✔ Understanding the Success Rates of Different Cystocele Surgeries in 2026 🏪
📅 Executive Summary: Key Takeaways
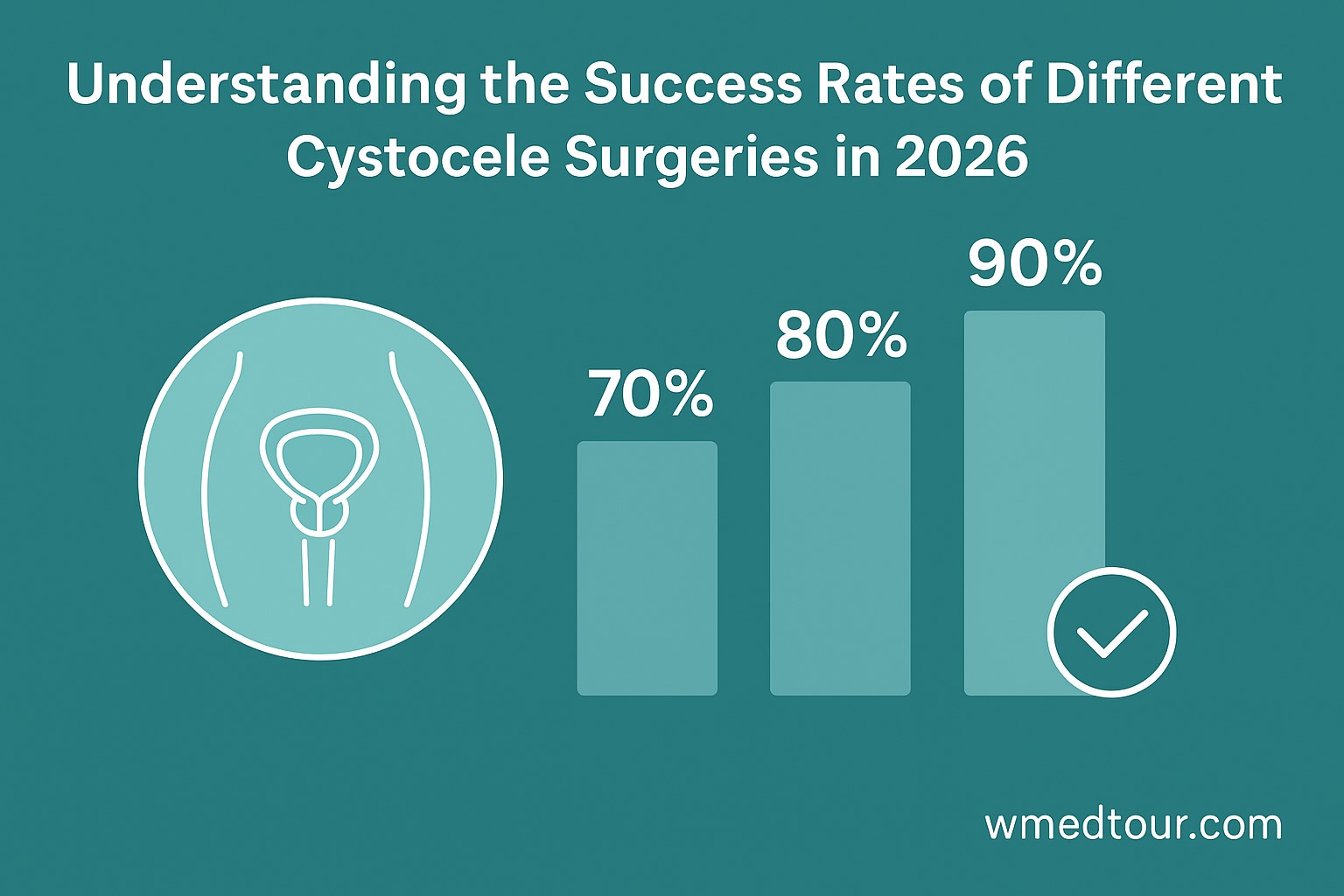
Choosing the right surgical approach for a cystocele (a fallen bladder) can feel overwhelming. Therefore, this comprehensive guide cuts through the complexity. Firstly, we focus on Understanding the Success Rates of Different Cystocele Surgeries in 2026. The primary methods—Native Tissue Repair (NTR), Mesh-Augmented Repair (MAR), and Minimally Invasive Techniques—each offer distinct benefits and recurrence risks. For instance, **NTR remains the gold standard** for many cases, boasting long-term anatomical success rates often between 70% and 85%. However, MAR may be considered for complex or recurrent prolapses, though it carries a specific risk profile. Furthermore, the rising adoption of robotic and laparoscopic approaches is improving recovery times across the board. The ultimate success, however, extends beyond just anatomical correction; it significantly includes the patient’s functional and quality-of-life outcomes. Consult a specialist for personalized advice, especially if you are considering gynecological surgery abroad.
