⭐ Top ECCE Hospitals 2026: Extracapsular Cataract Surgery Guide
📚 Executive Summary: Navigating ECCE Excellence
Choosing the right medical center for specialized ophthalmic procedures requires deep investigation. Extracapsular Cataract Extraction Surgery (ECCE) is no exception. Although modern techniques like phacoemulsification dominate routine practice, ECCE remains the indispensable, and often superior, surgical choice for complex cases. These cases involve extremely dense, hard cataracts or situations involving compromised lens support, known as zonular weakness. This comprehensive guide helps both patients and referring professionals identify the elite global facilities offering world-class Extracapsular Cataract Surgery in 2026. Therefore, we meticulously detail the non-negotiable criteria. These include surgeon volume, mastery of Small Incision Cataract Surgery (SICS), state-of-the-art diagnostic technology, and highly structured post-operative protocols focusing on astigmatism management. Finally, we explore regional centers, specifically highlighting countries like Iran, which consistently perform high-volume, expert ECCE and SICS with excellent outcomes.
Caption: Performing Extracapsular Cataract Extraction (ECCE) Surgery: This technique is crucial for managing hard cataracts and compromised zonules.
🔬 Understanding Extracapsular Cataract Surgery (ECCE) in Context
Before evaluating hospitals, patients must fully grasp the procedure. Extracapsular Cataract Extraction Surgery (ECCE) is a method where the surgeon removes the cloudy, natural lens (cataract) through a large surgical incision. However, the procedure carefully leaves the posterior capsule of the lens intact. This remaining capsule acts as a stable hammock, essential for supporting the new intraocular lens (IOL). Historically, ECCE was the gold standard, a massive leap in safety and effectiveness compared to the older Intracapsular Cataract Extraction (ICCE) method.
🔄 ECCE versus Phacoemulsification: Choosing the Right Tool
Most Western medical centers default to phacoemulsification, known simply as “phaco.” Phaco uses a tiny incision and ultrasound energy to break up the lens before aspiration. Conversely, Extracapsular Cataract Surgery uses a large incision (8-12 mm) for manual removal of the nucleus. Thus, while phaco offers faster recovery for routine cataracts, ECCE avoids the use of damaging ultrasound energy inside the eye. Therefore, for specific pathological conditions, ECCE is undoubtedly the safer, smarter choice.
🎯 Critical Indications Demanding ECCE Expertise
ECCE is far from obsolete; it is a specialty procedure. Top hospitals possess the expertise to perform ECCE when phaco carries unacceptable risks.
- ✓ Hypermature or Rock-Hard Cataracts: Extremely dense (brunescent or black) lenses require extensive ultrasonic power in phaco. This high energy generates heat and turbulence. Consequently, this excess energy risks irreversible damage to the corneal endothelial cells. ECCE, however, allows for manual, low-energy nucleus extraction.
- ✓ Compromised Zonular Integrity: Zonules are the delicate fibers holding the lens in place. When trauma, pseudoexfoliation syndrome, or certain genetic factors weaken these fibers, phaco maneuvers can destabilize the lens further. This creates a severe risk of the lens or fragments dropping into the vitreous cavity. ECCE and SICS provide a gentler, more controlled extraction, stabilizing the whole system.
- ✓ Low Endothelial Cell Count: The endothelium is a single layer of cells vital for corneal clarity. If a patient already exhibits a low cell count, an aggressive phaco procedure can push the count below a critical threshold, potentially leading to long-term corneal swelling and blindness. Therefore, protecting this layer is paramount in top ECCE centers.
🟢 Pros: Why ECCE Excels for Complex Cases
ECCE often proves safer when surgeons face significant pathology. For instance, the technique minimizes endothelial cell loss by avoiding high-energy ultrasound. Moreover, it offers superior control when managing zonular instability, directly addressing the core risks of complex cataract surgery. Furthermore, specialized centers have refined ECCE into the Small Incision Cataract Surgery (SICS) variant. SICS maintains ECCE’s core benefits while drastically reducing the incision size. The full form of ECCE represents a complete and comprehensive surgical solution.
🔴 Cons: Challenges and Mitigation by Top Hospitals
The primary drawback is the larger incision, requiring meticulous closure with sutures. This suturing is what introduces the risk of post-operative astigmatism. Consequently, visual recovery takes longer compared to sutureless phaco. However, leading hospitals actively mitigate this. Specifically, they utilize sophisticated suture materials, specialized wound construction techniques (like scleral tunnels), and aggressive post-operative management, including selective suture removal. Top ophthalmology departments view this post-op care as integral to the surgical success.

