surgical team, including the surgeon and anesthesiologist, to discuss the details of the procedure, postoperative care, and expected outcomes. This counseling session allows for an informed decision-making process and helps alleviate any anxiety or concerns.
Consent Process: Prior to surgery, the individual or their legal guardian will be required to provide informed consent for the procedure. This involves understanding the risks, benefits, and potential alternatives to surgery, and giving permission for the surgical team to proceed.
Aftercare following Patent Ductus Arteriosus (PDA) closure surgery is essential for a smooth recovery and optimal outcomes. The specific aftercare instructions may vary depending on the individual’s condition, the surgical approach used, and the healthcare facility’s protocols. However, here are some general aspects of aftercare that may be involved:
Monitoring: After surgery, the individual will be closely monitored in a specialized cardiac care unit or a designated postoperative recovery area. This monitoring includes vital signs, oxygen levels, heart rhythm, and overall recovery progress.
Pain Management: Pain management strategies are typically employed to ensure the individual’s comfort. This may involve the use of pain medications, either oral or intravenous, as prescribed by the healthcare team.
Fluid and Nutrition: The healthcare team will carefully manage the individual’s fluid and nutrition intake to maintain adequate hydration and support healing. In some cases, intravenous fluids may be administered initially, gradually transitioning to oral intake as tolerated.
Mobility and Activity: Gradual mobilization and activity are encouraged as the individual’s condition permits. This helps prevent complications such as blood clots and promotes overall recovery. The healthcare team will provide guidance on appropriate levels of activity and any restrictions that may be necessary.
Wound Care: The surgical incision site will require proper care and monitoring. The healthcare team will provide instructions on how to keep the incision clean, dry, and protected to minimize the risk of infection. They will also discuss signs of infection to watch for and when to seek medical attention.
Medication Management: The individual may be prescribed medications to support the healing process, manage pain, prevent infection, and address any other specific needs. It’s important to follow the prescribed medication regimen and attend any follow-up appointments for medication adjustments or discontinuation.
Follow-up Appointments: The healthcare team will schedule follow-up appointments to monitor the individual’s progress and assess the success of the PDA closure. These appointments may include physical examinations, echocardiograms, or other diagnostic tests to evaluate the healing process and ensure the PDA has been effectively closed.
Only logged in customers who have purchased this product may leave a review.
PDA closure surgery is a procedure performed to close a patent ductus arteriosus, which is a persistent opening between the pulmonary artery and the aorta. This opening, which is present in fetal circulation, is supposed to close shortly after birth. However, in some cases, the ductus arteriosus remains open, causing abnormal blood flow between the two major blood vessels of the heart.
The surgical closure of PDA is typically recommended when the defect is large, causing significant symptoms or complications. The procedure aims to close the opening and restore normal blood flow within the heart. There are two main approaches to PDA closure surgery:
Open-heart surgery: This traditional approach involves making an incision in the chest to access the heart. The surgeon then directly closes the PDA using sutures or a patch. Open-heart surgery is typically performed under general anesthesia and requires the use of a heart-lung bypass machine to maintain circulation during the procedure.
Catheter-based closure: In recent years, minimally invasive techniques have been developed for PDA closure. This approach involves inserting a catheter through a small incision in the groin and guiding it to the site of the PDA using imaging techniques. The catheter is used to deliver a device, such as a coil or an occluder, to close the PDA. This procedure is less invasive, requires a shorter hospital stay, and generally has a quicker recovery time compared to open-heart surgery.
The choice of surgical approach depends on various factors, including the size and location of the PDA, the individual’s age and overall health, and the expertise of the healthcare team.
Patent Ductus Arteriosus (PDA) closure surgery is typically suitable for individuals who meet certain criteria. The decision for surgery is usually based on factors such as the size of the PDA, the presence of symptoms or complications, and the individual’s overall health. Here are some general considerations:
Size of the PDA: Large PDAs are more likely to require surgical closure compared to small PDAs. A large PDA can cause significant symptoms and complications, such as heart failure or pulmonary hypertension, which may necessitate surgery.
Symptoms and Complications: Individuals experiencing symptoms related to the PDA, such as difficulty breathing, poor growth, or recurrent respiratory infections, may be candidates for surgery. Additionally, if the PDA is causing complications like heart failure or pulmonary hypertension, surgical closure may be recommended.
Failed Alternative Treatments: If alternative treatments, such as medication or catheter-based closure, have been unsuccessful in closing the PDA or managing symptoms, surgery may be considered.
Risk of Complications: Certain individuals, such as premature infants or those with specific medical conditions, may be at higher risk of complications related to a persistent PDA. In such cases, surgery may be considered to prevent potential long-term complications.
Individualized Assessment: The decision for PDA closure surgery is made on a case-by-case basis. The healthcare team, typically including a pediatric cardiologist or a congenital heart surgeon, will evaluate the individual’s specific condition, symptoms, and overall health to determine the most suitable treatment approach.
There are certain situations where Patent Ductus Arteriosus (PDA) closure surgery may not be suitable. These include:
Small and Asymptomatic PDAs: Small PDAs that are not causing significant symptoms or complications may not require surgical intervention. In such cases, the healthcare team may opt for a period of observation or alternative treatments like medication.
Premature Infants: Premature infants with PDAs may have a higher likelihood of spontaneous closure without the need for surgery. The healthcare team will closely monitor the PDA’s size and the infant’s overall health to determine the most appropriate course of action.
Unfavorable Anatomy: In some cases, the anatomy of the PDA may not be suitable for surgical closure. This could be due to its location, size, or associated abnormalities. The healthcare team will assess the individual’s specific condition to determine if surgery is feasible.
