Free
Embark on a transformative journey with our exceptional range of medical treatments. As a leading medical tour operator, we offer a comprehensive selection of world-class treatments and procedures to address your unique healthcare needs. From advanced surgeries to cutting-edge therapies, our team of experienced professionals is dedicated to providing top-notch care and ensuring your comfort and satisfaction. Discover a new level of healthcare excellence with our tailored treatment options. Book now to start your journey towards a healthier and happier you.
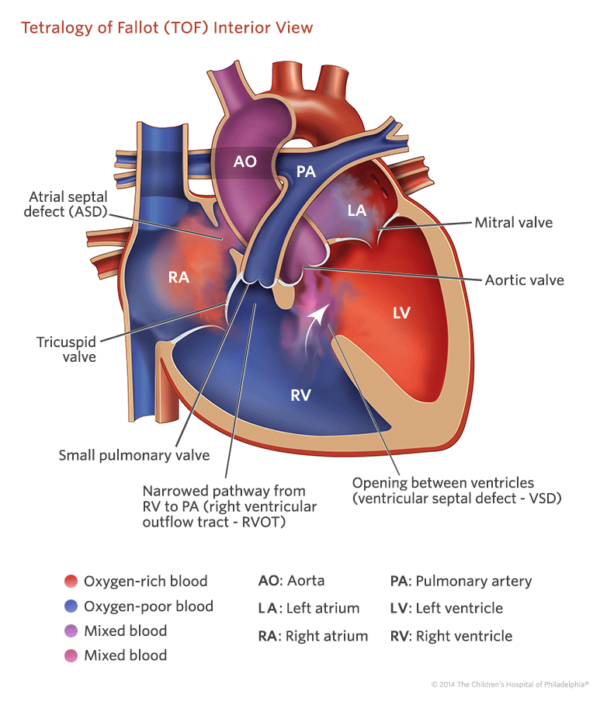
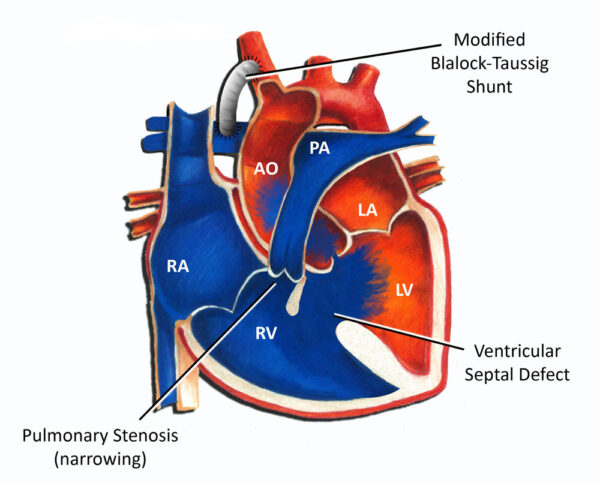
Tetralogy of Fallot (TOF) repair surgery is a procedure performed to correct a congenital heart defect known as Tetralogy of Fallot. TOF is characterized by a combination of four heart abnormalities: a ventricular septal defect (VSD), pulmonary stenosis (narrowing of the pulmonary valve and artery), an overriding aorta (the aorta is positioned over both ventricles), and right ventricular hypertrophy (thickening of the right ventricle).
The goal of TOF repair surgery is to improve blood flow to the lungs and alleviate the symptoms associated with the condition. The surgery is typically performed during infancy or early childhood, although it can also be done in adulthood if the condition was not corrected earlier.
During the procedure, the patient is placed under general anesthesia. The surgeon makes an incision in the chest to access the heart. The specific surgical technique may vary depending on the individual’s anatomy and the surgeon’s preference. The main steps of the surgery typically involve:
Closing the Ventricular Septal Defect (VSD): The surgeon closes the hole between the ventricles using a patch or sutures. This helps separate the oxygenated and deoxygenated blood, improving overall circulation.
Relieving Pulmonary Stenosis: The narrowed pulmonary valve and artery are widened to improve blood flow to the lungs. This can be achieved by removing obstructive tissue, enlarging the pulmonary valve, or using a patch to widen the artery.
Addressing Right Ventricular Hypertrophy: If the right ventricle has become thickened due to the increased workload, the surgeon may remove excess muscle tissue to restore normal thickness and function.
After the repairs are completed, the surgeon carefully checks for any residual leaks or obstructions and ensures that the heart is functioning properly. The incision is then closed, and the patient is moved to the recovery area.