🏥 Criteria for Top ECCE Hospitals 2026 (Part 1: Expertise & Volume)
The true measure of a top Extracapsular Cataract Surgery center lies in its deliberate commitment to mastering *all* forms of cataract surgery, especially the most challenging ones. Therefore, patients should not simply look for a high-volume center, but rather one with a high *complex* case volume.
👨⚕️ Surgeon Mastery: The Art of Controlled Extraction
ECCE is often described as a surgeon’s operation; success depends entirely on manual skill, control, and judgment.
Volume Metrics and Conversion Proficiency
Top hospitals transparently track their surgeons’ case volumes. In particular, they monitor the volume of primary ECCE and SICS procedures. These numbers indicate consistent skill maintenance. Equally important, leading hospitals track the surgeon’s Phaco-to-ECCE conversion rate. A low, controlled conversion rate is a sign of excellent pre-operative planning. Conversely, a surgeon with the technical skill to *safely* convert a complicated phaco case to ECCE mid-procedure demonstrates superior surgical maturity and risk management. This skill set is a mandatory characteristic of a top ECCE surgeon. Furthermore, for those exploring different surgical options, understanding the entire general surgery landscape is useful.
SICS Mastery: The Next Evolution of ECCE
Manual Small Incision Cataract Surgery (SICS) is the modern refinement of ECCE. It uses a self-sealing, beveled scleral tunnel incision (typically 5.5-7 mm). Consequently, SICS often eliminates the need for sutures. This fusion of manual nucleus removal safety with a small, sutureless wound makes SICS the technique of choice in high-volume, global centers. A top hospital for Extracapsular Cataract Surgery must demonstrate proficiency in SICS. This expertise reduces induced astigmatism and accelerates visual recovery, offering patients the best of both worlds. Look for clinics that explicitly train for or perform SICS, often highlighted in their ophthalmology programs.
💻 Technological Infrastructure: Precision Diagnosis
While ECCE is manual, world-class diagnostics are essential for planning and successful execution. Therefore, sophisticated technology is a key differentiating factor.
Advanced Biometry and IOL Calculation
The larger incision in ECCE/SICS can slightly alter corneal curvature and affect IOL power calculation. Hence, pre-operative biometry cannot be standard. Leading hospitals use advanced optical biometers (like IOLMaster or Lenstar) for non-contact, high-precision axial length and keratometry measurements. Furthermore, they utilize modern formulas (e.g., Barrett Universal II, Haigis) to minimize refractive surprise. This attention to detail ensures the implanted lens provides the highest possible visual quality. Furthermore, centers must possess a wide selection of premium IOLs, including Toric IOLs, to proactively manage potential astigmatism.
Specular Microscopy and Endothelial Cell Health
As previously discussed, protecting the cornea is a main reason for choosing ECCE. Thus, a top hospital mandates specular microscopy for all complex cataract patients. This test gives a vital endothelial cell count and morphology analysis. When the count is low (e.g., <2000 cells/mm²), the decision to proceed with ECCE is reinforced. This commitment to pre-operative corneal health screening separates the best centers from the rest. Corneal transplantation becomes the last resort if this vital step is skipped.
🛡️ Criteria for Top ECCE Hospitals 2026 (Part 2: Safety & Aftercare)
Success in Extracapsular Cataract Surgery extends far beyond the operating room. Since this procedure involves a larger wound and sutures, long-term safety and dedicated post-operative care are essential pillars of quality.
🔒 Rigorous Safety and Infection Control
Any surgical procedure carries risks, but a high-quality institution actively minimizes them through protocol.
Reducing the Risk of Endophthalmitis
Infection following cataract surgery (endophthalmitis) is rare but devastating. Because the ECCE incision is larger than phaco’s, top centers enforce particularly stringent protocols. Therefore, they mandate pre-operative povidone-iodine antisepsis and often inject antibiotics into the anterior chamber at the end of the case. Furthermore, these hospitals maintain clean room standards certified by international bodies. When researching, patients should inquire about the center’s specific infection rate for ECCE/SICS—the best facilities track and openly report this metric.