High Surgical Risk: Individuals with significant comorbidities or complex medical conditions may be at higher risk for surgical complications. In such cases, the healthcare team may explore alternative treatment options or consider a conservative approach.
Based on the search results, here are some potential advantages of Patent Ductus Arteriosus (PDA) closure:
Improved Symptoms: Closure of a significant PDA can alleviate symptoms associated with the condition, such as difficulty breathing, poor growth, or recurrent respiratory infections.
Prevention of Complications: Surgical closure of a PDA can help prevent potential long-term complications, including heart failure, pulmonary hypertension, and problems with the lungs and heart 1.
Restoration of Normal Blood Flow: PDA closure surgery aims to restore normal blood flow within the heart by closing the abnormal connection between the pulmonary artery and the aorta 2.
Long-Term Outlook: The long-term outlook after PDA closure surgery is generally excellent. In most cases, no additional surgeries or catheterizations are needed, and individuals can lead normal lives without increased risk 3.
Minimally Invasive Options: In addition to traditional open-heart surgery, there are minimally invasive techniques available for PDA closure, such as catheter-based procedures. These approaches offer advantages such as shorter hospital stays, quicker recovery times, and reduced invasiveness.
Based on the search results, here are some potential complications associated with Patent Ductus Arteriosus (PDA) closure:
Complications of Surgical Closure: Surgical closure of PDA, while generally safe, can be associated with potential complications. These may include bleeding, injury to nearby structures such as the recurrent laryngeal nerve or the vagus nerve, disruption of the thoracic duct leading to chylothorax, and rare but serious complications like ligation of the left pulmonary artery or other arterial structures within the chest.
Complications of Catheter Closure: Transcatheter closure of PDA using catheter-based procedures can also have complications. These may include bleeding at the catheterization site, rupture of blood vessels, tachyarrhythmias, bradyarrhythmias, vascular occlusion, inappropriate deployment or migration of the device, incomplete closure of the ductus, and rare cases of death, particularly in very low birth weight infants.
Postoperative Complications: Following PDA closure surgery, there can be postoperative complications such as pneumothorax (collapsed lung), chylothorax (leakage of lymphatic fluid into the chest cavity), and vocal cord paralysis. However, it’s important to note that the occurrence of these complications is generally low.
The specific care provided before surgery can vary depending on the individual’s condition and the healthcare facility’s protocols. However, here are some general aspects of care that may be involved:
Medical Evaluation: Before surgery, the individual will undergo a thorough medical evaluation, which may include a physical examination, medical history review, and diagnostic tests such as echocardiography, electrocardiography (ECG), and chest X-ray. These tests help determine the size and impact of the PDA and evaluate the individual’s overall health.
Symptom Management: If the individual is experiencing symptoms related to the PDA, such as difficulty breathing or poor growth, appropriate medical management may be initiated. This can include medications to improve heart function, manage symptoms, and stabilize the individual’s condition prior to surgery.
Preoperative Preparation: In preparation for surgery, the healthcare team will provide instructions regarding fasting, medication management, and any necessary preoperative tests or procedures. They will also discuss the surgical procedure, potential risks and benefits, and address any concerns or questions the individual or their family may have.
Preoperative Counseling: The individual and their family will have the opportunity to meet with the surgical team, including the surgeon and anesthesiologist, to discuss the details of the procedure, postoperative care, and expected outcomes. This counseling session allows for an informed decision-making process and helps alleviate any anxiety or concerns.
Consent Process: Prior to surgery, the individual or their legal guardian will be required to provide informed consent for the procedure. This involves understanding the risks, benefits, and potential alternatives to surgery, and giving permission for the surgical team to proceed.
Aftercare following Patent Ductus Arteriosus (PDA) closure surgery is essential for a smooth recovery and optimal outcomes. The specific aftercare instructions may vary depending on the individual’s condition, the surgical approach used, and the healthcare facility’s protocols. However, here are some general aspects of aftercare that may be involved:
Monitoring: After surgery, the individual will be closely monitored in a specialized cardiac care unit or a designated postoperative recovery area. This monitoring includes vital signs, oxygen levels, heart rhythm, and overall recovery progress.
Pain Management: Pain management strategies are typically employed to ensure the individual’s comfort. This may involve the use of pain medications, either oral or intravenous, as prescribed by the healthcare team.
Fluid and Nutrition: The healthcare team will carefully manage the individual’s fluid and nutrition intake to maintain adequate hydration and support healing. In some cases, intravenous fluids may be administered initially, gradually transitioning to oral intake as tolerated.
Mobility and Activity: Gradual mobilization and activity are encouraged as the individual’s condition permits. This helps prevent complications such as blood clots and promotes overall recovery. The healthcare team will provide guidance on appropriate levels of activity and any restrictions that may be necessary.
Wound Care: The surgical incision site will require proper care and monitoring. The healthcare team will provide instructions on how to keep the incision clean, dry, and protected to minimize the risk of infection. They will also discuss signs of infection to watch for and when to seek medical attention.
Medication Management: The individual may be prescribed medications to support the healing process, manage pain, prevent infection, and address any other specific needs. It’s important to follow the prescribed medication regimen and attend any follow-up appointments for medication adjustments or discontinuation.
Follow-up Appointments: The healthcare team will schedule follow-up appointments to monitor the individual’s progress and assess the success of the PDA closure. These appointments may include physical examinations, echocardiograms, or other diagnostic tests to evaluate the healing process and ensure the PDA has been effectively closed.
There are no reviews yet.
Only logged in customers who have purchased this product may leave a review.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment. The preferred choice for many patients is choosing private care.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment.
Reviews
There are no reviews yet.