Tetralogy of Fallot (TOF) repair surgery is suitable for individuals diagnosed with TOF, a congenital heart defect characterized by four specific abnormalities: ventricular septal defect (VSD), pulmonary valve stenosis, malposition of the aorta, and right ventricular hypertrophy.
The surgery is typically performed during the first year of life, although it can also be done in older children or adults if the condition was not corrected earlier. The goal of the surgery is to eliminate the shunting of blood across the ventricles and relieve the narrowing of the pulmonary valve, thereby improving blood flow to the lungs.
The suitability for TOF repair surgery depends on various factors, including the individual’s overall health, the severity of the condition, and the presence of any additional risk factors. In general, most infants with TOF can successfully undergo surgery in the first year of life, with a high success rate and improved long-term survival.
However, the surgical repair may be more challenging in cases where the pulmonary arteries are critically small or when the lung blood flow is predominantly supplied by aortopulmonary collaterals. In such situations, the surgical team may need to carefully evaluate the risks and benefits of the procedure.
While Tetralogy of Fallot (TOF) repair surgery is generally considered appropriate for most individuals with TOF, there may be certain cases where it is not suitable. The suitability for surgery depends on various factors, including the overall health of the individual, the severity of the TOF condition, and the presence of any additional risk factors. Here are some situations where TOF repair surgery may not be suitable:
Severe medical conditions: Individuals with severe medical conditions or comorbidities that make them too weak or medically unstable may not be suitable candidates for TOF repair surgery. The surgical team will assess the overall health of the individual to determine if they can tolerate the procedure and the associated anesthesia.
Extremely low birth weight: In cases where an infant with TOF has an extremely low birth weight, there may be concerns about their ability to withstand the surgery and the recovery process. The surgical team will carefully evaluate the risks and benefits in such situations.
Unfavorable anatomy: In some instances, the anatomy of the heart and blood vessels may make TOF repair surgery technically difficult or risky. This can include severely narrowed or absent pulmonary arteries, abnormal coronary artery anatomy, or complex associated heart defects. The surgical team will assess the specific anatomical considerations to determine the suitability for surgery.
Terminal illness: Individuals with terminal illnesses or limited life expectancy may not be suitable candidates for TOF repair surgery. The potential benefits of the surgery may be outweighed by the limited expected lifespan or quality of life.
Advantages of Tetralogy of Fallot (TOF) repair surgery include:
Improved quality of life: TOF repair surgery aims to correct the underlying heart defects, allowing for improved blood flow to the lungs and reducing symptoms such as cyanosis (bluish discoloration of the skin) and shortness of breath. This can significantly enhance the individual’s quality of life.
Prevention of complications: Repairing TOF helps prevent long-term complications associated with the condition. It can reduce the risk of end-organ damage caused by chronic cyanosis, such as polycythemia (increased red blood cell count) and clubbing of fingers. Additionally, it can prevent right ventricular hypertrophy and fibrosis, which can lead to heart failure if left untreated.
Preservation of heart function: TOF repair surgery aims to relieve the obstruction in the right ventricular outflow tract and minimize pulmonary regurgitation (backward flow of blood from the pulmonary artery to the right ventricle). By improving blood flow and reducing regurgitation, the surgery helps preserve the function of the right ventricle and overall heart function.
Long-term survival: Studies have shown that individuals who undergo TOF repair surgery have improved long-term survival rates compared to those who do not receive surgical intervention. The survival rates can vary depending on factors such as the age of surgery and the presence of additional risk factors, but overall, the surgery has been associated with favorable outcomes and increased life expectancy.
Development of pulmonary arteries and lungs: Early repair of TOF during infancy or childhood allows for better development of the pulmonary arteries and lungs. By relieving the obstruction and improving blood flow to the lungs, the surgery promotes the growth and maturation of these vital structures.
Complications associated with Tetralogy of Fallot (TOF) repair surgery can vary depending on individual factors and the specific case. Here are some potential complications that may arise:
Arrhythmias: Following TOF repair surgery, individuals may experience abnormal heart rhythms (arrhythmias). These can range from minor irregularities to more serious conditions that require medical intervention.
Residual defects: In some cases, there may be residual ventricular septal defects (VSDs) or other abnormalities present after TOF repair surgery. These residual defects may require further intervention or monitoring.
Pulmonary regurgitation: The surgical repair of TOF can sometimes result in pulmonary regurgitation, which is the backward flow of blood from the pulmonary artery to the right ventricle. This can lead to long-term complications such as right ventricular dilation and dysfunction.