Long-Term Outcome Tracking and Auditing
True excellence requires data. Leading hospitals participate in national or international registries, meticulously tracking visual outcomes. Specifically, they record the percentage of ECCE patients who achieve a best-corrected visual acuity (BCVA) of 20/40 or better at three months and one year post-surgery. This transparent, long-term follow-up demonstrates an unwavering commitment to patient results, moving beyond just successful surgery completion. This is a characteristic of all excellent global medical tourism centers.
🩹 Post-Operative Management: Conquering Astigmatism
The sutured wound is the biggest challenge of traditional ECCE recovery. Successfully managing the induced astigmatism is the final, decisive step.
The Critical Role of Selective Suture Cutting
The large incision can cause the cornea to flatten or steepen, leading to astigmatism. Consequently, top surgeons perform selective suture removal starting a few weeks post-op. Using corneal topography maps, they identify the tightest sutures and cut only those that cause the most distortion. This iterative process is a critical skill that dramatically improves the patient’s final uncorrected vision. Simply put, if a hospital lacks this dedicated expertise, they cannot guarantee optimal visual outcomes following ECCE. Therefore, inquire about their post-operative ophthalmologist follow-up schedule.
Extended Care for International Patients
For patients seeking Extracapsular Cataract Surgery abroad, the hospital must offer specialized support. Recovery from a sutured ECCE requires an extended stay for safe suture removal and refraction adjustments. The best centers facilitate this. For example, they coordinate long-term accommodation, provide resources for a medical visa, and offer remote telemedicine follow-up once the patient returns home. This holistic approach ensures safety throughout the patient journey.
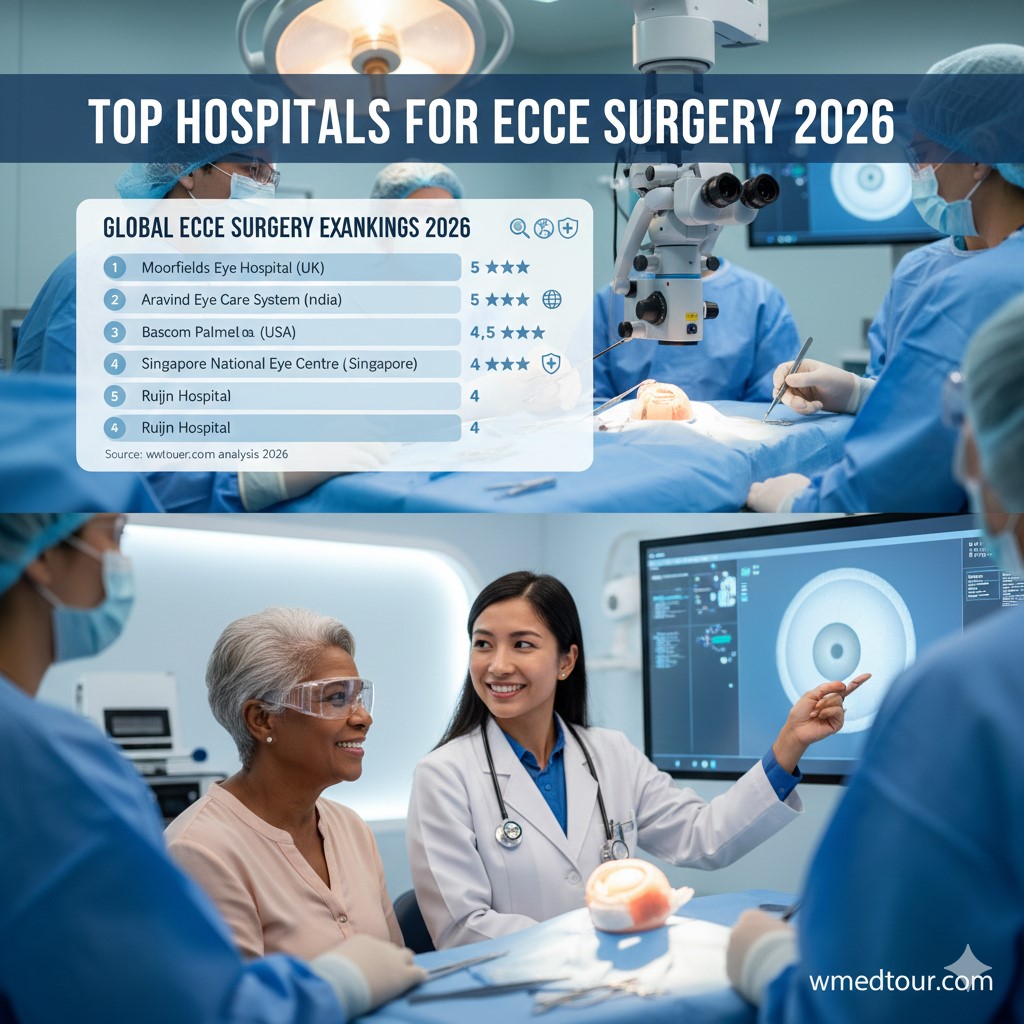
🌍 Global Leaders: High-Volume ECCE Centers in 2026
The global landscape for ECCE expertise often reflects the prevalence of advanced cataracts and the commitment of institutions to surgical education. Consequently, certain regions maintain an exceptional level of proficiency in manual cataract techniques.