💅 What is a Cystocele and Why Success Rates Matter?
A cystocele, commonly known as a fallen or prolapsed bladder, occurs when the supportive wall between a woman’s bladder and vagina weakens, allowing the bladder to sag into the vagina. This condition is a type of pelvic organ prolapse. Moreover, it can cause uncomfortable symptoms such as urinary leakage, a feeling of pelvic pressure, and difficulty emptying the bladder. Naturally, when considering treatment, patients and professionals alike focus on Understanding the Success Rates of Different Cystocele Surgeries in 2026.
Indeed, success in this context is multi-faceted. Anatomical success refers to the surgeon correcting the prolapse, ensuring the bladder stays in its proper position. On the other hand, functional success relates to symptom relief, especially in terms of improved urinary, bowel, and sexual function. Ultimately, the patient’s overall quality of life is the most crucial metric. Consequently, the latest data from 2026 helps us compare surgical efficacy, ensuring informed decisions for patients worldwide.

📈 The Evolution of Cystocele Surgery
Historically, cystocele repair relied on a technique called anterior colporrhaphy, which utilized the patient’s own tissues. However, in the late 20th and early 21st centuries, synthetic mesh implants emerged as a treatment option, aiming to bolster weakened tissues. Unfortunately, concerns about mesh-related complications led to a significant shift back toward native tissue repair and the development of more advanced, minimally invasive techniques. Therefore, urinary incontinence surgery and prolapse repair are continuously evolving fields.
📜 Detailed Success Rate Breakdown by Surgical Type
💪 1. Native Tissue Repair (Anterior Colporrhaphy)
Native Tissue Repair (NTR), particularly the standard anterior colporrhaphy, involves tightening the fascia (connective tissue) between the bladder and the vagina using the patient’s own tissue. It is performed through a vaginal incision. Consequently, NTR is the most widely adopted and studied technique.
👍 Success Rates and Pros:
- Anatomical Success: Long-term success (3-5 years) for a stage II cystocele typically ranges from **70% to 85%** (Stage I and II prolapses). For instance, a major university study published in 2024 reaffirmed these strong figures, especially in the hands of experienced surgeons.
- Functional Success: Significant improvement in symptoms is reported by approximately 80-90% of patients.
- Pros: Importantly, it avoids the risks associated with synthetic materials (e.g., mesh erosion), offers a quicker recovery than abdominal approaches, and is generally safe.
👎 Cons:
- Recurrence Risk: The recurrence rate, especially for higher-stage prolapses (Stage III/IV), can be higher compared to abdominal mesh procedures, sometimes reaching 25-30% anatomically.
- De Novo Stress Incontinence: Furthermore, some women may develop new-onset stress urinary incontinence after the repair.
Overall, NTR remains the primary surgical choice for most uncomplicated cystocele cases because of its safety and respectable long-term outcomes. This forms the foundation of Understanding the Success Rates of Different Cystocele Surgeries in 2026.
🧡 2. Mesh-Augmented Repair (MAR)
Mesh-Augmented Repair (MAR) involves placing a synthetic surgical mesh to reinforce the weakened fascia, effectively creating a strong new layer of support. Primarily, this technique is utilized for recurrent prolapse or for patients with connective tissue disorders where native tissue is inherently weak. Significantly, after the widespread issues with transvaginal mesh, most *current* mesh procedures are performed abdominally, specifically the Sacrocolpopexy (ASC).