Right ventricular dysfunction: The right ventricle may experience temporary or long-term dysfunction following surgery. This can be due to factors such as the previous hypertrophy (thickening) of the ventricle or the surgical incision made into the muscle of the ventricle.
Endocarditis: While the risk is reduced compared to individuals with uncorrected TOF, there is still a lifelong risk of endocarditis (infection of the heart’s inner lining) after TOF repair surgery. It is important to follow proper dental and medical hygiene practices and take antibiotics as prescribed by the healthcare provider.
Late postoperative complications: Late complications following TOF repair surgery can include the development of ventricular arrhythmias, which can lead to sudden death. However, it’s important to note that the overall risk of these complications is relatively low.
Prior to Tetralogy of Fallot (TOF) repair surgery, individuals with TOF may require ongoing medical care and management to optimize their health and prepare for the surgical intervention. Here are some aspects of previous care that may be involved:
Diagnosis and evaluation: TOF is typically diagnosed shortly after birth or during infancy through physical examination, imaging tests such as echocardiography, and possibly additional diagnostic procedures. The initial evaluation helps determine the severity of TOF and any associated abnormalities.
Medical management: Prior to surgery, individuals with TOF may require medical management to alleviate symptoms and optimize their health. This can include medications to manage cyanosis, improve heart function, and prevent complications such as infections.
Monitoring and follow-up: Regular monitoring and follow-up appointments with a cardiologist are essential to assess the individual’s condition and determine the appropriate timing for TOF repair surgery. This includes evaluating the growth and development of the individual, assessing the severity of TOF, and monitoring any changes in symptoms or heart function over time.
After Tetralogy of Fallot (TOF) repair surgery, individuals require postoperative care and monitoring to ensure proper healing and recovery. Here are some aspects of aftercare that may be involved:
Hospital stay: After TOF repair surgery, individuals typically spend a few days in the hospital for close monitoring and recovery. The length of the hospital stay can vary depending on factors such as the individual’s age, overall health, and any postoperative complications.
Pain management: Pain management is an important aspect of aftercare following TOF repair surgery. Medications may be prescribed to manage pain and discomfort during the recovery period. It’s important to follow the healthcare provider’s instructions regarding pain medication administration.
Monitoring vital signs: Healthcare professionals will closely monitor vital signs such as heart rate, blood pressure, and oxygen saturation levels to ensure stability and detect any potential complications.
Wound care: Proper wound care is essential to promote healing and prevent infection. The surgical incision site will need to be kept clean and dry. The healthcare team will provide instructions on how to care for the incision and when it is safe to remove any dressings or sutures.
Activity restrictions: Individuals may have activity restrictions following TOF repair surgery. The healthcare provider will provide guidance on gradually increasing activity levels and when it is safe to return to normal activities, including exercise and sports.
Medication management: Depending on the individual’s specific needs, medications may be prescribed after TOF repair surgery. This may include medications to prevent infection, manage pain, control blood pressure, or prevent blood clots. It’s important to take medications as prescribed and follow up with the healthcare provider regarding any concerns or side effects.
Follow-up appointments: Regular follow-up appointments with the healthcare provider, typically a cardiologist, are crucial to monitor the individual’s progress and assess the long-term outcome of the surgery. These appointments may involve physical examinations, imaging tests, and further evaluations to ensure proper healing and address any potential complications.
Lifestyle modifications: The healthcare provider may provide guidance on lifestyle modifications to support heart health and overall well-being. This can include recommendations for a heart-healthy diet, regular exercise, and strategies to manage any specific risk factors.
Only logged in customers who have purchased this product may leave a review.
Tetralogy of Fallot (TOF) repair surgery is a procedure performed to correct a congenital heart defect known as Tetralogy of Fallot. TOF is characterized by a combination of four heart abnormalities: a ventricular septal defect (VSD), pulmonary stenosis (narrowing of the pulmonary valve and artery), an overriding aorta (the aorta is positioned over both ventricles), and right ventricular hypertrophy (thickening of the right ventricle).
The goal of TOF repair surgery is to improve blood flow to the lungs and alleviate the symptoms associated with the condition. The surgery is typically performed during infancy or early childhood, although it can also be done in adulthood if the condition was not corrected earlier.
During the procedure, the patient is placed under general anesthesia. The surgeon makes an incision in the chest to access the heart. The specific surgical technique may vary depending on the individual’s anatomy and the surgeon’s preference. The main steps of the surgery typically involve:
Closing the Ventricular Septal Defect (VSD): The surgeon closes the hole between the ventricles using a patch or sutures. This helps separate the oxygenated and deoxygenated blood, improving overall circulation.