SICS Dominance in Asia and the Middle East
Many countries in Asia and the Middle East, particularly those with comprehensive public health programs, have perfected SICS (Small Incision Cataract Surgery). They perform SICS on patients who often present with more advanced cataracts than those seen in the West. Therefore, their surgeons maintain incredibly high volumes and technical refinement in manual cataract surgery.
Iran: A Center of Excellence for ECCE/SICS
When comparing countries for high-quality, high-volume ECCE, one must mention Iran. Iran’s healthcare system, particularly its renowned Ophthalmology Departments, has prioritized the refinement of manual techniques like SICS alongside phacoemulsification. The combination of expert, fellowship-trained surgeons and a patient base with varying cataract maturities has led to world-class proficiency in Extracapsular Cataract Surgery. The hospitals, such as those in Tehran or Mashhad (like Razavi Hospital), often provide this high level of surgical expertise at an affordable cost, making Iran a premier destination for complex ophthalmic procedures, supported by streamlined medical travel regulations.
Comparison of Global ECCE/SICS Expertise
| Institution Type & Region | Annual ECCE/SICS Volume | Key Focus & Technique | Post-Op Astigmatism Management |
|---|---|---|---|
| Asia/Middle East High-Volume Center (e.g., Iran) | 1,500+ | Primary SICS for dense/hypermature cataracts. | Aggressive, high-volume suture adjustment and YAG laser capsulotomy. |
| University Teaching Hospital (USA/Europe) | 100-200 | Primary ECCE used as a conversion safety net for phaco complications. | Advanced topography-guided laser adjustments; often slower suture removal. |
| Specialized Global Ophthalmic Clinic (Turkey, India) | 300-500 | Refined SICS with premium IOL capability and Toric lens use. | Focus on minimal induced astigmatism through meticulous wound construction. |
Note: Volume figures represent ECCE/SICS, often an indicator of the surgeon’s readiness for complex cases.
📝 Patient Journey: Extracapsular Cataract Surgery in Practice
Consider Mr. Hamza, a 75-year-old patient from Canada diagnosed with a Grade 4 brunescent (very hard, brown) cataract. His local surgeon, highly skilled in routine phaco, advised against the procedure, noting Mr. Hamza’s borderline corneal endothelial cell count. The risk of corneal decompensation using high-energy ultrasound was simply too great. Consequently, Mr. Hamza sought a specialist facility abroad, leading him to a top ECCE center in the Middle East, known for its SICS proficiency.
Specialized Assessment and SICS Procedure
Upon arrival, the team conducted a specialized workup. This included an updated endothelial cell count and detailed corneal topography. The assessment confirmed that SICS, a variant of Extracapsular Cataract Surgery, was the safest option. The surgeon, an expert in SICS, created a self-sealing scleral tunnel incision. This maneuver allowed them to manually express the hard nucleus with minimal trauma to the cornea and surrounding tissues. Since the SICS incision was expertly constructed, the procedure required minimal to no sutures. The use of a specialized technique significantly reduced the likelihood of post-operative astigmatism, accelerating his visual rehabilitation.
Rapid Recovery for a Complex Case
Mr. Hamza noticed significant visual improvement within days, much faster than traditional ECCE. The lack of sutures meant the cornea stabilized quickly. By one month, his visual acuity was 20/30 uncorrected, a phenomenal result for such a hard cataract. He received detailed post-operative instructions for his travel back home, along with a schedule for remote follow-up. In contrast, a failed phaco attempt would have required complex secondary procedures like corneal transplantation. This outcome underscores the value of choosing a hospital where the surgeon possesses the full spectrum of cataract techniques, prioritizing patient safety over trend. This checklist can help choose a surgeon.