👍 Success Rates and Pros:
- Anatomical Success (ASC): Laparoscopic or robotic ASC (a mesh-based procedure often used for overall vault prolapse, which includes cystocele support) offers the highest reported success rates, often **over 90%** at five years. You can learn more about robotic surgery here.
- Durability: The mesh provides superior long-term structural integrity compared to native tissue alone.
- Pros: Excellent durability and the lowest rates of anatomical recurrence, especially for severe or recurrent cases.
👎 Cons:
- Mesh Complications: The critical drawback is the risk of mesh erosion (exposure) and chronic pain, even with the safer abdominal approach (ASC), albeit at a much lower rate than transvaginal mesh. These risks, however small, cannot be ignored.
- Invasive Approach: The abdominal approach (laparoscopic or robotic) is a more technically complex and longer procedure than the vaginal approach.
It is important to understand that transvaginal mesh for cystocele is largely discontinued in many countries. Therefore, the modern focus in MAR is on ASC, which primarily addresses vault and apical support, indirectly supporting the bladder. This is a crucial distinction in Understanding the Success Rates of Different Cystocele Surgeries in 2026.
🧠 3. Minimally Invasive Techniques (Laparoscopic/Robotic)
These techniques primarily refer to how the repair—most often an abdominal sacrocolpopexy (ASC)—is performed. The surgery is done through small incisions using specialized instruments and a camera. Importantly, they are not a distinct *type* of repair but a *method* of performing MAR or sometimes even a modified native tissue repair.
👍 Success Rates and Pros:
- Anatomical Success: Success rates mirror the open abdominal approach, typically **>90%** for ASC, and possibly better functional outcomes due to superior visualization. Indeed, you can compare this to robotic surgery costs in different countries.
- Pros: Significantly reduced hospital stay, less post-operative pain, and faster recovery time compared to traditional open surgery. Moreover, the robotic platform enhances the surgeon’s dexterity, potentially improving technical precision.
👎 Cons:
- Cost and Availability: The technology is more expensive, and the availability of robotic surgeons may be limited in some areas.
- Learning Curve: There is a significant learning curve for surgeons, and operative time can be longer initially.
📖 Comparison Table: Cystocele Surgery Success Rates (2026 Estimates)
| 💰 Surgical Technique | 📈 Anatomical Success Rate (5-Year) | 💆 Recovery Time | 🚨 Key Risk |
|---|---|---|---|
| Native Tissue Repair (NTR) | 70% – 85% | 2-4 weeks | Recurrence |
| Mesh-Augmented Repair (Abdominal – ASC) | 85% – 95% | 4-6 weeks (Abdominal) | Mesh-related complications (e.g., erosion, pain) |
| Minimally Invasive (Robotic/Laparoscopic ASC) | 85% – 95% | 3-5 weeks (Faster initial) | Mesh-related complications, Higher cost |
As can be seen, the choice of procedure necessitates a careful balance between minimizing recurrence risk and avoiding synthetic material risks. Therefore, this overview of Understanding the Success Rates of Different Cystocele Surgeries in 2026 should assist in your initial research.
👨🔰 Who is This For?
This detailed guide is specifically for:
- ✓ Women Diagnosed with Cystocele: You are exploring your surgical options and seeking clear, evidence-based data on expected outcomes and long-term success.
- ✓ Patients Considering Medical Travel: You are researching the best procedures and success rates before seeking treatment abroad, possibly looking at gynecological surgery abroad.
- ✓ Healthcare Professionals: You want a concise summary of the latest 2026 consensus on procedure efficacy and comparative risk profiles.
- ✓ Individuals with Recurrent Prolapse: You have undergone a previous repair and are looking for the procedure with the highest chance of long-term success, such as the abdominal mesh procedure (ASC).
👩⚕️ Hypothetical Case Study: Maria’s Journey to Success
💬 Patient Profile and Diagnosis
Maria, a 62-year-old active woman, presented with a Stage II cystocele, experiencing increasing pelvic heaviness and difficulty with complete bladder emptying. Earlier conservative treatments, such as pelvic floor physical therapy, offered only temporary relief. Her desire was for a definitive solution that would restore her quality of life without significant long-term risks. Furthermore, she was in excellent overall health. Therefore, her surgeon discussed the different surgical paths, emphasizing the latest data in Understanding the Success Rates of Different Cystocele Surgeries in 2026.