Relieving Pulmonary Stenosis: The narrowed pulmonary valve and artery are widened to improve blood flow to the lungs. This can be achieved by removing obstructive tissue, enlarging the pulmonary valve, or using a patch to widen the artery.
Addressing Right Ventricular Hypertrophy: If the right ventricle has become thickened due to the increased workload, the surgeon may remove excess muscle tissue to restore normal thickness and function.
After the repairs are completed, the surgeon carefully checks for any residual leaks or obstructions and ensures that the heart is functioning properly. The incision is then closed, and the patient is moved to the recovery area.
Tetralogy of Fallot (TOF) repair surgery is suitable for individuals diagnosed with TOF, a congenital heart defect characterized by four specific abnormalities: ventricular septal defect (VSD), pulmonary valve stenosis, malposition of the aorta, and right ventricular hypertrophy.
The surgery is typically performed during the first year of life, although it can also be done in older children or adults if the condition was not corrected earlier. The goal of the surgery is to eliminate the shunting of blood across the ventricles and relieve the narrowing of the pulmonary valve, thereby improving blood flow to the lungs.
The suitability for TOF repair surgery depends on various factors, including the individual’s overall health, the severity of the condition, and the presence of any additional risk factors. In general, most infants with TOF can successfully undergo surgery in the first year of life, with a high success rate and improved long-term survival.
However, the surgical repair may be more challenging in cases where the pulmonary arteries are critically small or when the lung blood flow is predominantly supplied by aortopulmonary collaterals. In such situations, the surgical team may need to carefully evaluate the risks and benefits of the procedure.
While Tetralogy of Fallot (TOF) repair surgery is generally considered appropriate for most individuals with TOF, there may be certain cases where it is not suitable. The suitability for surgery depends on various factors, including the overall health of the individual, the severity of the TOF condition, and the presence of any additional risk factors. Here are some situations where TOF repair surgery may not be suitable:
Severe medical conditions: Individuals with severe medical conditions or comorbidities that make them too weak or medically unstable may not be suitable candidates for TOF repair surgery. The surgical team will assess the overall health of the individual to determine if they can tolerate the procedure and the associated anesthesia.
Extremely low birth weight: In cases where an infant with TOF has an extremely low birth weight, there may be concerns about their ability to withstand the surgery and the recovery process. The surgical team will carefully evaluate the risks and benefits in such situations.
Unfavorable anatomy: In some instances, the anatomy of the heart and blood vessels may make TOF repair surgery technically difficult or risky. This can include severely narrowed or absent pulmonary arteries, abnormal coronary artery anatomy, or complex associated heart defects. The surgical team will assess the specific anatomical considerations to determine the suitability for surgery.
Terminal illness: Individuals with terminal illnesses or limited life expectancy may not be suitable candidates for TOF repair surgery. The potential benefits of the surgery may be outweighed by the limited expected lifespan or quality of life.
Advantages of Tetralogy of Fallot (TOF) repair surgery include:
Improved quality of life: TOF repair surgery aims to correct the underlying heart defects, allowing for improved blood flow to the lungs and reducing symptoms such as cyanosis (bluish discoloration of the skin) and shortness of breath. This can significantly enhance the individual’s quality of life.
Prevention of complications: Repairing TOF helps prevent long-term complications associated with the condition. It can reduce the risk of end-organ damage caused by chronic cyanosis, such as polycythemia (increased red blood cell count) and clubbing of fingers. Additionally, it can prevent right ventricular hypertrophy and fibrosis, which can lead to heart failure if left untreated.
Preservation of heart function: TOF repair surgery aims to relieve the obstruction in the right ventricular outflow tract and minimize pulmonary regurgitation (backward flow of blood from the pulmonary artery to the right ventricle). By improving blood flow and reducing regurgitation, the surgery helps preserve the function of the right ventricle and overall heart function.
Long-term survival: Studies have shown that individuals who undergo TOF repair surgery have improved long-term survival rates compared to those who do not receive surgical intervention. The survival rates can vary depending on factors such as the age of surgery and the presence of additional risk factors, but overall, the surgery has been associated with favorable outcomes and increased life expectancy.
Development of pulmonary arteries and lungs: Early repair of TOF during infancy or childhood allows for better development of the pulmonary arteries and lungs. By relieving the obstruction and improving blood flow to the lungs, the surgery promotes the growth and maturation of these vital structures.