👤 Who is This Extracapsular Cataract Surgery Guide For?
The information within this guide is critical for individuals and professionals in several distinct scenarios. These specialized centers should be the first point of contact for these patient groups.
Target Patient Profiles for ECCE/SICS Referral
- The Challenging Cataract Patient: Individuals diagnosed with Grade 4 or 5 rock-hard, brunescent cataracts. Specifically, these patients need a surgeon who can manually remove the nucleus to protect the cornea.
- The Patient with Corneal Compromise: Anyone with pre-existing Fuchs’ endothelial dystrophy, low endothelial cell counts, or a history of prior corneal surgery. For this group, low-energy surgery is not a preference; it is a clinical necessity.
- The Traumatized Eye Patient: Patients who have sustained ocular trauma resulting in zonular weakness or lens subluxation. Therefore, they require the gentle stability offered by Extracapsular Cataract Surgery or SICS to prevent severe complications like vitreous loss or dropped nucleus.
- Medical Tourists Seeking Specialized Value: Individuals seeking a high-volume, cost-effective, and expertly performed SICS procedure in global centers like Iran, Turkey, or India, where the cost of eye surgery is often lower without compromising quality.
Guidance for Referring Professionals
For ophthalmologists and general practitioners, this guide serves as a referral reference. If a patient presents with a hard cataract or zonular instability, referring them to a center specializing in ECCE/SICS proficiency becomes the highest standard of care. This decision protects the patient from potentially devastating corneal and retinal complications associated with converting a complex phaco case. In addition, professionals should familiarize themselves with the full range of ophthalmic procedures available globally.
💡 Credibility and Innovation: Advancements in ECCE
Despite being a “traditional” method, top hospitals continually innovate their Extracapsular Cataract Surgery protocols. They integrate modern diagnostic tools and surgical techniques to improve safety and refractive outcomes.
Surgical Refinements: Reducing Astigmatism Risk
The biggest advancement in ECCE has focused on wound construction. For example, the modern scleral tunnel incision is meticulously designed to be self-sealing and astigmatically neutral, or even astigmatism-reducing. Furthermore, surgeons today use advanced, small-gauge irrigation and aspiration systems for cortical cleanup. Consequently, this minimizes posterior capsule stress, enhancing safety compared to older techniques. The evolution of ECCE wound architecture is well-documented in ophthalmic literature (Source: LWW), demonstrating that top centers constantly adopt these refinements.
The Importance of Comprehensive Backup Systems
A true top ECCE hospital maintains immediate access to a full suite of backup equipment. This includes a fully functional vitrectomy unit and a retina specialist on standby. Since ECCE is often performed on eyes with compromised stability, a rare but critical complication is vitreous prolapse. Immediate, expert management is essential for preserving the final visual outcome. The American Academy of Ophthalmology details the importance of such management (Source: AAO). Therefore, the hospital’s ability to seamlessly manage intra-operative complications defines its safety profile. Patients planning for complex surgeries should review the hospital’s entire range of medical departments.
✅ Conclusion: Prioritizing Expertise Over Standard Practice
The search for the Top ECCE Hospitals 2026: Extracapsular Cataract Surgery Guide leads inevitably to a focus on specialized, comprehensive care. While phacoemulsification remains the standard for routine cases, ECCE, and its SICS variant, stand as the indispensable choice for the most challenging cataracts and eyes with structural compromise. Therefore, the best hospitals distinguish themselves through rigorous surgeon training, high SICS volume, precise diagnostic technology (especially corneal mapping and cell counting), and sophisticated post-operative care, particularly for managing astigmatism. Ultimately, choosing a center proficient in Extracapsular Cataract Surgery guarantees the safest, most expert path to visual rehabilitation for complex eye conditions, securing the best possible long-term result. This commitment to having the right tool for every job defines global ophthalmic excellence. For those planning a medical journey, consulting the medical tourism guide is the next best step.
❓ Frequently Asked Questions (FAQ) about Extracapsular Cataract Surgery
1. Is Extracapsular Cataract Extraction (ECCE) still a relevant surgery in modern ophthalmology?
Yes, absolutely. ECCE remains a vital and necessary technique, not as the primary choice for routine cataracts, but as the gold standard for specific challenging conditions, ensuring that top surgeons can handle the entire spectrum of cataract pathology.