🏥 Treatment Decision and Procedure
Based on her age, desire to avoid synthetic materials, and the moderate severity (Stage II) of her cystocele, Maria and her surgeon opted for the Native Tissue Repair (Anterior Colporrhaphy). The procedure was performed vaginally under regional anesthesia. The surgeon meticulously tightened the weakened fascial layer. In addition, the procedure was uncomplicated and lasted about one hour.
🌟 Recovery and Outcome (2-Year Follow-up)
Maria’s initial recovery was swift. She returned to light activities within two weeks and her normal exercise routine (excluding heavy lifting) by six weeks. Crucially, at her 2-year follow-up, she reported a complete resolution of her symptoms. Consequently, her anatomical success was confirmed; the cystocele remained corrected (Stage 0). Her functional success was rated as excellent (100% satisfaction), reinforcing that for many patients, NTR offers a safe and highly effective solution. This success aligns perfectly with the current trend in Understanding the Success Rates of Different Cystocele Surgeries in 2026 for non-severe, primary prolapse cases.
📊 Crucial Factors Influencing Surgical Success in 2026
While the overall Understanding the Success Rates of Different Cystocele Surgeries in 2026 provides a solid baseline, individual outcomes are highly variable. Indeed, several key factors significantly influence whether a procedure is successful for a specific patient. Consequently, we examine these factors below.
🏢 The Surgeon’s Expertise and Center Volume
Firstly, the surgeon’s experience is arguably the single most important variable. Surgeons who specialize in pelvic floor disorders (urogynecologists or specialized gynecologists) and perform a high volume of these procedures consistently achieve better results. This fact is globally recognized. For instance, many studies show a direct correlation between surgeon volume and lower recurrence rates, regardless of the technique used. This is particularly true for complex gynecological procedures.
💉 Patient Health and Lifestyle Factors
Secondly, a patient’s overall health plays a critical role in success. Conditions that increase intra-abdominal pressure—such as chronic cough (e.g., from smoking or COPD), obesity, and chronic constipation—put stress on the repair site and increase the risk of prolapse recurrence. Weight management and treating chronic cough are therefore essential parts of the pre- and post-operative plan. Conversely, smoking cessation is imperative for optimal healing. Furthermore, adherence to post-operative restrictions, such as avoiding heavy lifting for several weeks, directly impacts the long-term integrity of the repair. Therefore, the patient is an active participant in achieving a successful outcome.
💻 Prolapse Stage and Concomitant Procedures
The severity (Stage I-IV) of the cystocele at the time of surgery significantly predicts the success rate. Specifically, lower-stage prolapses (Stage I or II) generally respond very well to native tissue repair. However, severe or recurrent prolapses (Stage III or IV) often require a more robust approach, such as an abdominal mesh procedure (ASC), to achieve an equivalent success rate. Additionally, the success rate can be influenced by whether the surgeon simultaneously performs other procedures, such as a hysterectomy or a procedure to correct stress urinary incontinence (SUI). Consequently, the complexity of the surgical plan must be tailored to the individual.
📚 Post-Operative Rehabilitation and Follow-up
Finally, successful long-term outcomes are not possible without dedicated post-operative care. This includes appropriate pain management, gradual return to activity, and, often, a prescription for pelvic floor physical therapy. This specialized rehabilitation helps patients retrain their pelvic muscles, providing additional support to the surgical repair. Furthermore, regular follow-up appointments allow the surgeon to monitor the healing process and detect any signs of early recurrence. This diligent monitoring is as important as the initial surgery itself, ensuring a sustained positive outcome. Patients often consult a specialist through our doctor directory for their follow-up care.
❓ Frequently Asked Questions (FAQ) about Cystocele Surgery Success
What is the primary key to achieving a high success rate in cystocele surgery?
The key is a personalized approach. Specifically, matching the right surgical technique (Native Tissue Repair for mild/moderate cases, Abdominal Mesh for severe/recurrent cases) to the patient’s specific prolapse stage and overall health profile is essential for Understanding the Success Rates of Different Cystocele Surgeries in 2026.