Complications associated with Tetralogy of Fallot (TOF) repair surgery can vary depending on individual factors and the specific case. Here are some potential complications that may arise:
Arrhythmias: Following TOF repair surgery, individuals may experience abnormal heart rhythms (arrhythmias). These can range from minor irregularities to more serious conditions that require medical intervention.
Residual defects: In some cases, there may be residual ventricular septal defects (VSDs) or other abnormalities present after TOF repair surgery. These residual defects may require further intervention or monitoring.
Pulmonary regurgitation: The surgical repair of TOF can sometimes result in pulmonary regurgitation, which is the backward flow of blood from the pulmonary artery to the right ventricle. This can lead to long-term complications such as right ventricular dilation and dysfunction.
Right ventricular dysfunction: The right ventricle may experience temporary or long-term dysfunction following surgery. This can be due to factors such as the previous hypertrophy (thickening) of the ventricle or the surgical incision made into the muscle of the ventricle.
Endocarditis: While the risk is reduced compared to individuals with uncorrected TOF, there is still a lifelong risk of endocarditis (infection of the heart’s inner lining) after TOF repair surgery. It is important to follow proper dental and medical hygiene practices and take antibiotics as prescribed by the healthcare provider.
Late postoperative complications: Late complications following TOF repair surgery can include the development of ventricular arrhythmias, which can lead to sudden death. However, it’s important to note that the overall risk of these complications is relatively low.
Prior to Tetralogy of Fallot (TOF) repair surgery, individuals with TOF may require ongoing medical care and management to optimize their health and prepare for the surgical intervention. Here are some aspects of previous care that may be involved:
Diagnosis and evaluation: TOF is typically diagnosed shortly after birth or during infancy through physical examination, imaging tests such as echocardiography, and possibly additional diagnostic procedures. The initial evaluation helps determine the severity of TOF and any associated abnormalities.
Medical management: Prior to surgery, individuals with TOF may require medical management to alleviate symptoms and optimize their health. This can include medications to manage cyanosis, improve heart function, and prevent complications such as infections.
Monitoring and follow-up: Regular monitoring and follow-up appointments with a cardiologist are essential to assess the individual’s condition and determine the appropriate timing for TOF repair surgery. This includes evaluating the growth and development of the individual, assessing the severity of TOF, and monitoring any changes in symptoms or heart function over time.
After Tetralogy of Fallot (TOF) repair surgery, individuals require postoperative care and monitoring to ensure proper healing and recovery. Here are some aspects of aftercare that may be involved:
Hospital stay: After TOF repair surgery, individuals typically spend a few days in the hospital for close monitoring and recovery. The length of the hospital stay can vary depending on factors such as the individual’s age, overall health, and any postoperative complications.
Pain management: Pain management is an important aspect of aftercare following TOF repair surgery. Medications may be prescribed to manage pain and discomfort during the recovery period. It’s important to follow the healthcare provider’s instructions regarding pain medication administration.
Monitoring vital signs: Healthcare professionals will closely monitor vital signs such as heart rate, blood pressure, and oxygen saturation levels to ensure stability and detect any potential complications.
Wound care: Proper wound care is essential to promote healing and prevent infection. The surgical incision site will need to be kept clean and dry. The healthcare team will provide instructions on how to care for the incision and when it is safe to remove any dressings or sutures.
Activity restrictions: Individuals may have activity restrictions following TOF repair surgery. The healthcare provider will provide guidance on gradually increasing activity levels and when it is safe to return to normal activities, including exercise and sports.
Medication management: Depending on the individual’s specific needs, medications may be prescribed after TOF repair surgery. This may include medications to prevent infection, manage pain, control blood pressure, or prevent blood clots. It’s important to take medications as prescribed and follow up with the healthcare provider regarding any concerns or side effects.
Follow-up appointments: Regular follow-up appointments with the healthcare provider, typically a cardiologist, are crucial to monitor the individual’s progress and assess the long-term outcome of the surgery. These appointments may involve physical examinations, imaging tests, and further evaluations to ensure proper healing and address any potential complications.
Lifestyle modifications: The healthcare provider may provide guidance on lifestyle modifications to support heart health and overall well-being. This can include recommendations for a heart-healthy diet, regular exercise, and strategies to manage any specific risk factors.
There are no reviews yet.
Only logged in customers who have purchased this product may leave a review.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment. The preferred choice for many patients is choosing private care.
Choosing the right hospital and physician are important factors to consider that significantly influence a patient’s treatment.
Reviews
There are no reviews yet.