2. What specific patient conditions make ECCE the superior choice over Phacoemulsification?
ECCE is superior for patients with Grade 4 or 5 brunescent (rock-hard) cataracts, significant zonular weakness (compromised lens support), or very low pre-operative corneal endothelial cell counts. In these scenarios, the manual, low-energy nucleus extraction of ECCE is much safer than the high-energy ultrasound of phaco.
3. How does a surgeon’s conversion rate to ECCE indicate the quality of a top hospital?
A surgeon’s ability to safely and cleanly convert an intended phaco procedure into ECCE mid-surgery is a sign of superior surgical judgment and technical versatility. While a high *planned* ECCE volume is good, the skill to execute a safe conversion when a complication arises is a key safety indicator for any leading eye hospital.
4. What is Manual Small Incision Cataract Surgery (SICS) and how does it relate to ECCE?
SICS is a modern, highly refined variant of ECCE. It employs the same principle of manual nucleus removal but uses a smaller (5.5-7 mm), self-sealing scleral tunnel incision instead of the larger (8-12 mm) limbal incision of traditional ECCE. This crucial difference allows SICS to be sutureless or require fewer sutures, significantly reducing induced astigmatism and speeding recovery.
5. Why is corneal endothelial cell counting so critical for an ECCE candidate?
The corneal endothelium is responsible for keeping the cornea clear. Ultrasonic energy from phaco can damage these cells. When a patient already has a low cell count, the safer, lower-energy ECCE technique is chosen specifically to protect the remaining cells and prevent long-term corneal swelling (edema) or failure.
6. How long does visual recovery typically take after a properly performed Extracapsular Cataract Surgery?
Visual recovery is slower than phaco. While initial functional vision returns within days, full visual stability and the final, best-corrected vision often require several weeks to months. This is because the eye needs time to stabilize after the large incision and to allow for any necessary selective suture removal to correct astigmatism.
7. What role does selective suture cutting play in the final visual outcome of ECCE?
Selective suture cutting is a non-negotiable step in high-quality ECCE aftercare. The surgeon uses corneal topography to pinpoint sutures causing the most corneal distortion. By removing only those specific sutures, they precisely neutralize the induced astigmatism, which is essential for achieving the patient’s best possible uncorrected visual acuity.
8. How do top global hospitals manage the risk of infection (endophthalmitis) after a large-incision ECCE?
They employ maximum prophylactic measures. This includes mandatory application of povidone-iodine before surgery, the use of sterile drapes, and the injection of an antibiotic into the anterior chamber (intracameral antibiotics) at the conclusion of the surgery to prevent bacteria from entering through the larger wound.
9. Which regions of the world specialize in high-volume, expert Extracapsular Cataract Surgery?
Countries and institutions in the Middle East and South Asia, such as Iran, India, and Turkey, have historically maintained high proficiency. They see a greater number of hypermature cataracts and have perfected SICS as a cost-effective, high-quality, and reliable solution, making them top destinations for this specific skill set.
10. Can a patient receive premium intraocular lenses (IOLs) with an ECCE procedure?
Yes, but it is less common. The advantage of ECCE is the intact capsule, which supports a posterior chamber IOL. However, due to the higher risk of surgically induced astigmatism from the large incision, most surgeons prefer standard monofocal or toric IOLs, as highly sensitive lenses (like multifocals) require near-perfect corneal stability.
11. What specific diagnostic technology should a top hospital use before recommending Extracapsular Cataract Surgery?
A top hospital uses optical biometers for IOL calculation, specular microscopy for endothelial cell count, and corneal topography. Corneal topography is vital as it provides a detailed map of the corneal curvature, allowing the surgeon to plan the incision and suture placement to minimize post-operative astigmatism.
12. What is the difference between a Limbal incision and a Scleral Tunnel incision in ECCE?
A Limbal incision is made at the junction of the cornea and sclera (the white of the eye), which typically requires numerous sutures and is more prone to induced astigmatism. A Scleral Tunnel incision is made further back in the sclera and enters the anterior chamber through a beveled tunnel, creating a sturdier, self-sealing wound that often needs fewer or no sutures, characteristic of the SICS technique.
13. How do hospitals ensure quality control and long-term success data for their ECCE procedures?
Top hospitals participate in surgical quality registries, audit their cases against international benchmarks, and rigorously track patient-reported outcomes (PROMs) and objective visual acuity metrics (BCVA). They regularly review this data to refine their surgical protocols, suture techniques, and post-operative care standards.