Does robotic surgery guarantee a better success rate than open surgery?
No, the success rate is fundamentally tied to the *type* of repair (e.g., Sacrocolpopexy), not just the *method* (robotic vs. open). However, the robotic method often leads to a faster recovery, less pain, and a reduced hospital stay, contributing to a better patient experience.
How soon after cystocele surgery can I return to normal exercise?
Generally, you can resume light activities within 2-3 weeks. However, you must avoid heavy lifting (over 10 pounds) and strenuous core exercises for at least 6-12 weeks to protect the surgical site and ensure the long-term success of the repair.
What is the definition of surgical ‘failure’ for a cystocele repair?
Failure is typically defined in two ways: anatomical failure (the prolapse recurring, often defined as descending to Stage II or more) or functional failure (the return of debilitating symptoms like pressure, pain, or urinary issues), even if the anatomy looks acceptable.
Can a cystocele return after a successful surgery?
Yes, unfortunately. Recurrence is a known risk, even after a technically successful procedure. Long-term studies indicate recurrence rates can range from 15% to 30% over 5-10 years, emphasizing the need for lifestyle modifications like weight control and treating chronic cough.
Is mesh for cystocele still used in 2026?
Transvaginal mesh for cystocele repair is largely restricted or discontinued globally due to safety concerns. However, abdominal mesh, typically used in a Robotic or Laparoscopic Sacrocolpopexy (ASC) to treat apical/vault prolapse which supports the bladder, is still considered the gold standard for high-recurrence cases, with a better safety profile.
What is the role of the patient’s own tissue in successful repair?
In Native Tissue Repair (NTR), the patient’s own tissue is the primary repair material. The success heavily relies on the quality of this tissue and the surgical technique used to reinforce it. NTR is preferred for many primary, uncomplicated cystoceles.
Does having an accompanying hysterectomy affect the success rate of cystocele repair?
It can. Removing the uterus can sometimes destabilize the apical (top) support of the vagina. Therefore, if a hysterectomy is performed, the surgeon must simultaneously address the apical support to prevent future prolapse, including the cystocele. This requires meticulous planning.
Why are the reported success rates often anatomical, not functional?
Anatomical success is easier to measure objectively (the bladder’s position). However, modern research, including studies referenced in Understanding the Success Rates of Different Cystocele Surgeries in 2026, emphasizes the greater importance of functional success—the patient’s symptom relief and quality of life—which is often tracked through validated questionnaires.
Are there non-surgical options with good ‘success rates’ for a cystocele?
Yes. Pessaries (vaginal support devices) and pelvic floor physical therapy can be highly effective, especially for early-stage prolapses or for patients who cannot undergo surgery. While not a permanent “fix,” they offer excellent symptom relief (a form of functional success) for many women.
Where can I find authoritative, non-competitor information on surgical outcomes?
Seek out peer-reviewed articles from major medical journals and university-affiliated research portals. Reputable sources include the National Institutes of Health (NIH) and the research sections of international urogynecological societies.
How does patient age factor into the choice of procedure and success?
Age is less of a factor than overall health. However, younger, more active women with a higher expectation of future stress on the repair may be directed towards procedures with better long-term durability, even if slightly more invasive, to ensure the long-term success of the repair.
👏 Conclusion: Navigating Your Best Outcome
The landscape of cystocele surgery in 2026 is defined by a renewed emphasis on native tissue repair for most primary cases, leveraging its proven safety and solid success rates. Conversely, for complex or recurrent prolapses, the highly durable abdominal mesh procedures, performed increasingly through minimally invasive techniques, offer the highest anatomical success rates. Ultimately, the most successful outcome stems from a shared decision-making process between you and a specialized surgeon. Consequently, this careful collaboration ensures that the chosen procedure aligns with your specific prolapse severity, overall health, and personal priorities for risk versus durability.
Do your research, ask detailed questions about your surgeon’s experience with the specific technique, and ensure a robust post-operative plan is in place. Furthermore, if you are considering travel for care, research the credentials and success rates meticulously. For more detailed information on procedures, recovery, or to connect with specialists, visit our comprehensive resources at WMEDTOUR.